
If you’re a man in Burbank who’s been living with pelvic pain, urinary irritation, or ongoing sexual discomfort, you are far from alone. These symptoms are often linked to chronic prostatitis, or what’s medically called Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS). It’s a condition that can impact men at any stage of life, and statistics show that roughly 10% of men will face prostatitis-like symptoms at some point.
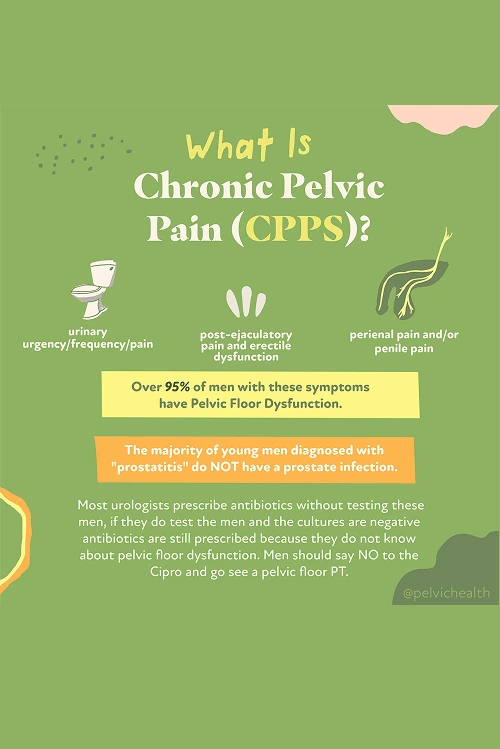
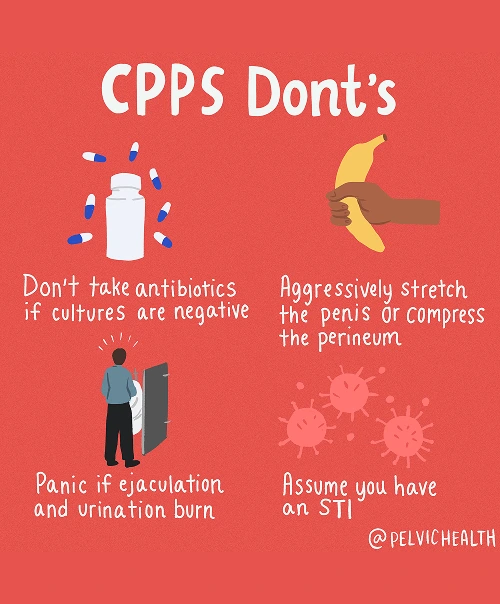
Interestingly, about 97% of men who receive a diagnosis of prostatitis do not actually have an infection in their prostate or bladder, even though antibiotics are frequently prescribed. In reality, for most men, the source of the problem is the pelvic floor muscles. When these muscles become overly tight, strained, or lose coordination, they can create symptoms that are nearly identical to a prostate infection.
For men in Burbank seeking long-term relief, pelvic floor physical and occupational therapy at PHRC can make a significant difference. Our skilled pelvic floor physical and occupational therapists focus on correcting muscle imbalances, restoring flexibility, and releasing tension. By targeting the true muscular causes of your discomfort, we help you regain comfort, confidence, and quality of life.
What are the Causes of Chronic Pelvic Pain Syndrome in Men?
For most men, Chronic Pelvic Pain Syndrome is not caused by a bacterial infection in the prostate, despite what they may have been told. Instead, multiple factors, primarily related to the way the pelvic floor interacts with other bodily systems, are typically involved.
- Lumbar pathology: The nerves supplying the pelvic region originate in the lower back. If a disc bulges, spinal arthritis develops, or a lumbar nerve becomes irritated, the pain may radiate forward into the pelvis and feel like prostate discomfort, even when the spine is the real source.
- Vascular pathology: Circulatory issues in the pelvis, such as enlarged veins, pelvic venous congestion, or changes in blood flow, can cause a sense of heaviness, pressure, or aching that closely resembles prostate pain.
- Pelvic floor pathology: The pelvic floor muscles form a hammock beneath the pelvis. When they become tight, spasm, or lose proper coordination, they can irritate nerves and produce pain that seems to arise from the prostate or bladder, but in reality, the muscles themselves are frequently the main source.
Other contributing factors can include:
- Past surgeries such as vasectomy or prostate procedures
- Structural issues like hip dysfunction, scoliosis, or leg length differences
- Excessive or sudden changes in exercise
- Long hours of sitting
- Chronic constipation or frequent straining
- Trauma or stress to the pelvic area
Even though several elements might influence symptoms, research shows that most men with chronic pelvic pain and urinary or digestive complaints have underlying pelvic floor muscle dysfunction.
