Symptoms commonly associated with this condition include:
- Unpleasant sensations like aching, itching, or burning in the genital, anal, or perineal areas
- Discomfort caused or worsened by sitting, physical exertion, or snug-fitting clothes
- Bladder problems like urgency, frequent urges, or reduced urinary flow
- Pain associated with ejaculation or during sexual activity
- Erectile difficulties or changes in ejaculation force
- Digestive complaints, such as constipation or frequent bloating
- Flare-ups that are either triggered by specific actions or appear suddenly without warning
- Symptoms that cycle over time, seeming to resolve only to return again
If you’re in Silverlake and have faced these symptoms, pelvic floor physical and occupational therapy is a highly effective and evidence-based path to resolving the real source of your discomfort.
Symptoms commonly associated with this condition include:
- Unpleasant sensations like aching, itching, or burning in the genital, anal, or perineal areas
- Discomfort caused or worsened by sitting, physical exertion, or snug-fitting clothes
- Bladder problems like urgency, frequent urges, or reduced urinary flow
- Pain associated with ejaculation or during sexual activity
- Erectile difficulties or changes in ejaculation force
- Digestive complaints, such as constipation or frequent bloating
- Flare-ups that are either triggered by specific actions or appear suddenly without warning
- Symptoms that cycle over time, seeming to resolve only to return again
If you’re in Silverlake and have faced these symptoms, pelvic floor physical and occupational therapy is a highly effective and evidence-based path to resolving the real source of your discomfort.
Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

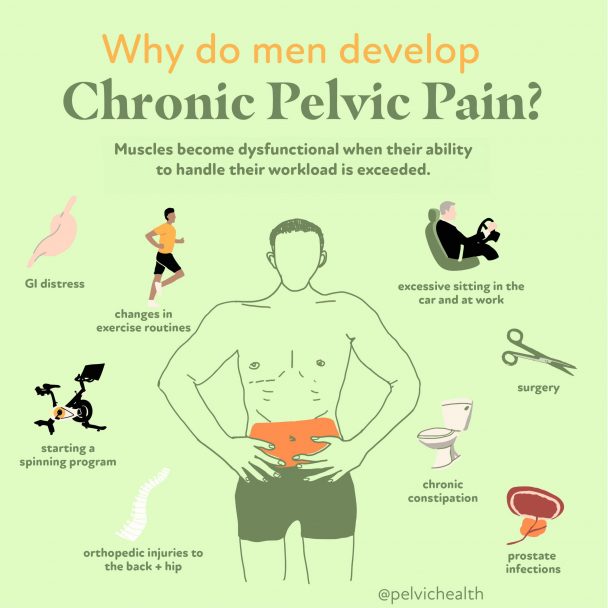
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction

Causes of Pelvic Pain
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction
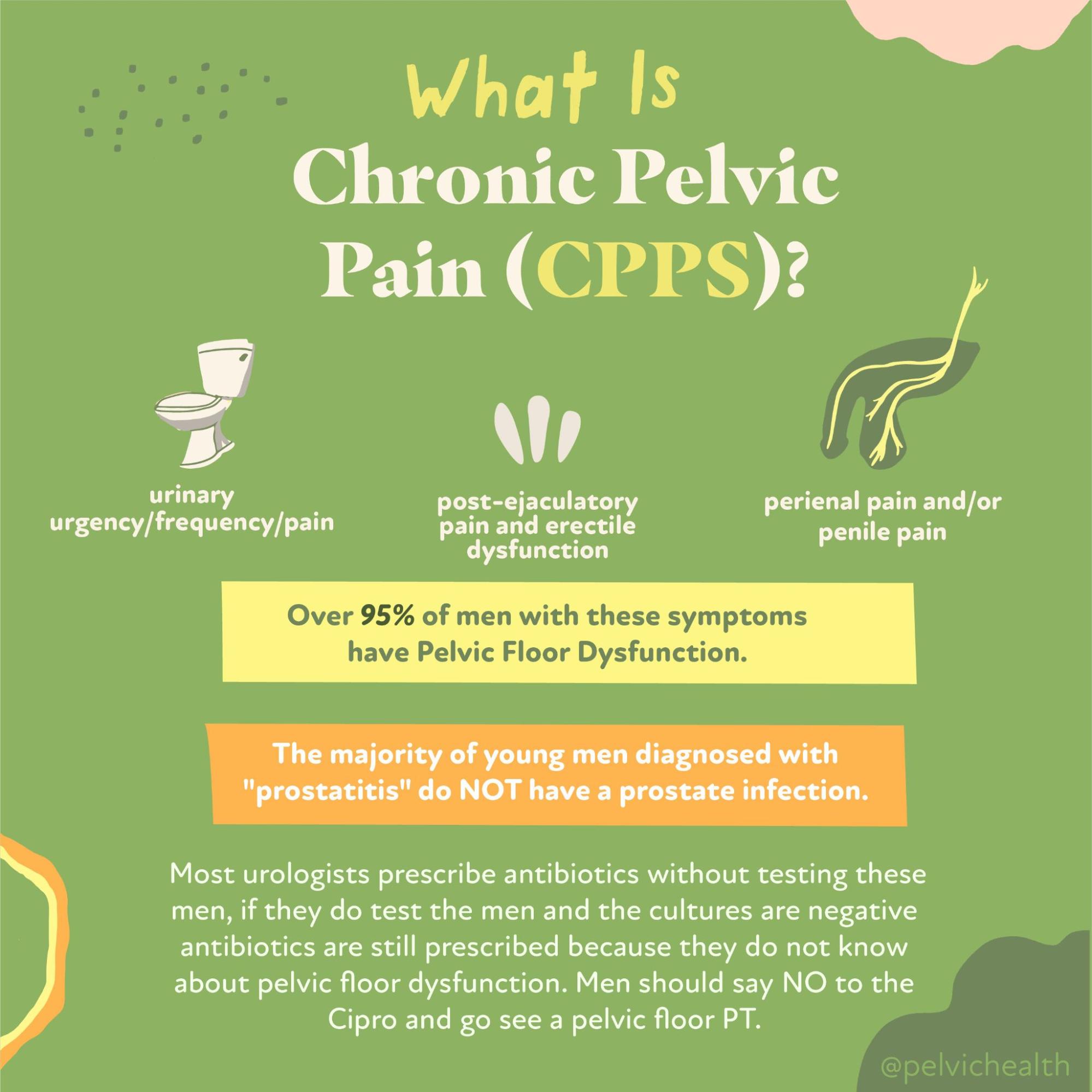
Diagnostic Challenges
It’s surprisingly common for men with pelvic pain to go years without receiving the right diagnosis. In fact, research suggests it can take up to seven years before a correct diagnosis is given. One of the main reasons for this delay is that pelvic pain in men often mimics other conditions, such as prostate issues, bladder infections, or STIs. Rather than taking the time to conduct thorough evaluations, many healthcare providers default to prescribing antibiotics as a first step. Sadly, this often leads patients down the wrong treatment path, leaving the true cause—pelvic floor dysfunction—unaddressed. Making matters more difficult, male patients frequently encounter physical and occupational therapistss whose training focuses primarily on female anatomy. PHRC stands apart in this regard; our therapists are extensively trained in male pelvic health, and we regularly treat more men than women in our clinics.
Many men suffering from chronic pelvic pain are misdiagnosed with “prostatitis” and prescribed antibiotics, even though no infection is present. Medical research confirms that more than 90% of men who experience genitourinary pain—such as discomfort in the pelvic region or testicular area—do not suffer from bacterial prostatitis. Instead, their condition usually falls under the umbrella of Chronic Pelvic Pain Syndrome (CPPS), especially in forms described by the National Institutes of Health as Category IIIa or IIIb.
These non-bacterial syndromes require a very different management strategy, often involving physical and occupational therapy rather than pharmaceuticals.
Here’s how the NIH classifies prostatitis conditions:
Category I: Acute bacterial prostatitis – a sudden, painful condition involving infection, inflammation, and systemic illness.
Category II: Chronic bacterial prostatitis – identified by long-term prostate infections and repeated episodes of urinary tract infections.
Category IIIa: Inflammatory CPPS – where testing reveals white blood cells in ejaculate or urine samples, confirming inflammation.
Category IIIb: Non-inflammatory CPPS – shows no such immune cell presence, despite persistent symptoms and discomfort.
Category IV: Asymptomatic inflammatory prostatitis – an unexpected diagnosis discovered through testing even when the patient feels no discomfort.
Diagnostic Challenges
It’s surprisingly common for men with pelvic pain to go years without receiving the right diagnosis. In fact, research suggests it can take up to seven years before a correct diagnosis is given. One of the main reasons for this delay is that pelvic pain in men often mimics other conditions, such as prostate issues, bladder infections, or STIs. Rather than taking the time to conduct thorough evaluations, many healthcare providers default to prescribing antibiotics as a first step. Sadly, this often leads patients down the wrong treatment path, leaving the true cause—pelvic floor dysfunction—unaddressed. Making matters more difficult, male patients frequently encounter physical and occupational therapistss whose training focuses primarily on female anatomy. PHRC stands apart in this regard; our therapists are extensively trained in male pelvic health, and we regularly treat more men than women in our clinics.
Many men suffering from chronic pelvic pain are misdiagnosed with “prostatitis” and prescribed antibiotics, even though no infection is present. Medical research confirms that more than 90% of men who experience genitourinary pain—such as discomfort in the pelvic region or testicular area—do not suffer from bacterial prostatitis. Instead, their condition usually falls under the umbrella of Chronic Pelvic Pain Syndrome (CPPS), especially in forms described by the National Institutes of Health as Category IIIa or IIIb.
These non-bacterial syndromes require a very different management strategy, often involving physical and occupational therapy rather than pharmaceuticals.
Here’s how the NIH classifies prostatitis conditions:
Category I: Acute bacterial prostatitis – a sudden, painful condition involving infection, inflammation, and systemic illness.
Category II: Chronic bacterial prostatitis – identified by long-term prostate infections and repeated episodes of urinary tract infections.
Category IIIa: Inflammatory CPPS – where testing reveals white blood cells in ejaculate or urine samples, confirming inflammation.
Category IIIb: Non-inflammatory CPPS – shows no such immune cell presence, despite persistent symptoms and discomfort.
Category IV: Asymptomatic inflammatory prostatitis – an unexpected diagnosis discovered through testing even when the patient feels no discomfort.
Treatment:
How We Can Help You

