Symptoms you may notice include:
- A persistent or recurring burning, tingling, aching, or itching in the penis, scrotum, testicles, or around the perineum or anus
- Pain that worsens when sitting for too long, doing certain workouts, or wearing snug underwear
- Urinary issues such as frequent urges, difficulty starting the stream, or a weakened flow
- Discomfort during or after ejaculation, especially in the genital or perineal region
- Erectile dysfunction and changes in ejaculation strength
- Digestive symptoms like constipation or a bloated feeling
- Flare-ups triggered by activities such as exercise or ejaculation—or sometimes with no obvious cause
- Symptoms that appear in cycles, sometimes fading and then returning unexpectedly
For men in Glendale, pelvic floor physical and occupational therapy offers a direct, evidence-based approach to relieving symptoms by tackling the root dysfunction—not masking the pain.
Symptoms you may notice include:
- A persistent or recurring burning, tingling, aching, or itching in the penis, scrotum, testicles, or around the perineum or anus
- Pain that worsens when sitting for too long, doing certain workouts, or wearing snug underwear
- Urinary issues such as frequent urges, difficulty starting the stream, or a weakened flow
- Discomfort during or after ejaculation, especially in the genital or perineal region
- Erectile dysfunction and changes in ejaculation strength
- Digestive symptoms like constipation or a bloated feeling
- Flare-ups triggered by activities such as exercise or ejaculation—or sometimes with no obvious cause
- Symptoms that appear in cycles, sometimes fading and then returning unexpectedly
For men in Glendale, pelvic floor physical and occupational therapy offers a direct, evidence-based approach to relieving symptoms by tackling the root dysfunction—not masking the pain.
Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction

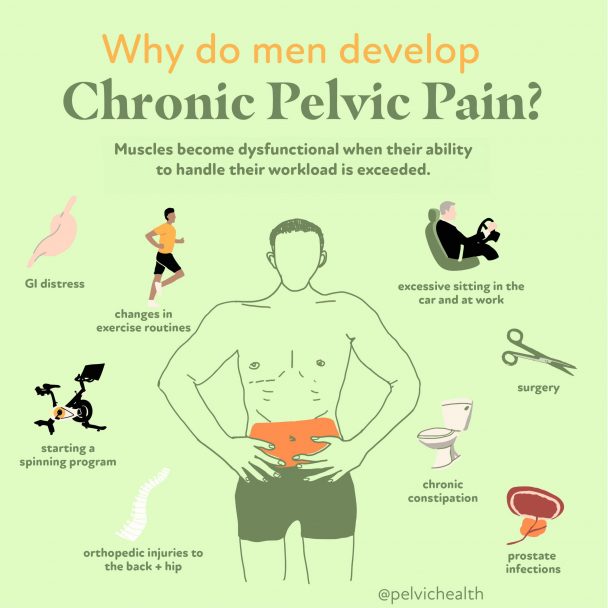
Causes of Pelvic Pain
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction
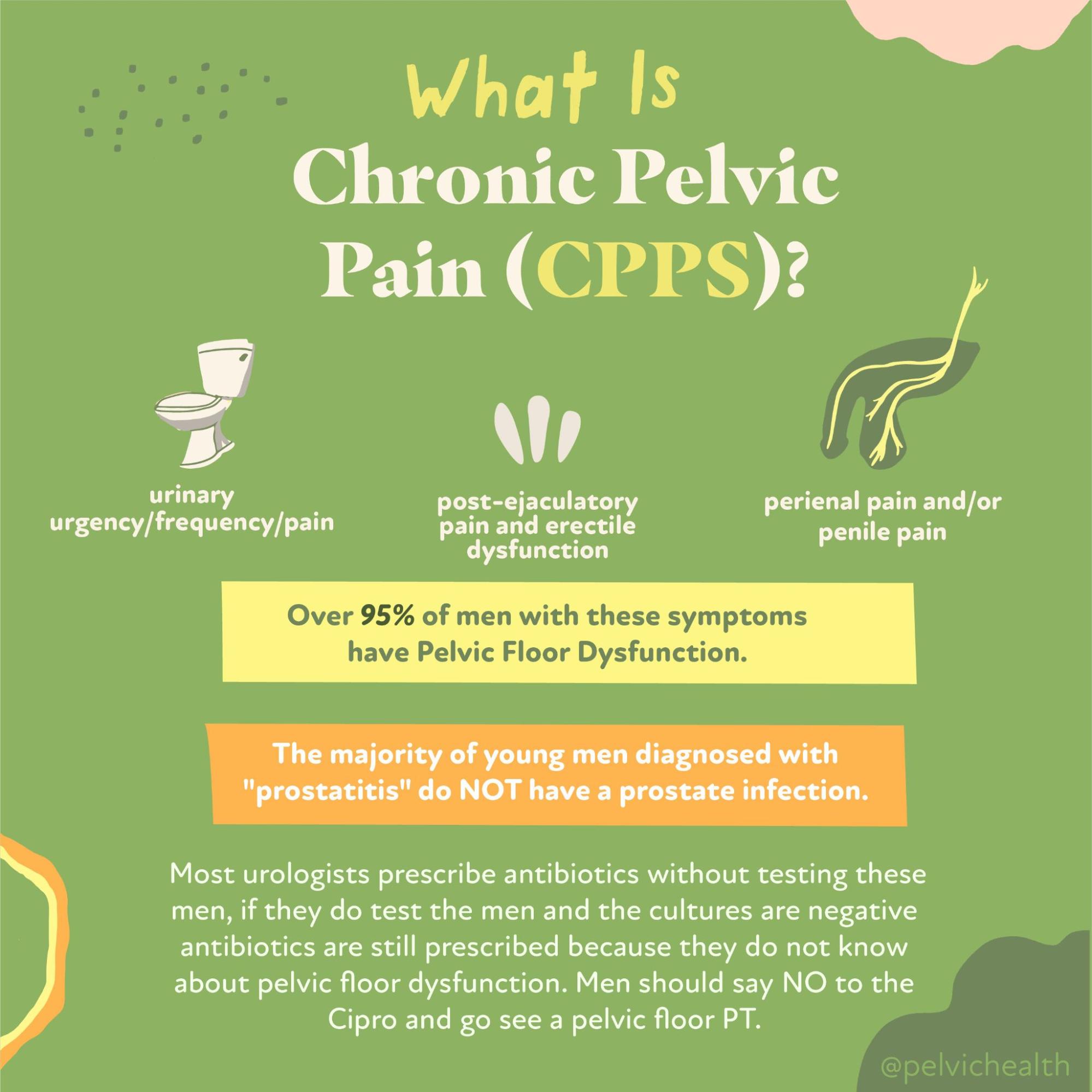
Diagnostic Challenges
Many men suffering from chronic pelvic pain go years without receiving the correct diagnosis. Studies show that it can take up to seven years for men with these symptoms to get an accurate assessment of what’s truly going on. This delay is often due to the fact that pelvic pain symptoms in men mimic those of prostate infections, urinary tract infections, or sexually transmitted infections. As a result, many healthcare professionals skip comprehensive testing and instead prescribe antibiotics based on assumptions. Unfortunately, this tends to overlook the actual root cause—pelvic floor dysfunction. Adding to the challenge, most pelvic floor therapists receive training focused on treating female anatomy, which can leave men struggling to find qualified care. That’s not an issue at PHRC, where our clinicians are deeply knowledgeable in male pelvic health, and it’s not uncommon for our male caseload to exceed that of our female patients on any given day.