Symptoms of Chronic Pelvic Pain Syndrome
The symptoms that accompany CPPS are often confusing because they feel identical to prostate or bladder problems, even though they may actually originate from muscle dysfunction in the pelvic floor. Common experiences among men with CPPS include:
- Aching, pressure, or sharp pain in the perineum, pubic area, or lower abdomen
- Discomfort that feels like it’s coming from the testicles, tip of the penis, or inside the urethra
- Urgency, frequency, weak stream, or the sensation that you can’t fully empty your bladder
- Burning or stinging, even when no infection is present
- Pain with or after ejaculation, erectile discomfort, or reduced sexual satisfaction
- Tightness or aching that overlaps with pelvic discomfort
- A sense of heaviness, pressure, or tight muscles in the pelvic floor area
Associated Diagnoses
Chronic pelvic pain affecting men can have several underlying causes recognized by medical professionals. These may involve spinal alignment, blood vessel function, or muscular control within the pelvic floor.
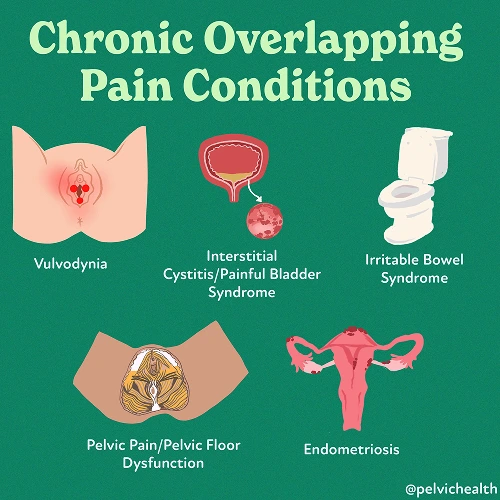
Low back disorders, including lumbar nerve irritation, degenerative disc disease, or arthritis, can trigger nerve pain that extends into the pelvic region and mimics prostate discomfort. Problems such as varicocele, twisted testicles, or pelvic vein congestion can reduce circulation and result in aching, pressure, or pulsating pain. While Chronic Pelvic Pain Syndrome is the condition most often seen, pelvic floor dysfunction can occur alongside issues such as pudendal neuralgia, bladder pain syndrome, or hard flaccid syndrome.
Often, it is the pelvic floor dysfunction itself that serves as the link, causing pain directly or worsening symptoms from other contributing systems.
Diagnostic Challenges
For many men, one of the greatest challenges with CPPS is the confusion surrounding diagnosis. It’s very common to be told the problem is prostatitis and to be prescribed antibiotics, even when there is no infection involved. Studies reveal that more than 90% of men who experience pain in the pelvic or urogenital area do not have bacterial prostatitis at all.
Instead, the majority belong to the Category III group identified by the National Institutes of Health (NIH), which covers chronic pelvic pain conditions. The NIH prostatitis classification includes:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Instead, the majority belong to the Category III group identified by the National Institutes of Health (NIH), which covers chronic pelvic pain conditions. The NIH prostatitis classification includes:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
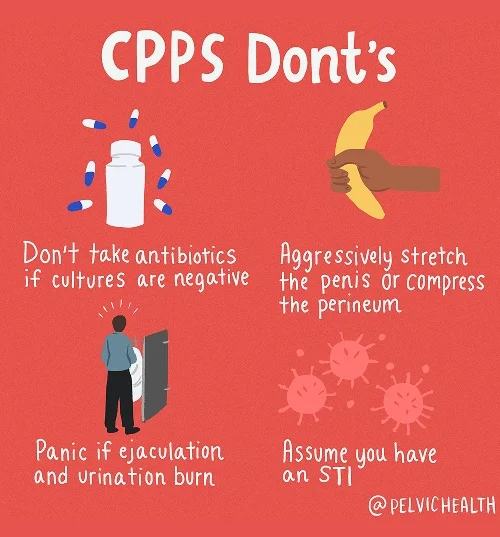
Because lower back and blood flow issues can create pain patterns that mirror those of pelvic floor dysfunction, it’s common for standard medical tests to appear normal. Unfortunately, this leads many men to feel stuck without a diagnosis. The overlap in symptoms causes delays in proper care, sending men through cycles of unnecessary antibiotics and endless referrals. Real improvement often starts when pelvic floor physical and occupational therapy identifies and treats the true muscular and nerve-related cause.
Symptoms of Chronic Pelvic Pain Syndrome
Because CPPS is rarely connected to infection, the pathway to healing doesn’t rely on antibiotics. Instead, the goal is to retrain and rebalance the pelvic floor while addressing related systems that may be heightening pain or tension.
