By Stephanie Prendergast, MPT, Cofounder, PHRC Los Angeles
Do you know the difference between vulvodynia & vestibulodynia? Vulvodynia simply means pain in the vulva, which includes the clitoris, labia, mons pubis, perineum, hymen, and vestibule.
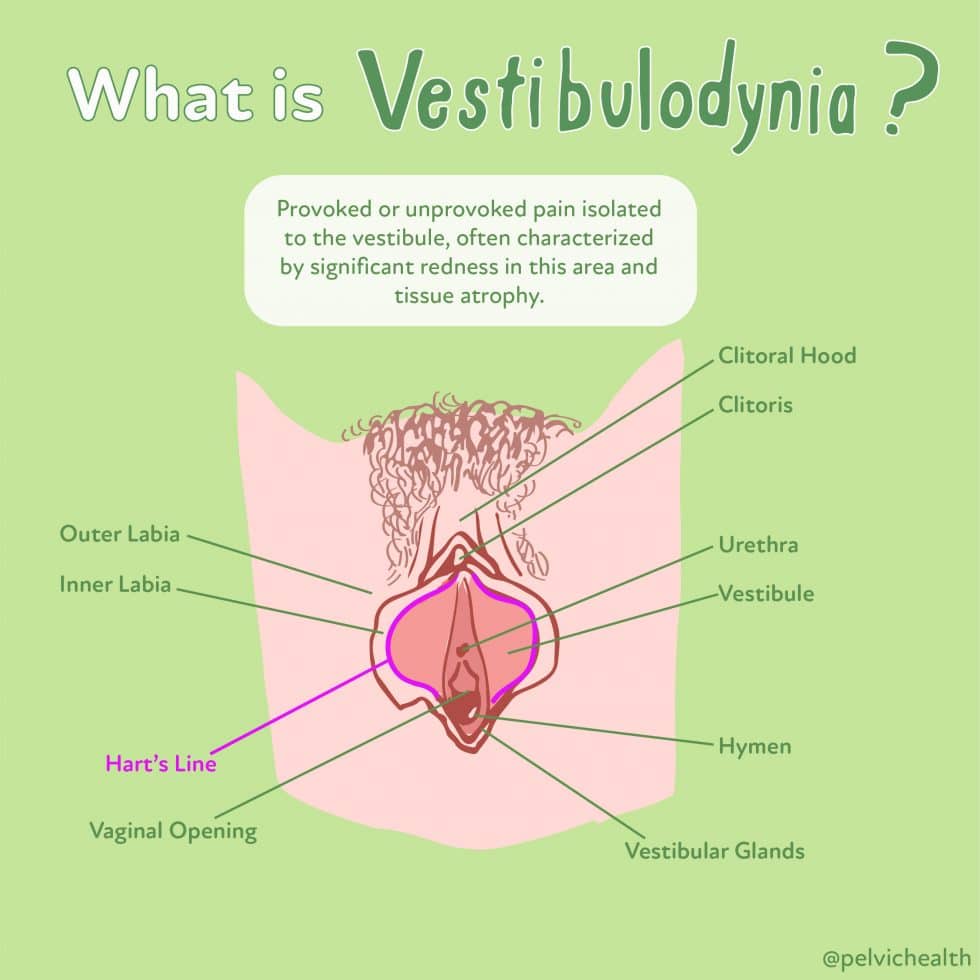
Vestibulodynia is pain in the vestibule, a more precise description for the area of pain. The vestibule is depicted in the picture above and extends from inside the labia minora to the hymen & houses the opening of the urethra and our major & minor glands that provide some of our lubrication when we are aroused.⠀
Understandably, most people with painful sex & vulvar pain may not know where the vestibule is unless they have seen vulvar expert who explains the differences. Importantly, the vestibule is anatomically different from the rest of the vulva.⠀Below are graphics depicting some of the most common causes and treatments for vestibulodynia. Following them are our most frequently asked questions on the topic with their answers!
Q: Can vestibulodynia happen just around the urethra? Is it frequent in pregnancy?
A: It is possible for someone to have vestibulodynia in just part of the vestibule, and that can be the area around the urethra. We see this sometimes when people aren’t applying their topical properly and ‘miss’ some areas. It also can simply develop there and not in the entire vestibule. It is not common for women to develop vestibulodynia in pregnancy per our clinical observations, I am not sure if this has been studied. Great questions!
Q: Spent a day reading about some updated guidelines – have you guys come across local diazepam suppositories much? They are recommended and yet doctors here do not prescribe much for muscular related vestibulodynia.
A: Several physicians in our area are prescribing these for patients, other doctors are not comfortable doing so. It is important to know that diazepam works on the central nervous system, regardless of how it gets into our bodies. It does not work ‘better’ on pelvic floor dysfunction if it is inserted in the vagina. Most people do not realize this. People sometimes report feeling ‘better’ with vaginal diazepam, this may be because it calms the nervous system versus relaxing the muscles. Multiple studies have shown that diazepam does not reduce painful muscles, lower muscle tone, or reduce pain with sex. Now with this said, some people do report improvement, we just want to be clear on what this drug does and does not do.
