Some frequently experienced symptoms include:
- Painful sensations such as burning, itching, or aching in the penis, testicles, perineum, or anal region
- Symptoms aggravated by sitting too long, certain clothing, or physical activities
- Urinary challenges, including an urgent need to go, frequent urination, or a weak urinary stream
- Painful ejaculation or post-ejaculatory discomfort focused in the pelvic area
- Erectile function issues, such as difficulty maintaining an erection or weaker ejaculation
- Gastrointestinal problems like bloating or constipation that may coincide with pelvic pain
- Episodes of discomfort that worsen after certain triggers or appear without clear explanation
- Symptoms that fluctuate, with better days and flare-ups coming and going
For those in the Burbank area, turning to pelvic floor physical and occupational therapy can provide the specialized care needed to get lasting relief and restore quality of life.
Some frequently experienced symptoms include:
- Painful sensations such as burning, itching, or aching in the penis, testicles, perineum, or anal region
- Symptoms aggravated by sitting too long, certain clothing, or physical activities
- Urinary challenges, including an urgent need to go, frequent urination, or a weak urinary stream
- Painful ejaculation or post-ejaculatory discomfort focused in the pelvic area
- Erectile function issues, such as difficulty maintaining an erection or weaker ejaculation
- Gastrointestinal problems like bloating or constipation that may coincide with pelvic pain
- Episodes of discomfort that worsen after certain triggers or appear without clear explanation
- Symptoms that fluctuate, with better days and flare-ups coming and going
For those in the Burbank area, turning to pelvic floor physical and occupational therapy can provide the specialized care needed to get lasting relief and restore quality of life.
Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

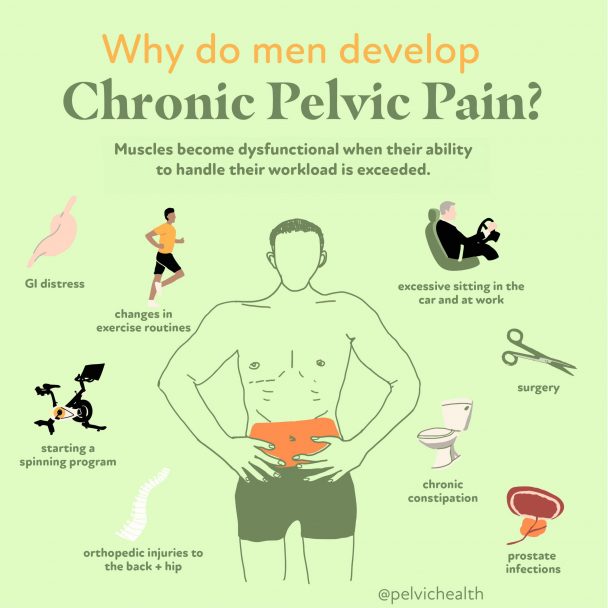
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction

