Symptoms Commonly Seen in Men Include:
- A sensation of burning, aching, itching, or general discomfort in the penis, scrotum, testicles, anal, or perineal regions
- Increased pain when engaging in physical activity, sitting for long periods, or wearing tight clothing
- Issues related to urination, such as urgency, hesitancy, frequency, or a weak stream
- Pain or discomfort during or after ejaculation, particularly in the penis, scrotum, or perineum
- Erectile dysfunction symptoms, sometimes coupled with reduced ejaculation force
- Digestive problems including bloating and constipation
- Symptoms that may worsen after physical exertion or appear unexpectedly without a clear trigger
- Fluctuating symptom patterns, with discomfort coming and going over time
For Temecula residents seeking lasting relief, pelvic floor physical and occupational therapy can provide targeted treatment that addresses the root cause of the issue—not just the symptoms.
Symptoms Commonly Seen in Men Include:
- A sensation of burning, aching, itching, or general discomfort in the penis, scrotum, testicles, anal, or perineal regions
- Increased pain when engaging in physical activity, sitting for long periods, or wearing tight clothing
- Issues related to urination, such as urgency, hesitancy, frequency, or a weak stream
- Pain or discomfort during or after ejaculation, particularly in the penis, scrotum, or perineum
- Erectile dysfunction symptoms, sometimes coupled with reduced ejaculation force
- Digestive problems including bloating and constipation
- Symptoms that may worsen after physical exertion or appear unexpectedly without a clear trigger
- Fluctuating symptom patterns, with discomfort coming and going over time
For Temecula residents seeking lasting relief, pelvic floor physical and occupational therapy can provide targeted treatment that addresses the root cause of the issue—not just the symptoms.
Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

Associated Diagnoses
Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Chronic Nonbacterial Prostatitis, Pudendal Neuralgia, Hard Flaccid Syndrome and Interstitial Cystitis/Painful Bladder Syndrome are all pain syndromes that cause pelvic pain due to pelvic floor dysfunction.

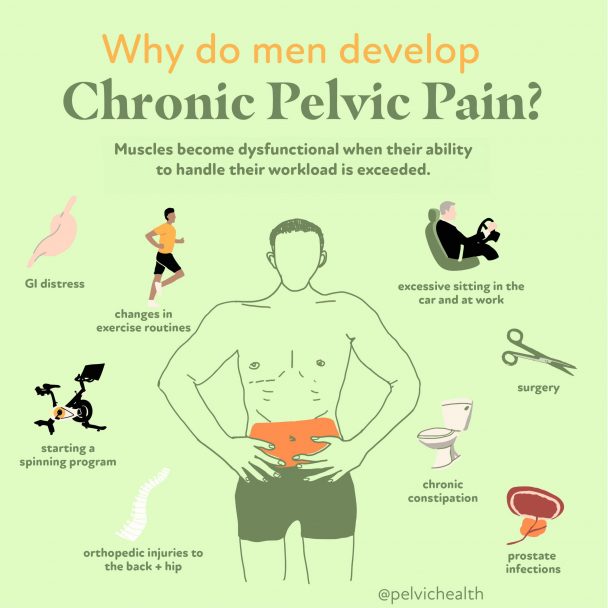
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction

