
Many men do not realize that erectile dysfunction can come from pelvic floor dysfunction rather than a simple blood flow issue. The pelvic floor muscles play a major role in erections by supporting the base of the penis, guiding blood into the erectile tissues, and coordinating the muscles that maintain firmness. When these muscles become tight, weak, or uncoordinated, they can restrict blood flow, irritate nerves, and interfere with arousal and performance.
At PHRC, pelvic floor physical and occupational therapy can address these muscular patterns, improve coordination through the pelvis and core, and help restore the function needed for strong and reliable erections.
What Are the Causes of Erectile Dysfunction?
Erectile dysfunction has several potential contributors, and many of them involve the pelvic floor, circulation, and/or the nervous system. While ED is often assumed to be strictly vascular, a large number of men experience symptoms that stem from muscular and neuromuscular issues in the pelvic floor. The specific causes can include:
- Pelvic floor dysfunction: The pelvic floor muscles support the base of the penis and help pump and keep blood into the erectile tissues. When these muscles become overactive, tight, or in spasm, they can restrict circulation, create pain or numbness, and fail to keep blood in the erectile tissues. Weak or underactive muscles can also make it difficult to maintain an erection or complete ejaculation. Trigger points in the pelvic floor can also refer to discomfort in the penis, scrotum, perineum, or rectum.
- Lumbar or nerve-related causes: The nerves involved in erections start in the lower back and travel through the pelvis. When these nerves become irritated due to a disc issue, arthritis, or tension in surrounding muscles, men can experience difficulty achieving or maintaining an erection, along with pelvic or genital pain.
- Vascular factors: Changes in blood flow, such as vessel congestion or impaired circulation, can contribute to erectile difficulties. Pelvic floor tension often worsens these vascular patterns by compressing or constricting the surrounding tissues.
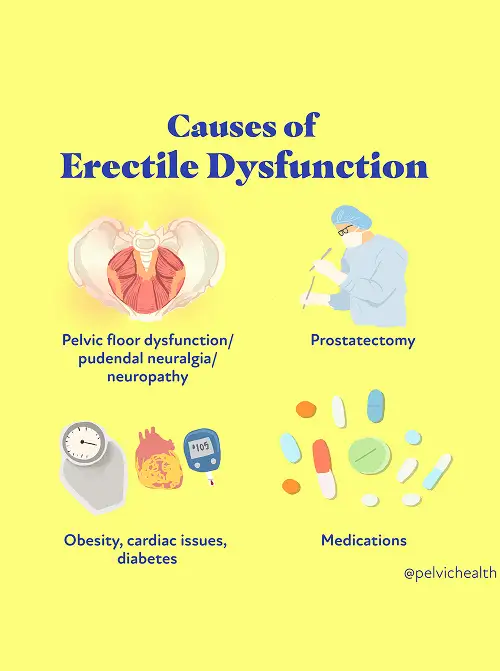
Additional contributors to erectile dysfunction can include:
- Surgical history involving the prostate, bladder, or pelvic organs
- Biomechanical or structural dysfunction in the hips, low back, or pelvis
- Excessive sitting or pressure on the pelvic floor
- High intensity exercise or abrupt changes in exercise routine
- Chronic constipation or straining
- Increased stress, anxiety, or nervous system activation
- Changes related to aging or other medical conditions
- Jelquing and penile enhancement devices
Most men with chronic pelvic or genital symptoms, with or without urinary or bowel complaints, also show signs of pelvic floor dysfunction.
Symptoms of Chronic Pelvic Pain Syndrome
Erectile dysfunction can appear in several ways, depending on whether the issue involves tight muscles, weak muscles, nerve irritation, or circulation. Men often report:
- Difficulty achieving a firm erection
- Trouble maintaining an erection during sexual activity
- Reduced rigidity at the base or shaft of the penis
- Decreased sensitivity or altered sensation
- Pain, aching, or pressure in the penis, scrotum, perineum, or anal area
Men with pelvic floor-related erectile dysfunction may also notice:
- Pelvic pain during or after sitting, exercise, or sexual activity
- Urinary urgency, frequency, hesitancy, or a weakened stream
- Discomfort during ejaculation or reduced ejaculation strength
- A feeling of tension or heaviness in the pelvic floor
- Gastrointestinal distress, bloating, or constipation that worsens with exercise or ejaculation
- Symptoms that fluctuate from day to day or appear without clear triggers
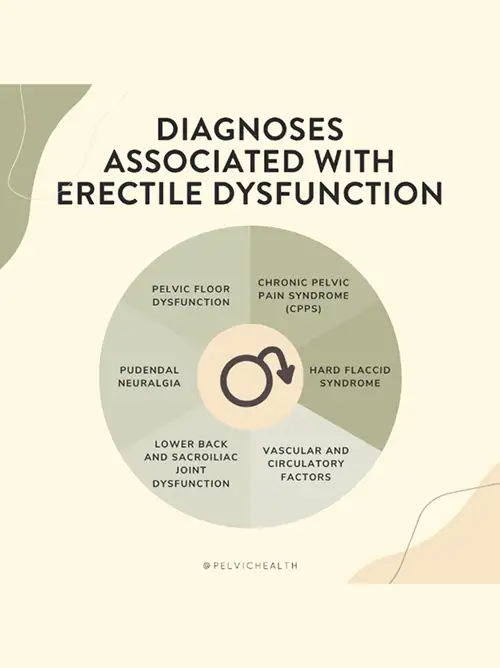
Associated Diagnoses
Erectile dysfunction often overlaps with other pelvic and musculoskeletal conditions that influence circulation, nerve signaling, and muscle function. These conditions can create additional strain on the pelvic floor or disrupt the pathways involved in arousal and erection. Common associated diagnoses include:
- Chronic Pelvic Pain Syndrome (CPPS): A condition marked by pelvic floor muscle tension, nerve irritation, and urinary or sexual symptoms. Many men with CPPS also experience erectile difficulties because the same muscles responsible for pelvic pain help support erections.