Causes of Pelvic Pain
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction
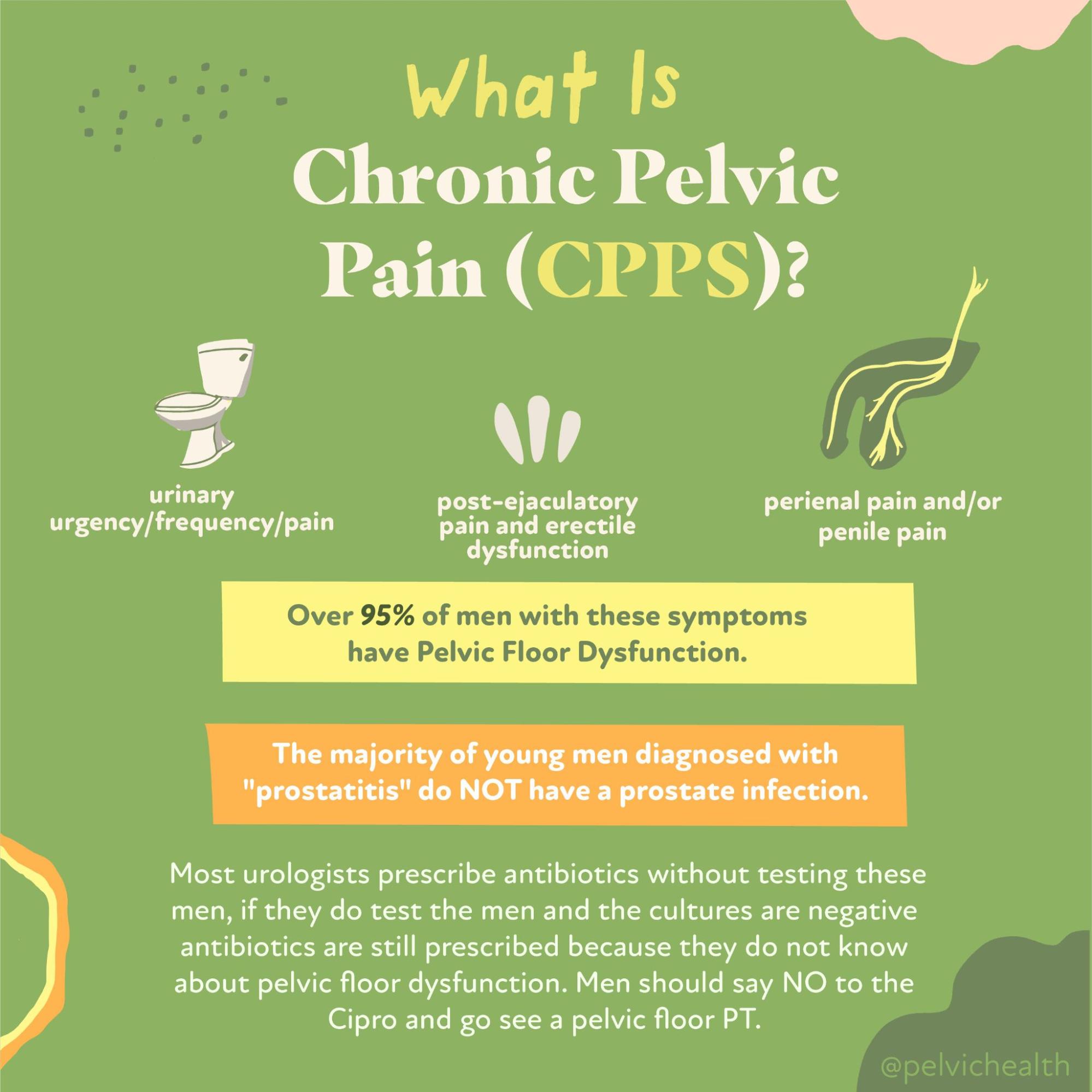
Diagnostic Challenges
Men dealing with pelvic pain are often misdiagnosed or left undiagnosed for extended periods—sometimes even years. Research has found it can take up to seven years before an accurate diagnosis is made. This significant delay is largely because male pelvic pain symptoms often resemble conditions like prostatitis, bladder infections, or STIs. Many providers opt for a quick fix by prescribing antibiotics, skipping the diagnostic testing that would rule out infection. Unfortunately, this common approach fails to uncover the true problem: dysfunction of the pelvic floor. Another barrier men face is the limited number of physical and occupational therapistss trained specifically in male pelvic health, as most are oriented toward female patients. At PHRC, however, we understand the complexity of male pelvic pain and have built a practice where men receive the care and expertise they deserve—often making up the majority of our client base.
For many men, a diagnosis of “prostatitis” often leads to ineffective treatments and prolonged frustration. The standard course of antibiotics may be prescribed under the assumption of infection, but research clearly reveals that in more than 90% of these cases, no bacterial infection is present. Rather than fighting an infection, these men are frequently dealing with Chronic Pelvic Pain Syndrome (CPPS), particularly in forms classified as NIH Categories IIIa or IIIb. These are non-bacterial conditions involving muscle dysfunction or nerve irritation—not something antibiotics can fix.
According to the National Institutes of Health, prostatitis syndromes are divided as follows:
Category I: Acute bacterial prostatitis – includes severe pelvic pain, systemic symptoms like fever, and confirmed acute urinary infection.
Category II: Chronic bacterial prostatitis – usually includes repeated urinary tract infections and bacteria residing long-term in the prostate.
Category IIIa: Inflammatory CPPS – characterized by immune cells (white blood cells) in reproductive or urinary secretions, indicating chronic inflammation.
Category IIIb: Non-inflammatory CPPS – shows similar pelvic pain symptoms but lacks white blood cells, making inflammation undetectable in lab work.
Category IV: Asymptomatic inflammatory prostatitis – inflammation found during routine testing despite the absence of any symptoms reported by the patient.
Diagnostic Challenges
Men dealing with pelvic pain are often misdiagnosed or left undiagnosed for extended periods—sometimes even years. Research has found it can take up to seven years before an accurate diagnosis is made. This significant delay is largely because male pelvic pain symptoms often resemble conditions like prostatitis, bladder infections, or STIs. Many providers opt for a quick fix by prescribing antibiotics, skipping the diagnostic testing that would rule out infection. Unfortunately, this common approach fails to uncover the true problem: dysfunction of the pelvic floor. Another barrier men face is the limited number of physical and occupational therapistss trained specifically in male pelvic health, as most are oriented toward female patients. At PHRC, however, we understand the complexity of male pelvic pain and have built a practice where men receive the care and expertise they deserve—often making up the majority of our client base.
For many men, a diagnosis of “prostatitis” often leads to ineffective treatments and prolonged frustration. The standard course of antibiotics may be prescribed under the assumption of infection, but research clearly reveals that in more than 90% of these cases, no bacterial infection is present. Rather than fighting an infection, these men are frequently dealing with Chronic Pelvic Pain Syndrome (CPPS), particularly in forms classified as NIH Categories IIIa or IIIb. These are non-bacterial conditions involving muscle dysfunction or nerve irritation—not something antibiotics can fix.
According to the National Institutes of Health, prostatitis syndromes are divided as follows:
Category I: Acute bacterial prostatitis – includes severe pelvic pain, systemic symptoms like fever, and confirmed acute urinary infection.
Category II: Chronic bacterial prostatitis – usually includes repeated urinary tract infections and bacteria residing long-term in the prostate.
Category IIIa: Inflammatory CPPS – characterized by immune cells (white blood cells) in reproductive or urinary secretions, indicating chronic inflammation.
Category IIIb: Non-inflammatory CPPS – shows similar pelvic pain symptoms but lacks white blood cells, making inflammation undetectable in lab work.
Category IV: Asymptomatic inflammatory prostatitis – inflammation found during routine testing despite the absence of any symptoms reported by the patient.
Treatment:
How We Can Help You

