
If you are a male Culver City resident dealing with ongoing pelvic discomfort, painful urination, or sexual issues that linger, you are not the only one. Many men encounter these same concerns, which are frequently caused by a condition called chronic prostatitis, or Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS). Approximately one in ten men will experience these symptoms at some point in their lives.
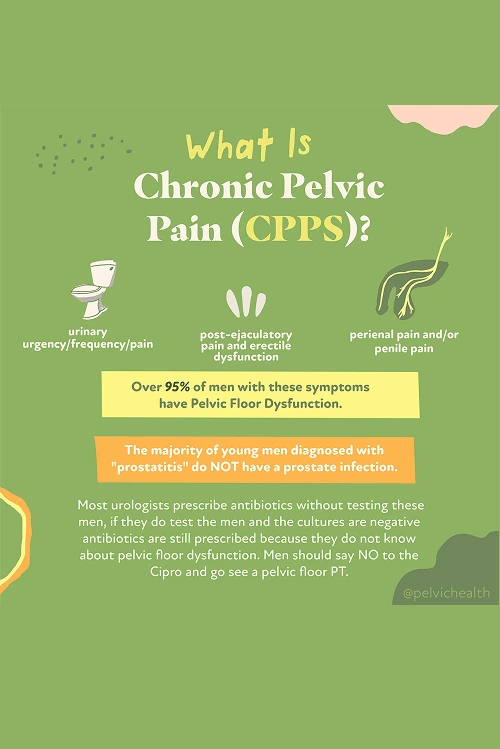
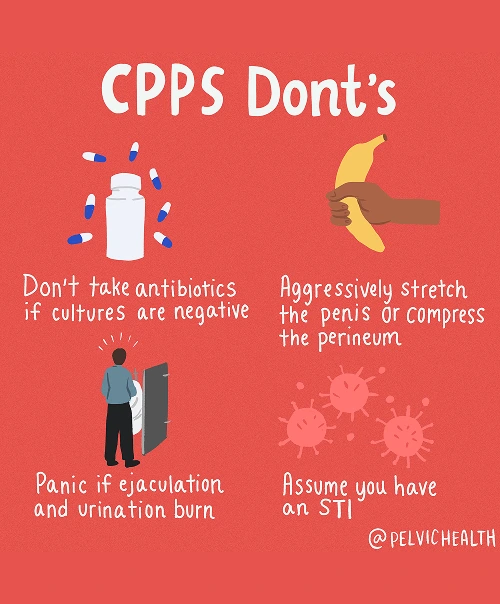
Research has revealed that about 97% of men with these symptoms do not actually have a prostate or bladder infection, despite the frequent use of antibiotics. The true source of the discomfort usually lies in the pelvic floor muscles. Tight, inflamed, or uncoordinated muscles in this area can mimic the sensations of a prostate problem.
For men in Culver City experiencing these challenges, PHRC’s pelvic floor and occupational therapy provides hope and relief. Our dedicated therapists focus on easing muscle tension, restoring proper function, and improving pelvic mobility. By addressing the root muscular causes, our goal is to help men achieve lasting comfort and better daily living.
What are the Causes of Chronic Pelvic Pain Syndrome in Men?
Chronic Pelvic Pain Syndrome does not usually come from a prostate infection, even though men are often told otherwise. The primary contributors often involve the pelvic floor and its connections with other bodily systems.
- Lumbar pathology: Nerves serving the pelvis start in the lower spine. Spinal issues such as disc bulges, arthritis, or nerve irritation can send pain forward into the pelvic area, mimicking prostate discomfort.
- Vascular pathology: Problems with circulation, such as varicoceles or pelvic venous congestion, can produce sensations of pressure, heaviness, or aching that feel like prostate pain.
- Pelvic floor pathology: The pelvic floor muscles provide support under the pelvis. When these muscles spasm, tighten, or fail to coordinate properly, they can irritate nerves and produce symptoms that feel like they originate from the prostate or bladder, while the muscles themselves are often the root cause.
Other contributing factors may include:
- Past surgeries such as vasectomy or prostate procedures
- Structural issues like hip dysfunction, scoliosis, or leg length differences
- Excessive or sudden changes in exercise
- Long hours of sitting
- Chronic constipation or frequent straining
- Trauma or stress to the pelvic area
Even though many factors can worsen chronic pelvic pain, most men, especially those with urinary or bowel difficulties, have an underlying problem rooted in pelvic floor dysfunction.
