
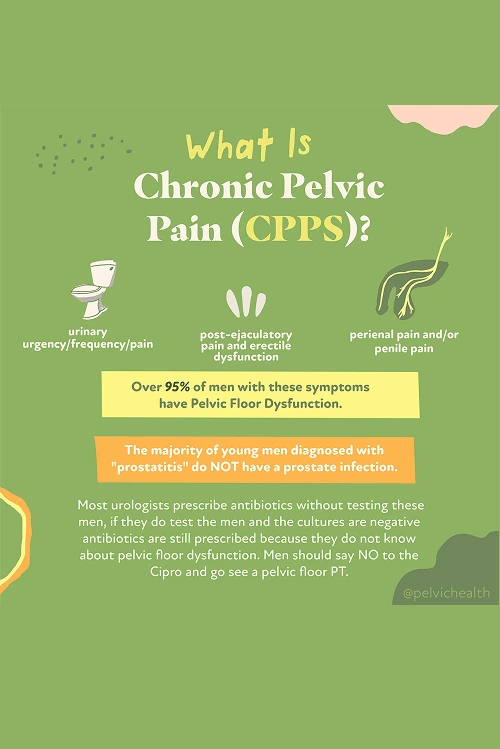
Men living in Encino who face chronic pelvic pain, discomfort while urinating, or persistent sexual difficulties often find these issues difficult to manage. Such symptoms are commonly associated with chronic prostatitis, also known as Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS), which affects roughly 10% of men during their lifetime.
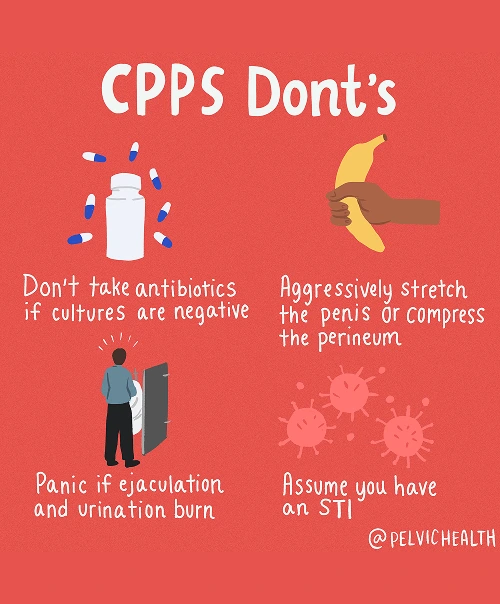
Studies have shown that around 97% of men with these symptoms do not have an actual prostate or bladder infection, even though antibiotics are often prescribed. The underlying source of the pain usually originates in the pelvic floor muscles. Tightness, inflammation, or lack of coordination in these muscles can generate the same sensations typically attributed to prostate conditions.
For men in Encino seeking relief, pelvic floor and occupational therapy at PHRC provides an effective approach. Our team of physical and occupational therapists specializes in reducing muscle tension, restoring pelvic function, and improving overall mobility. By addressing the underlying muscular dysfunction rather than just the symptoms, we help men regain lasting comfort and better quality of life.
What are the Causes of Chronic Pelvic Pain Syndrome in Men?
Chronic Pelvic Pain Syndrome is rarely due to an actual prostate infection, even though men are frequently told antibiotics will help. Most pain originates from pelvic floor dysfunction and other related physiological factors.
-
- Lumbar pathology: Nerves from the lower back serve the pelvis. Herniated discs, spinal arthritis, or nerve inflammation can radiate pain into the pelvic region, causing sensations that mimic prostate discomfort.
- Vascular pathology:Circulatory disruptions such as pelvic venous congestion or varicoceles can result in heaviness, aching, or pressure that is often misinterpreted as coming from the prostate.
- Pelvic floor pathology: The pelvic floor muscles act as a supportive hammock beneath the pelvis. Muscle tightness, spasms, or uncoordinated contraction can irritate nerves and create pain that feels like it originates from the prostate or bladder, though the muscles themselves are typically responsible.
Other contributing factors may include:
- Past surgeries such as vasectomy or prostate procedures
- Structural issues like hip dysfunction, scoliosis, or leg length differences
- Excessive or sudden changes in exercise
- Long hours of sitting
- Chronic constipation or frequent straining
- Trauma or stress to the pelvic area
Although various factors can aggravate chronic pelvic pain, most men, particularly those struggling with urinary or bowel problems, have a primary issue in the pelvic floor muscles.