Living in Silverlake and coping with pelvic pain can be incredibly isolating, but starting with an evaluation from a pelvic floor physical and occupational therapists can open the door to effective, lasting relief. At your initial session, the therapist will spend time learning about your history—everything from your current symptoms and previous diagnoses to past treatments and whether they brought any relief. We understand that for many men in Silverlake, this isn’t the first attempt to get help, and it often follows a long and frustrating journey.
Your physical and occupational therapists will then conduct a complete assessment of your pelvic floor muscles, surrounding structures like joints and nerves, and how your body moves during different tasks. After this evaluation, they’ll explain what’s been discovered and present a structured treatment plan that explains the origins of your pain and how they aim to resolve it. Most treatment programs include sessions once or twice a week for roughly 12 weeks, with a home program to keep progress going outside of the clinic. Your therapist will also work hand-in-hand with other providers if you have a broader care team. Silverlake residents can trust that compassionate and expert care is available locally.

Treatment:
How We Can Help You
Living in Silverlake and coping with pelvic pain can be incredibly isolating, but starting with an evaluation from a pelvic floor physical and occupational therapists can open the door to effective, lasting relief. At your initial session, the therapist will spend time learning about your history—everything from your current symptoms and previous diagnoses to past treatments and whether they brought any relief. We understand that for many men in Silverlake, this isn’t the first attempt to get help, and it often follows a long and frustrating journey.
Your physical and occupational therapists will then conduct a complete assessment of your pelvic floor muscles, surrounding structures like joints and nerves, and how your body moves during different tasks. After this evaluation, they’ll explain what’s been discovered and present a structured treatment plan that explains the origins of your pain and how they aim to resolve it. Most treatment programs include sessions once or twice a week for roughly 12 weeks, with a home program to keep progress going outside of the clinic. Your therapist will also work hand-in-hand with other providers if you have a broader care team. Silverlake residents can trust that compassionate and expert care is available locally.
How Can We Help You?
Got a question or something you’d like to share with us? Use the form below to reach out. Make sure to enter your email address so we can provide a direct response. We take your privacy seriously—everything you submit will be kept entirely confidential and won’t be shared with anyone else.

Join The Newsletter. Win a copy of our book, “Pelvic Pain Explained!”
We love getting to know our website visitors. Please tell us a little bit about yourself and get the latest info via PHRC e-newsletter!
*Subscribers automatically eligible to win our book, “Pelvic Pain Explained.”
At the heart of Pelvic Pain Explained lies a detailed account of what it’s like for people living with pelvic pain—from the initial, confusing symptoms to the winding path toward a proper diagnosis and treatment. The book offers insight into the professional and personal roadblocks along the way, uncovers the challenge of weighing treatment choices, and gives voice to the silent suffering that often accompanies an invisible illness. It paints a complete picture of both the medical and emotional realities of this condition.