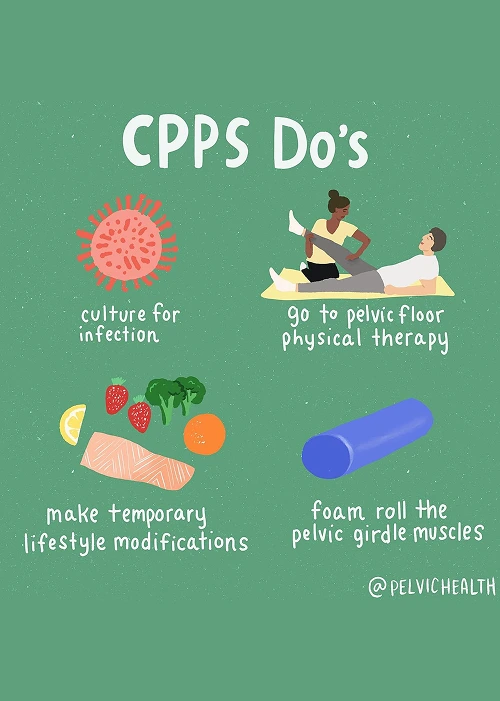
- Pelvic floor physical and occupational therapy: This is the cornerstone of care for men experiencing CPPS. The therapy works by reducing tension in the pelvic floor muscles, improving coordination, and soothing irritated nerves that trigger ongoing discomfort.
- Spine and back treatment: If the source of pain is linked to the lower spine, your therapist will address posture and movement mechanics to reduce irritation. Physicians may occasionally recommend injections to support this process.
- Vascular-related treatment: Circulatory problems can worsen symptoms, so pelvic floor therapy emphasizes improved posture and breathing to encourage better blood flow and ease congestion in the pelvic veins.
- Biomechanical support: Evaluating hip mobility and alignment can make a significant difference. Correcting imbalances reduces the overall strain on your pelvic region and allows for smoother movement.
- Lifestyle adjustments: Practical steps like avoiding excessive sitting, maintaining good bowel habits, and slowly reintroducing activity can make day-to-day life much more comfortable.
How We Can Help with Your Chronic Pelvic Pain
Many men in Burbank dealing with chronic pelvic pain find themselves stuck in a frustrating cycle of trial and error. You might have gone from doctor to doctor, taken multiple antibiotics, or received conflicting opinions, yet still face symptoms that disrupt your daily life. At PHRC, we understand how discouraging this can be, which is why we offer focused evaluations with pelvic floor physical and occupational therapists who specialize in men’s pelvic health.
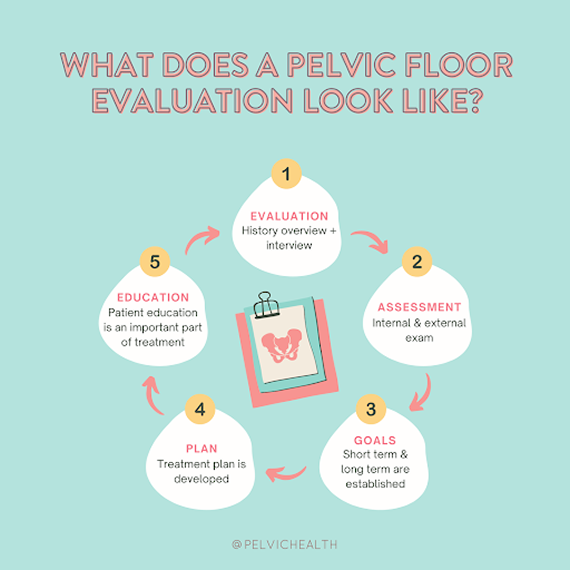
When you visit our clinic, your evaluation will begin with an in-depth conversation about your medical history, symptoms, past diagnoses, and previous treatments. We’ll take the time to understand how those approaches have worked or haven’t worked for you. This process helps us identify patterns and pinpoint potential causes that may have been overlooked before.
We also know how exhausting it can be to keep searching for answers, so we make sure you feel truly heard and supported from start to finish.
How We Can Help with Your Chronic Pelvic Pain
Many men in Burbank dealing with chronic pelvic pain find themselves stuck in a frustrating cycle of trial and error. You might have gone from doctor to doctor, taken multiple antibiotics, or received conflicting opinions, yet still face symptoms that disrupt your daily life. At PHRC, we understand how discouraging this can be, which is why we offer focused evaluations with pelvic floor physical and occupational therapists who specialize in men’s pelvic health.
When you visit our clinic, your evaluation will begin with an in-depth conversation about your medical history, symptoms, past diagnoses, and previous treatments. We’ll take the time to understand how those approaches have worked or haven’t worked for you. This process helps us identify patterns and pinpoint potential causes that may have been overlooked before.
We also know how exhausting it can be to keep searching for answers, so we make sure you feel truly heard and supported from start to finish.
During your physical exam, your PHRC therapist will assess the muscles, joints, nerves, and connective tissues of your pelvic region. Once the evaluation is complete, we’ll review our findings with you and explain how your pain developed. Together, we’ll design a personalized plan that outlines short- and long-term goals tailored to your recovery.
Typically, your treatment will include one to two therapy sessions per week for about twelve weeks, along with a home exercise program designed to support your progress. Your PHRC therapist will coordinate your care with your other healthcare professionals to ensure a complete, team-based approach. Our mission is to help you overcome chronic pain and regain a better quality of life.