Symptoms of Chronic Pelvic Pain Syndrome
CPPS can be tricky to identify because the symptoms often resemble prostate or bladder issues even though the real source is in the pelvic floor muscles. Men may notice:
- Aching, pressure, or sharp discomfort in the pubic region, perineum, or lower abdomen
- Sensations that feel as if they are coming from the tip of the penis, urethra, or testicles
- Urgent or frequent urination, weak stream, or feeling unable to empty the bladder completely
- Burning or stinging without a present infection
- Pain during or after ejaculation, erectile challenges, or reduced sexual satisfaction
- Tight or aching pelvic muscles that overlap with general pelvic discomfort
- A sense of pressure, heaviness, or tension in the pelvic floor
Associated Diagnoses
Chronic pelvic pain among men can be linked to a variety of well-documented medical issues. Some of these arise from the spine, others from the vascular system, and many involve the pelvic floor muscles.
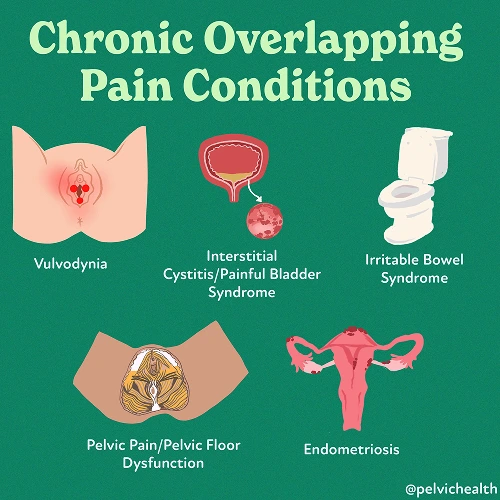
Spinal problems, including nerve compression in the lumbar region, degenerative disc disease, or arthritis, can affect nerves that run into the pelvic area. These nerve-related issues can feel remarkably similar to prostate pain. Circulatory problems such as varicoceles, pelvic venous congestion, or testicular complications can create sensations of heaviness, aching, or sharp stinging. While Chronic Pelvic Pain Syndrome is most commonly identified, pelvic floor dysfunction often co-occurs with pudendal neuralgia, painful bladder syndrome, or hard flaccid syndrome.
In a significant number of cases, dysfunction in the pelvic floor becomes the primary factor. It can directly generate pain or intensify discomfort stemming from spinal or vascular conditions, making treatment of the muscles essential for relief.
Diagnostic Challenges
Many men living with CPPS go through years of confusion before receiving the correct diagnosis. It is frequent for physicians to diagnose prostatitis and treat with antibiotics, even when infection tests return negative. Research has shown that roughly 90 percent of men with pelvic or urogenital pain do not have a true bacterial infection of the prostate.
According to the NIH prostatitis classification, most men with these symptoms fall under Category III. The NIH identifies five main categories:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
According to the NIH prostatitis classification, most men with these symptoms fall under Category III. The NIH identifies five main categories:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
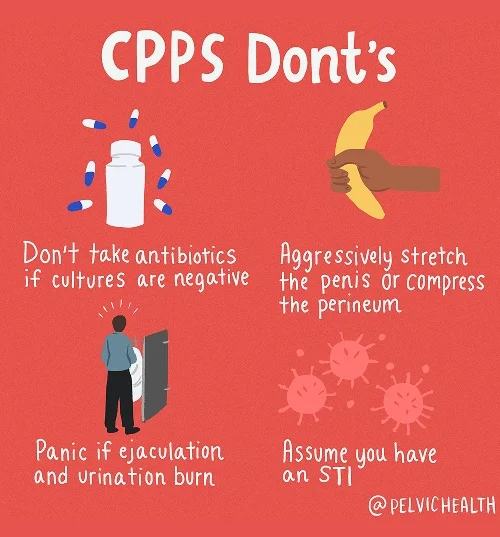
It is common for men experiencing pelvic floor pain to receive normal test results even though they continue to suffer. Conditions affecting the spine or blood vessels can create sensations that mimic pelvic floor discomfort. Without an accurate diagnosis, many men are sent from one specialist to another and prescribed antibiotics that provide no real relief. Pelvic floor therapy, both physical and occupational, helps patients target the true cause of their symptoms, promoting lasting improvement in comfort and daily function.
Symptoms of Chronic Pelvic Pain Syndrome
Since infections are rarely the root cause of CPPS, treatment focuses on restoring balance, improving pelvic floor function, and addressing other contributing physical factors instead of using antibiotics. The aim is to calm irritated nerves and normalize the pelvic region to relieve persistent pain.