Symptoms of Chronic Pelvic Pain Syndrome
CPPS can be tricky to identify because the symptoms often resemble prostate or bladder issues even though the real source is in the pelvic floor muscles. Men may notice:
- Pain, pressure, or aching in the perineum, pubic area, or lower abdomen
- Discomfort perceived in the urethra, testicles, or penis tip
- Frequent urges to urinate, weak stream, or incomplete bladder emptying
- Stinging or burning sensations without infection
- Pain with ejaculation, erectile discomfort, or reduced sexual satisfaction
- Aching or tightness in pelvic muscles
- Heaviness, tension, or pressure in the pelvic floor region
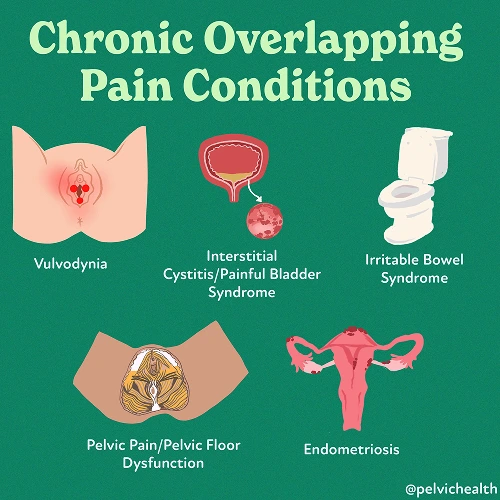
Associated Diagnoses
Men with chronic pelvic pain often have multiple potential medical contributors. Some causes are spinal in nature, others involve blood vessels, and many are rooted in pelvic floor muscle dysfunction.
Lower back concerns, such as lumbar nerve irritation, disc degeneration, or arthritis, can affect nerves traveling into the pelvis, producing sensations that are often mistaken for prostate pain. Vascular complications like varicoceles, pelvic venous congestion, or torsion of the testicles can disrupt circulation, causing dull, aching, or stinging pain. Although Chronic Pelvic Pain Syndrome is frequently diagnosed, pelvic floor dysfunction commonly appears alongside pudendal neuralgia, painful bladder syndrome, and hard flaccid syndrome.
In many men, pelvic floor muscle dysfunction is the unifying factor. It can either cause pain directly or worsen symptoms originating from spinal or vascular issues, emphasizing the need for treatment focused on the pelvic musculature.
Diagnostic Challenges
Men with chronic pelvic pain frequently experience years of uncertainty before finding the correct diagnosis. It is not unusual for them to be told they have prostatitis and to be prescribed antibiotics, even if tests show no infection. Studies report that over ninety percent of men with pelvic or urogenital pain do not have a bacterial infection in the prostate.
Most men with these complaints fall under Category III in the NIH prostatitis classification system. The five NIH categories are:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Most men with these complaints fall under Category III in the NIH prostatitis classification system. The five NIH categories are:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Men who have long-term pelvic pain often face frustration when standard medical tests do not reveal the cause. Spinal problems or circulatory issues can produce pain that feels as though it originates in the pelvic floor, leading to misdirected treatments. Many men end up visiting multiple healthcare providers and taking antibiotics that do not resolve the problem. Pelvic floor physical and occupational therapy addresses the root muscular and structural causes, providing a pathway to real relief and enhanced quality of life.
Symptoms of Chronic Pelvic Pain Syndrome
Because CPPS is usually not related to a prostate infection, effective treatment is focused on function, balance, and holistic care rather than prescribing antibiotics. The aim is to restore proper pelvic floor function, calm nerves, and address other bodily systems that may worsen pain or tension.