Q: How do you get diagnosed with vestibulodynia vs. vaginismus. How do you determine if you have both! What kind of specialist should you see if you have vestibulodynia? It seems like most gynos I have seen have no idea what it is. And curious about treatment options for sure.
A: Many gynecologists may be aware of vulvodynia but not how to treat it, and even fewer know and understand vestibulodynia. We recommend seeing a vulvar specialist, someone who intentionally has sought out additional course work around this topic. We suggest looking at their websites and many doctors who belong to the International Society for the Study of Women’s Health may know more than general gynecologists. They have a provider link on their website. Vestibulodynia is most simply defined as pain in the vestibule, usually with redness, that can be confirmed by visual inspection and a cotton swab test. Vaginismus refers to involuntary contraction of the pelvic floor muscles that interferes with penetration. It is possible to have vaginismus and NOT have vestibulodynia and vice versa. However, they can exist together too.
Q: Can pain manifest as itching?
A: Itching can be the symptom of an infection such as yeast, a disease such as lichen sclerosus, and it can also be a symptom of neuropathic pain. It is important to have a good differential diagnosis to understand what is causing it.
Q: Suggestions for calming a flare or symptoms?
A: Remind yourself that you have been through flares before and that they will not last forever. It is important to calm the nervous system via meditation and other calming strategies. Unfortunately without more information on the symptoms and cause I can’t suggest more than this.
Q: Can PFD with vulvodynia cause hemorrhoids?
A: The majority of people with vulvodynia have pelvic floor dysfunction, and pelvic floor dysfunction can alter bowel mechanics and result in straining during bowel movements which can lead to hemorrhoids.
Q: Why does PFD cause that burning feeling?
A: Unprovoked burning is more often caused by vestibulodynia than PFD, but it feels internal enough that people think the symptoms are coming from the vagina or pelvic floor muscles. However, if significant pelvic floor tightness is present and/or there is pudendal nerve irritation the muscles and nerve may create a burning sensation when touched.
Q: Can PT fix it completely?
A: Pelvic floor physical therapy can resolve musculoskeletal dysfunction completely. If a patient has hormonal insufficiencies, neuroproliferative vestibulodynia, lichen sclerosis or planus, or vaginal infections as contributing factors to their pain, PFPT alone will not be enough. Effective treatment will involve medical management and physical therapy and patients can do very well!
Q: Does weightlifting make it worse? If so, what can I do to continue being able to lift?
A: In general, weight lifting should be something that is good for us. However, when people have pelvic floor and girdle dysfunction weight lifting may exacerbate symptoms. When we do squats, lunges, or core work our pelvic floor muscles reflexively tighten to keep us continent. Under normal circumstances the muscles relax again afterwards. When people have pelvic floor dysfunction their muscles may remain contracted, or in spasm, after the activity stops and therefore they may experience symptoms. A general rule of thumb for strengthening is that people can resume doing this safely once they can control their pelvic floor muscles and the muscles can once again relax after activities that cause them to contract.
Q: How common it is for VVD to spread to the mons?
A: When left untreated it symptoms can advance and ‘spread’ to neighboring anatomy areas. I am not aware of any studies that discusses the prevalence of mons pubis pain specifically.
Q: Can I get steroid/trigger point injections for vestibulodynia?
A: Pelvic floor dysfunction is one cause vestibulodynia. Trigger point injections, with or without steroids, are a known and effective dysfunctional pelvic floor muscles, therefore, may help reduce the symptoms of vestibulodynia. We do not typically advise injecting the vestibule itself, it is better to treat the cause of the vestibulodynia which is rarely just ‘inflammation’.
Q: DR ruled out hormone mediated vestibulodynia w/o testing. How should I ask them to do testing?
A: Hormonally mediated vestibulodynia can be diagnosed with a combination of tests: lab work to identify low free testosterone and high SHBG, visual inspection of the vulva with vulvoscopy, and a cotton swab test to identify areas and severity of pain.
Q: Is provoked pain in the transverse perineal part of the vestibulodynia?
A: Most women with vestibulodynia have myalgia in the muscles of the urogenital triangle, the transverse perineal muscle is part of this muscle group. However, the muscles are not technically part of the vestibule itself.
Q: Possible medication that makes it bearable?
A: Several classes of medication can help reduce persistent pelvic pain: these include neuromodulators such as Neurontin and Lyrica, SNRIs such as Cymbalta and Effexor, and tricyclic antidepressants. More research studies show encouraging results with low-dose naltrexone. Pain management physicians can be a great resource to help control the pain as people are working to treat the underlying causes of pain.
Q:… vulvodynia?