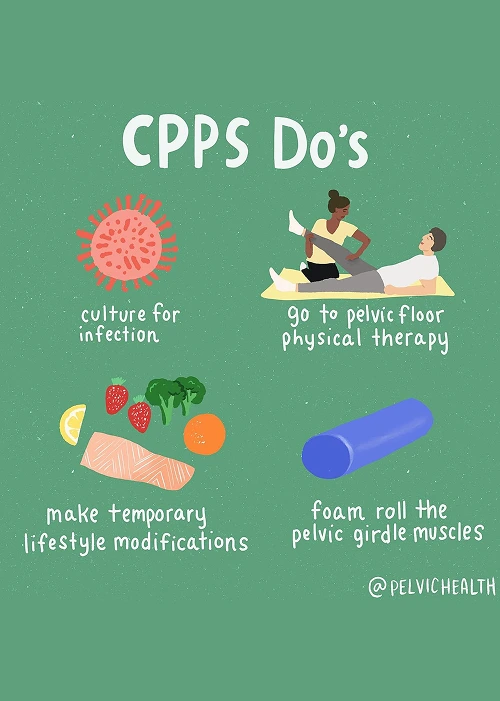
- Pelvic floor physical and occupational therapy: This treatment is the cornerstone of care. Techniques involve releasing tension in the muscles, retraining coordination, and soothing nerve irritation to help men regain comfort and function.
- Spine and back treatment: Issues in the lower back or sciatic nerves often contribute to pelvic pain. Interventions focus on improving posture, spinal alignment, and mobility, and physicians may add anti-inflammatory injections when necessary.
- Vascular-related treatment: Circulatory disturbances can increase discomfort. Breathing exercises, relaxation techniques, and postural correction during therapy improve blood flow and alleviate vascular tension.
- Biomechanical support: Proper alignment and movement patterns in the pelvis and hips reduce uneven pressure and minimize additional strain on the pelvic floor.
- Lifestyle adjustments: Gentle movement, sitting less, and managing bowel function are practical daily changes that can make a noticeable difference in symptom severity.
How We Can Help with Your Chronic Pelvic Pain
For men in Culver City struggling with chronic pelvic discomfort, the road to recovery can feel overwhelming. Many have tried antibiotics, sought multiple medical opinions, and yet continue to experience persistent symptoms. At PHRC, our pelvic floor physical and occupational therapists specialize in men’s pelvic health to provide focused and effective evaluations.
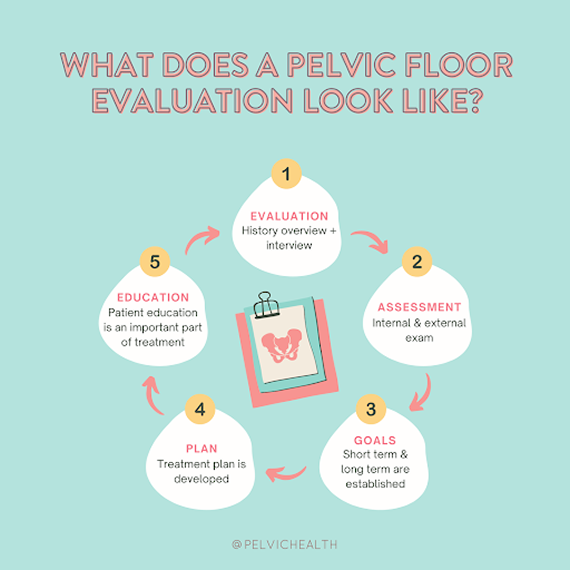
Your evaluation begins with a thorough conversation about your current symptoms, medical history, and prior treatment efforts. We aim to understand how these challenges impact your daily life, work performance, and personal relationships. Our approach emphasizes patience, empathy, and open communication to help you feel supported.
How We Can Help with Your Chronic Pelvic Pain
For men in Culver City struggling with chronic pelvic discomfort, the road to recovery can feel overwhelming. Many have tried antibiotics, sought multiple medical opinions, and yet continue to experience persistent symptoms. At PHRC, our pelvic floor physical and occupational therapists specialize in men’s pelvic health to provide focused and effective evaluations.
Your evaluation begins with a thorough conversation about your current symptoms, medical history, and prior treatment efforts. We aim to understand how these challenges impact your daily life, work performance, and personal relationships. Our approach emphasizes patience, empathy, and open communication to help you feel supported.
During the physical assessment, your therapist evaluates the pelvic floor muscles, nerves, connective tissues, and overall movement patterns. Once the evaluation is complete, findings are shared and discussed to help you understand the underlying causes of your pain. Together, we design an individualized plan to address both immediate symptom relief and long-term functional improvement.
Therapy is commonly scheduled once or twice per week for twelve weeks and complemented with a personalized home exercise program. Your PHRC therapist also coordinates with other healthcare providers as part of a comprehensive approach. Our goal is to empower men in Culver City to regain control, reduce pain, and restore confidence in everyday activities.