It’s very common for men experiencing pelvic discomfort to receive a misdiagnosis of “prostatitis” and be placed on rounds of antibiotics, only to find little or no relief. However, scientific studies have shown that over 90% of men with persistent genitourinary symptoms—such as pain in the pelvic area, testicles, or perineum—do not actually have a bacterial infection of the prostate. Instead, most of these cases are classified under Chronic Pelvic Pain Syndrome (CPPS), specifically falling into NIH-defined categories IIIa or IIIb. These forms of CPPS represent a non-infectious source of discomfort that requires a completely different treatment approach.
The National Institutes of Health outlines five categories of prostatitis:
Category I: Acute bacterial prostatitis – sudden and intense onset, accompanied by systemic symptoms and an acute urinary tract infection.
Category II: Chronic bacterial prostatitis – marked by the persistence of bacterial infections in the prostate and recurring urinary tract infections.
Category IIIa: Inflammatory CPPS – identified by the presence of white blood cells in semen, prostatic secretions, or urine, indicating inflammation.
Category IIIb: Non-inflammatory CPPS – similar symptoms but with no white blood cells found in diagnostic fluids, suggesting no inflammation is present.
Category IV: Asymptomatic inflammatory prostatitis – inflammation is discovered during testing, even though the individual reports no visible symptoms.
Diagnostic Challenges
Many men suffering from chronic pelvic pain go years without receiving the correct diagnosis. Studies show that it can take up to seven years for men with these symptoms to get an accurate assessment of what’s truly going on. This delay is often due to the fact that pelvic pain symptoms in men mimic those of prostate infections, urinary tract infections, or sexually transmitted infections. As a result, many healthcare professionals skip comprehensive testing and instead prescribe antibiotics based on assumptions. Unfortunately, this tends to overlook the actual root cause—pelvic floor dysfunction. Adding to the challenge, most pelvic floor therapists receive training focused on treating female anatomy, which can leave men struggling to find qualified care. That’s not an issue at PHRC, where our clinicians are deeply knowledgeable in male pelvic health, and it’s not uncommon for our male caseload to exceed that of our female patients on any given day.