Men in Burbank who experience ongoing pelvic pain often benefit from a comprehensive evaluation by a pelvic floor physical and occupational therapists. This initial consultation is designed to uncover the root cause of your symptoms and provide a clear path forward. The therapist will take time to fully understand your personal medical background, what you’ve already been diagnosed with, what treatments you’ve tried, and how successful—or frustrating—those treatments have been. We know that by the time many Burbank residents reach us, they’re tired of not having answers.
The examination involves assessing the muscles of the pelvic floor, the integrity of nearby soft tissues, any joint imbalances, nerve sensitivities, and how your body moves during certain motions. After this hands-on evaluation, your therapist will review the results with you in detail and craft a personalized treatment plan. Most individuals attend physical and occupational therapy once or twice per week for approximately 12 weeks, supplemented with a home program to extend your progress. The therapist will coordinate care with any other specialists involved in your case. In Burbank, we’re dedicated to helping you move toward a pain-free and more functional life.

Treatment:
How We Can Help You
Men in Burbank who experience ongoing pelvic pain often benefit from a comprehensive evaluation by a pelvic floor physical and occupational therapists. This initial consultation is designed to uncover the root cause of your symptoms and provide a clear path forward. The therapist will take time to fully understand your personal medical background, what you’ve already been diagnosed with, what treatments you’ve tried, and how successful—or frustrating—those treatments have been. We know that by the time many Burbank residents reach us, they’re tired of not having answers.
The examination involves assessing the muscles of the pelvic floor, the integrity of nearby soft tissues, any joint imbalances, nerve sensitivities, and how your body moves during certain motions. After this hands-on evaluation, your therapist will review the results with you in detail and craft a personalized treatment plan. Most individuals attend physical and occupational therapy once or twice per week for approximately 12 weeks, supplemented with a home program to extend your progress. The therapist will coordinate care with any other specialists involved in your case. In Burbank, we’re dedicated to helping you move toward a pain-free and more functional life.
How Can We Help You?
We welcome you to contact us through the form below if you have any inquiries or feedback. Including your email address is important so that we can get back to you promptly. You can trust that your personal information will be kept completely private and used solely for communication purposes related to your message.

Join The Newsletter. Win a copy of our book, “Pelvic Pain Explained!”
We love getting to know our website visitors. Please tell us a little bit about yourself and get the latest info via PHRC e-newsletter!
*Subscribers automatically eligible to win our book, “Pelvic Pain Explained.”
Pelvic Pain Explained is a comprehensive look at the experiences of those dealing with persistent pelvic pain. It walks readers through the long and often discouraging road to diagnosis, explores the barriers to effective treatment, and highlights the struggle of navigating conflicting information about care options. Beyond the medical journey, it emphasizes the unseen toll this condition takes on a person’s emotional well-being, day-to-day functioning, and relationships with others.