- Pudendal Neuralgia: Irritation of the pudendal nerve can cause burning, numbness, or aching in the penis, scrotum, and perineum. Because this nerve plays a major role in sexual function, pudendal neuralgia often contributes to arousal issues, pain with erection, or difficulty maintaining firmness.
- Hard Flaccid Syndrome: A pelvic floor and nerve related condition that creates altered penile sensation, changes in rigidity, increased pelvic tension, and erectile difficulties. It often reflects overactive pelvic floor muscles combined with nerve irritation.
- Lower Back and Sacroiliac Joint Dysfunction: Lumbar radiculopathy, disc issues, or SI joint dysfunction can disrupt the nerve pathways that support erections. These conditions may send referred pain into the pelvis or cause changes in sensation or sexual function.
- Vascular and Circulatory Factors: Pelvic venous congestion, vascular insufficiency, or prolonged sitting can influence blood flow to the erectile tissues. Pelvic floor tension frequently amplifies these vascular patterns by compressing or restricting nearby structures.
In many men, pelvic floor dysfunction acts as the central link. It can drive erectile issues directly or magnify symptoms from other systems, which is why a comprehensive pelvic evaluation is essential for accurate diagnosis and meaningful improvement.
Diagnostic Challenges
Erectile dysfunction caused by pelvic floor dysfunction can be difficult to diagnose because the causes do not appear clearly on imaging or routine lab work. Men are often told their symptoms are strictly vascular or psychological, even when the underlying issue involves pelvic floor dysfunction, nerve irritation, or musculoskeletal imbalance.
Since pelvic floor related erectile dysfunction does not show up on standard medical tests, it is frequently overlooked or misunderstood.
Another challenge is that erectile dysfunction often overlaps with other conditions such as pelvic pain, urinary symptoms, low back issues, or chronic muscle tension in the hips and pelvis. These patterns can mimic vascular or hormonal problems and lead to referrals that do not fully address the true contributors. Some men undergo extensive medical workups, try multiple medications, or receive conflicting explanations before anyone evaluates the pelvic floor.
Because the nerves and muscles involved in erections run through the pelvis, dysfunction in these structures can create changes in arousal, sensation, and rigidity. Yet many providers are not trained to assess pelvic floor involvement in erectile dysfunction, which leads to delays in receiving effective treatment. Furthermore, many pelvic floor physical therapists are not trained to treat male sexual dysfunction or pelvic pain. At PHRC we undergo advanced training in men’s health, we take a detailed and trauma informed approach, listening closely to your symptoms and examining how your pelvic floor, spine, and nervous system interact. This helps us identify the contributors that standard testing can miss and build a plan that supports long term improvement.
Since pelvic floor related erectile dysfunction does not show up on standard medical tests, it is frequently overlooked or misunderstood.
Another challenge is that erectile dysfunction often overlaps with other conditions such as pelvic pain, urinary symptoms, low back issues, or chronic muscle tension in the hips and pelvis. These patterns can mimic vascular or hormonal problems and lead to referrals that do not fully address the true contributors. Some men undergo extensive medical workups, try multiple medications, or receive conflicting explanations before anyone evaluates the pelvic floor.
Because the nerves and muscles involved in erections run through the pelvis, dysfunction in these structures can create changes in arousal, sensation, and rigidity. Yet many providers are not trained to assess pelvic floor involvement in erectile dysfunction, which leads to delays in receiving effective treatment. Furthermore, many pelvic floor physical therapists are not trained to treat male sexual dysfunction or pelvic pain. At PHRC we undergo advanced training in men’s health, we take a detailed and trauma informed approach, listening closely to your symptoms and examining how your pelvic floor, spine, and nervous system interact. This helps us identify the contributors that standard testing can miss and build a plan that supports long term improvement.
Treatment for ED Caused by Pelvic Floor Dysfunction
At PHRC, we design a plan that addresses your symptoms directly and helps you restore comfortable and reliable sexual function. Treatment can include:

- Pelvic floor physical and occupational therapy: Therapy focuses on releasing overactive muscles, reducing trigger points, improving coordination, and retraining the muscular patterns that support erections. Treatment also works to calm irritated nerves and improve the pressure system needed for strong, sustained rigidity.