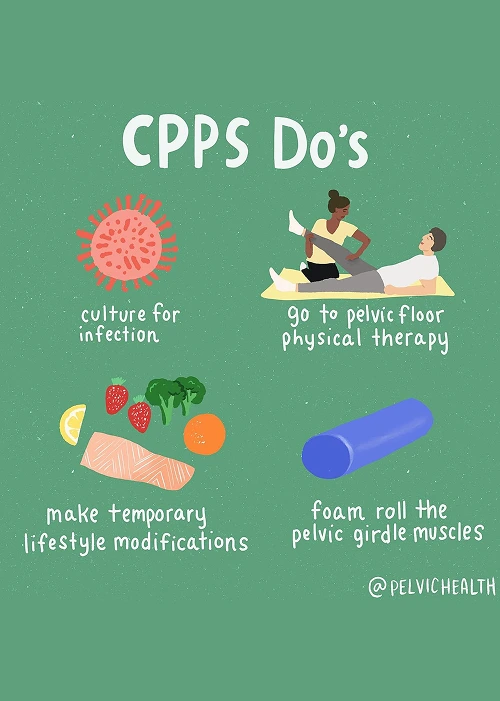
- Pelvic floor physical and occupational therapy: Central to treatment, these therapies release tight or spastic muscles, retrain movement patterns, and ease irritated nerves, providing relief and restoring daily comfort.
- Spine and back treatment: Discomfort stemming from the lower back or sciatic nerves requires interventions to improve posture, alignment, and mobility, sometimes supplemented with injections to reduce inflammation.
- Vascular-related treatment: Circulatory issues can amplify discomfort. Techniques such as controlled breathing, relaxation, and postural corrections during therapy enhance blood flow and reduce vein congestion.
- Biomechanical support: Adjusting hip and pelvic alignment and correcting movement restrictions ensures even distribution of pressure, reducing strain on the pelvic floor.
- Lifestyle adjustments:Simple changes, including limiting prolonged sitting, maintaining bowel health, and incorporating gentle movement, support symptom improvement and long-term wellness.
How We Can Help with Your Chronic Pelvic Pain
Chronic pelvic pain can create a challenging and discouraging experience for men in Encino. Many have undergone multiple courses of antibiotics, sought different opinions, and still struggle to find lasting relief. PHRC provides specialized evaluations conducted by pelvic floor physical and occupational therapists who are experts in men’s pelvic health.
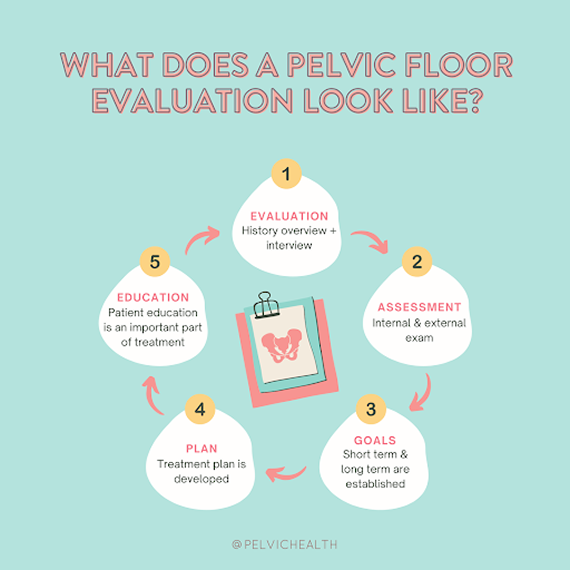
The process begins with an in-depth conversation about your symptoms, medical history, and treatments already attempted. Therapists take time to understand the impact of pain on your work, relationships, and daily routine. Compassion, patience, and clarity are central to our approach to make your experience supportive and informative.
How We Can Help with Your Chronic Pelvic Pain
Chronic pelvic pain can create a challenging and discouraging experience for men in Encino. Many have undergone multiple courses of antibiotics, sought different opinions, and still struggle to find lasting relief. PHRC provides specialized evaluations conducted by pelvic floor physical and occupational therapists who are experts in men’s pelvic health.
The process begins with an in-depth conversation about your symptoms, medical history, and treatments already attempted. Therapists take time to understand the impact of pain on your work, relationships, and daily routine. Compassion, patience, and clarity are central to our approach to make your experience supportive and informative.
During the evaluation, the therapist examines pelvic floor muscles, nerves, connective tissues, and movement patterns to pinpoint dysfunction. Afterward, findings are explained and a treatment plan is developed that addresses both immediate relief and long-term goals.
Therapy sessions are typically conducted one or two times per week for roughly twelve weeks and paired with a home exercise program tailored to your needs. Coordination with other healthcare professionals ensures a holistic treatment approach. Our mission is to help men in Encino regain comfort, functionality, and confidence.