A: Not everyone knows the difference between vulvodynia & vestibulodynia. Read a full description of the difference here. Vulvodynia simply means pain in the vulva, which includes the clitoris, labia, mons pubis, perineum, hymen, and vestibule. Vestibulodynia is pain in the vestibule, a more precise description for the area of pain. The vestibule is depicted in the picture above and extends from inside the labia minora to the hymen & houses the opening of the urethra and our major & minor glands that provide some of our lubrication when we are aroused.
Q: I experience pain in the vaginal orifice (upwards), but only during sex. May this also be vulvodynia?
A: This symptom is considered provoked vulvodynia, meaning it only occurs with physical contact.
Q: Can atrophy be repaired/healed?
A: Yes! Typical treatment involves medical management of hormone therapy with a physician.
Q: Do people get cured of vulvodynia? Been battling it a year now.
A: YES. Successful treatment involves identifying all underlying factors and treatment by both pelvic floor physical therapists and medical management with physicians.
Q: Best cure for vulvodynia?
A: This depends on the underlying causes, which can be multifactorial. Common causes include pelvic floor dysfunction, hormonal insufficiency, infections such as yeast and BV, diseases such as STIs and lichen sclerosus/planus, neuropathic such as pudendal neuralgia, and trauma from things like childbirth or pelvic reconstruction.
Q: What kind of test could doctor’s do on my clitoris to figure out why I cannot orgasm?
A: To my knowledge there is not a single ‘test’ that can be utilized. However, many women suffer from aorgasmia and a combination of medical management, sex therapy, and PFPT if there is muscles dysfunction or pelvic pain can help. We recommend the book Come as You Are to help people better understand their bodies. Many sex therapist’s offer online programs to help, we recommend checking out Dr. Erica Marchand’s program, you can find her on IG as @hertherapysecrets.
Q: Can you have vulvodynia without having the symptom of painful sex? I have the burning sensation off and on and I tend to try to have sex when it feels better and I am able to have it without pain.
A: Vulvodynia symptoms can be transient, especially if they are tied to hormonal insufficiency people may feel ‘better’ around ovulation and ‘worse’ the week before their periods because of hormone fluctuations resulting in a change in the symptoms.
Q: Why do I have vulvodynia flares while on my period?
A: Hormone insufficiencies around menses may result in an exacerbation of symptoms. Menstrual pads and tampons plus the fluid itself can be vulvar irritants.
Q: Can vulvodynia be brought on by hormonal imbalances- specifically because of birth control?
A: YUP. Numerous research studies have linked OCP use to vestibulodynia. One study followed 30 women once they started taking birth control. None of these women had pelvic pain prior to starting the pill. The women were evaluated using sexual functioning questionnaires, lab work, and a physical examination. After 3 months on the birth control pill many of them reported painful sex. Their blood work showed low free testosterone and high SHBG. Their clitoris and labia shrunk. Women need to be warned that this can happen, it does not happen to everyone but developing vulvodynia is a risk factor. Reference: https://pubmed.ncbi.nlm.nih.gov/22188640/
Q: Could hormonal IUD cause hormone imbalances leading to vestibular pain?
A: To my knowledge there has not been an association between hormonal IUDs and vestibular pain. The reason oral contraceptives can cause vulvar pain is because they can reduce our bioavailable testosterone. Hormonal IUDs do not reduce our testosterone levels.
Q: Thoughts on vaginismus diagnosis without pain with a speculum/tampon, but only with intercourse?
A: It is possible that dysfunction muscles can interfere with intercourse but not tampons or a speculum.
Q: Is the inflammation involved with vvd the same as systemic inflammation typical of obesity?
A: I am not aware of any studies about this.
Q: Is it okay to feel discomfort in the pelvic region when doing squats and lunges?
A: Symptoms are using a sign of faulty neuromuscular and we suggest seeing a PFPT for an evaluation.
How to find informed medical providers:
International Pelvic Pain Society Find a Provider
International Society for the Study of Women’s Sexual Health
American Physical Therapy Association’s Section on Women’s Health PT Locator
Herman and Wallace Find a Provider
Pelvic Guru Provider Directory
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual physical therapy appointments too!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical therapists committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical therapists, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical therapist who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
PHRC is also offering individualized movement sessions, hosted by Karah Charette, DPT. Karah is a pelvic floor physical therapist at the Berkeley and San Francisco locations. She is certified in classical mat and reformer Pilates, as well as a registered 200 hour Ashtanga Vinyasa yoga teacher. There are 30 min and 60 min sessions options where you can: (1) Consult on what type of Pilates or yoga class would be appropriate to participate in (2) Review ways to modify poses to fit your individual needs and (3) Create a synthesis of your home exercise program into a movement flow. To schedule a 1-on-1 appointment call us at (510) 922-9836
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Like us on Facebook,
Subscribe to our YouTube Channel,