It’s very common for men experiencing pelvic discomfort to receive a misdiagnosis of “prostatitis” and be placed on rounds of antibiotics, only to find little or no relief. However, scientific studies have shown that over 90% of men with persistent genitourinary symptoms—such as pain in the pelvic area, testicles, or perineum—do not actually have a bacterial infection of the prostate. Instead, most of these cases are classified under Chronic Pelvic Pain Syndrome (CPPS), specifically falling into NIH-defined categories IIIa or IIIb. These forms of CPPS represent a non-infectious source of discomfort that requires a completely different treatment approach.
The National Institutes of Health outlines five categories of prostatitis:
Category I: Acute bacterial prostatitis – sudden and intense onset, accompanied by systemic symptoms and an acute urinary tract infection.
Category II: Chronic bacterial prostatitis – marked by the persistence of bacterial infections in the prostate and recurring urinary tract infections.
Category IIIa: Inflammatory CPPS – identified by the presence of white blood cells in semen, prostatic secretions, or urine, indicating inflammation.
Category IIIb: Non-inflammatory CPPS – similar symptoms but with no white blood cells found in diagnostic fluids, suggesting no inflammation is present.
Category IV: Asymptomatic inflammatory prostatitis – inflammation is discovered during testing, even though the individual reports no visible symptoms.
Treatment:
How We Can Help You

If you’re residing in Glendale and dealing with persistent pelvic pain, booking an evaluation with a skilled pelvic floor physical and occupational therapists could be the turning point in your recovery. During your first appointment, the therapist will take a detailed look into your health history, your specific symptoms, any past diagnoses you’ve received, and which treatments—if any—have worked or failed. Many men arrive at this stage feeling frustrated and discouraged, and that is completely understood and acknowledged.
Your therapist will conduct a thorough physical exam, checking the function of your pelvic muscles, the condition of nearby tissues, alignment of joints, nerve sensitivity, and how your body moves. Once the exam is complete, the therapist will walk you through the findings and design a plan tailored to your situation. Most Glendale treatment programs involve visiting the clinic once or twice weekly for around 12 weeks, combined with at-home exercises customized for you. Your physical and occupational therapists will also collaborate with any other care providers to ensure consistent and well-rounded support. Our goal is to help you feel like yourself again and enjoy life here in Glendale with confidence.

Treatment:
How We Can Help You
If you’re residing in Glendale and dealing with persistent pelvic pain, booking an evaluation with a skilled pelvic floor physical and occupational therapists could be the turning point in your recovery. During your first appointment, the therapist will take a detailed look into your health history, your specific symptoms, any past diagnoses you’ve received, and which treatments—if any—have worked or failed. Many men arrive at this stage feeling frustrated and discouraged, and that is completely understood and acknowledged.
Your therapist will conduct a thorough physical exam, checking the function of your pelvic muscles, the condition of nearby tissues, alignment of joints, nerve sensitivity, and how your body moves. Once the exam is complete, the therapist will walk you through the findings and design a plan tailored to your situation. Most Glendale treatment programs involve visiting the clinic once or twice weekly for around 12 weeks, combined with at-home exercises customized for you. Your physical and occupational therapists will also collaborate with any other care providers to ensure consistent and well-rounded support. Our goal is to help you feel like yourself again and enjoy life here in Glendale with confidence.
How Can We Help You?
If you have any questions or comments, we encourage you to use the form below to get in touch with us. Don’t forget to provide your email address so that we can respond directly to your message. Please know that any personal details you share will be handled with the utmost confidentiality and will not be shared or disclosed to others.

Join The Newsletter. Win a copy of our book, “Pelvic Pain Explained!”
We love getting to know our website visitors. Please tell us a little bit about yourself and get the latest info via PHRC e-newsletter!
*Subscribers automatically eligible to win our book, “Pelvic Pain Explained.”
At its foundation, Pelvic Pain Explained, is a powerful exploration of what it means to live with pelvic pain. The book takes a deep dive into the often confusing and frustrating process of getting a proper diagnosis, the many challenges faced by both patients and healthcare professionals, and the difficulty of sorting through a wide array of treatment options. It also shines a spotlight on the emotional and relational burden of dealing with a condition that isn’t outwardly visible—yet has a profound impact on daily life.