- Spine and back treatment: If the nerves involved in erections are irritated in the lower back, therapy may include lumbar mobility work, posture training, and strategies that reduce nerve compression. In some cases, your medical team may recommend injections to calm inflammation if lumbar nerve irritation plays a major role.
- Circulation and vascular support: Pelvic floor treatment helps reduce muscle guarding around the pelvis, improve blood flow, and create balanced pressure around the erectile tissues. Posture work, breathing coordination, and tissue mobility techniques can reduce compression near vessels that influence erectile function.
- Addressing biomechanical issues: Hip mobility, core strength, and pelvic alignment all influence the pelvic floor’s ability to support erections. Therapy often includes exercises that improve hip function, reduce strain on the pelvis, and correct movement patterns that contribute to tension or weakness.
- Lifestyle adjustments: Managing constipation, reducing prolonged sitting, improving stress patterns, and gradually returning to exercise can reduce strain on the pelvic floor. These changes help create an environment where erections occur more easily and consistently.
How We Can Help You with Erectile Dysfunction
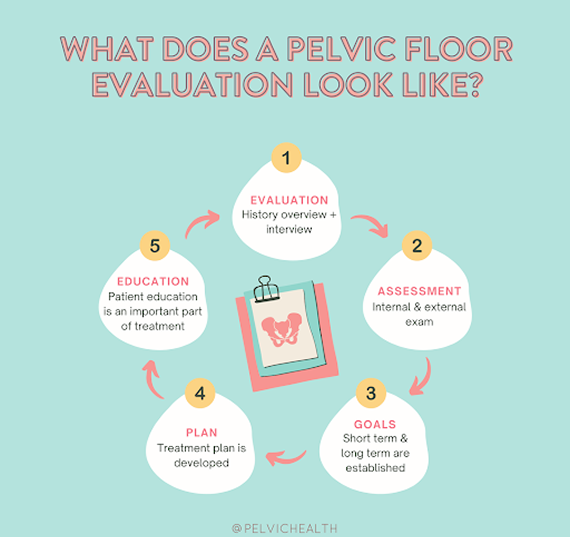
Men experiencing ED can benefit from an evaluation with a pelvic floor physical and occupational therapist specializing in pelvic pain. During your evaluation at PHRC, the pelvic floor physical and occupational therapist reviews your history and symptoms with you, what you have been diagnosed with in the past, the treatments you have undergone and how effective or not effective these treatments have been.
We understand what you have been going through and that most men are very frustrated by the time they see us.
During your physical examination the pelvic floor physical and occupational therapist examines muscles, tissues, joints, nerves, and your movement patterns. Once your pelvic floor physical and occupational therapist completes the examination they review your findings with you. They also create an assessment which explains how you developed pain and creates short and long-term goals for your treatment plan.
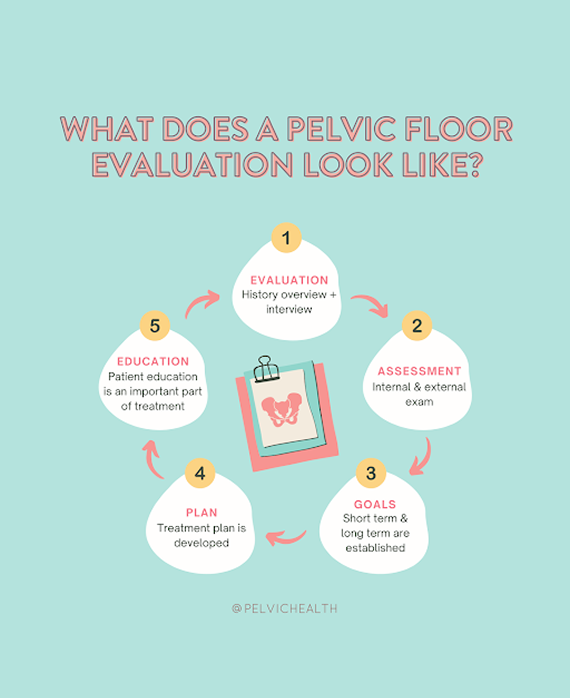
How We Can Help You with Erectile Dysfunction
Men experiencing ED can benefit from an evaluation with a pelvic floor physical and occupational therapist specializing in pelvic pain. During your evaluation at PHRC, the pelvic floor physical and occupational therapist reviews your history and symptoms with you, what you have been diagnosed with in the past, the treatments you have undergone and how effective or not effective these treatments have been.
We understand what you have been going through and that most men are very frustrated by the time they see us.
During your physical examination the pelvic floor physical and occupational therapist examines muscles, tissues, joints, nerves, and your movement patterns. Once your pelvic floor physical and occupational therapist completes the examination they review your findings with you. They also create an assessment which explains how you developed pain and creates short and long-term goals for your treatment plan.
Typically, the frequency of pelvic floor physical and occupational therapy treatment is one to two times per week for roughly 12 weeks. You are given a home exercise program to complement your in-person sessions, and your pelvic floor physical and occupational therapist will help to coordinate your recovery with the other members of your treatment team. At PHRC, we are here to help you recover and finally get relief from your symptoms.