Causes of Pelvic Pain
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain, with or without urinary or bowel complaints, have pelvic floor dysfunction
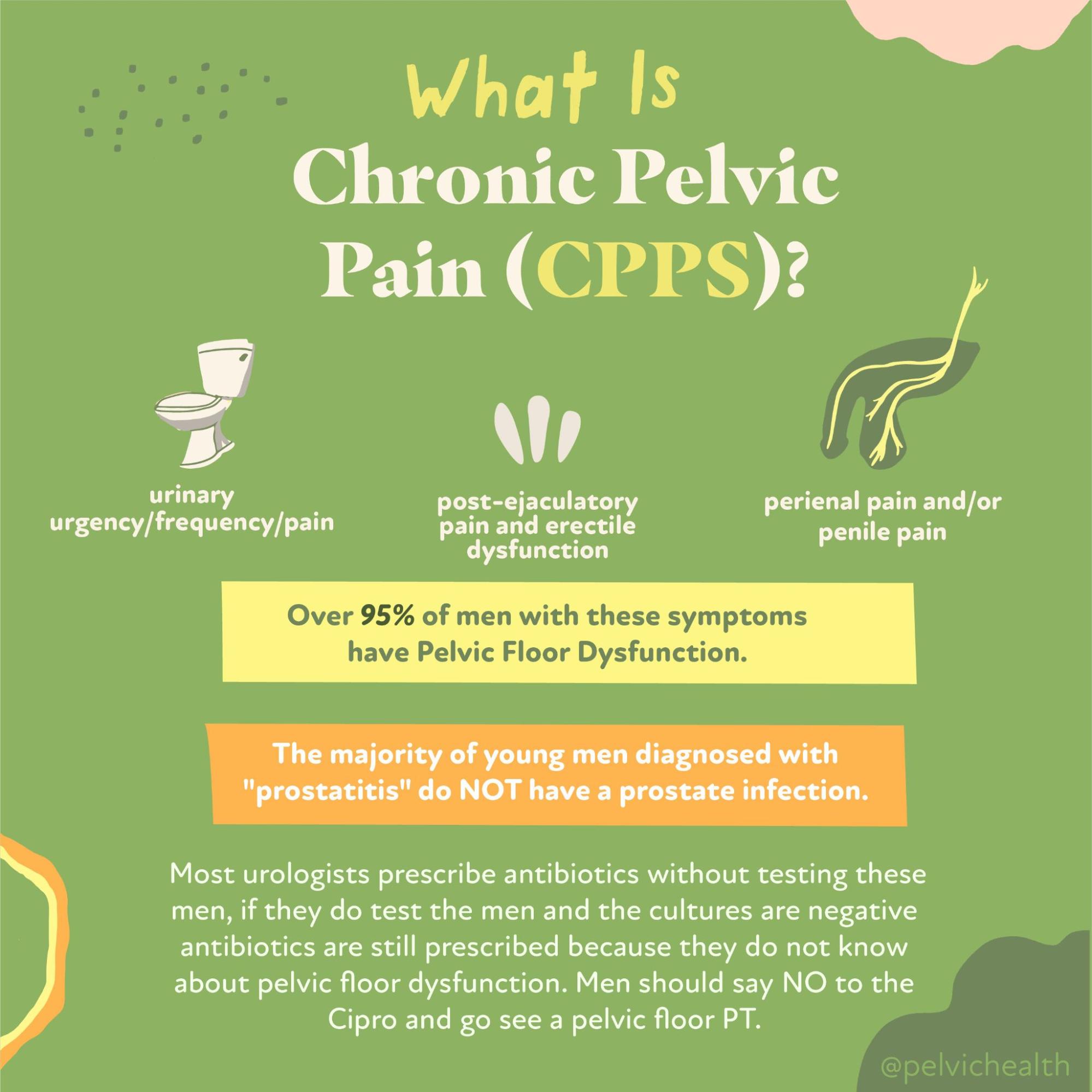
Diagnostic Challenges
It’s not uncommon for men with pelvic pain to go undiagnosed or misdiagnosed for years—research indicates that it can take up to seven years to receive an accurate diagnosis. This delay is largely because the symptoms often resemble those of prostate conditions, bladder infections, or STIs. Rather than conduct the in-depth testing required to confirm a prostate infection, many healthcare providers choose to prescribe antibiotics preemptively. Unfortunately, this approach often misses the real issue: pelvic floor dysfunction. What makes things more complicated is that most pelvic floor therapists are primarily trained to treat women, leaving men underserved. That’s not the case at PHRC, where our team is highly experienced in treating male pelvic health—and on many days, we see more men than women.
It’s not uncommon for men with pelvic pain to be wrongly diagnosed with “prostatitis,” leading to unnecessary antibiotic treatments that fail to resolve the underlying issue. In reality, studies have demonstrated that more than 90% of males who report pain or discomfort in the genitourinary region do not have a bacterial prostate infection. Instead, these cases usually fall into categories IIIa or IIIb as defined by the National Institutes of Health (NIH), which are recognized forms of Chronic Pelvic Pain Syndrome (CPPS).
Here is how the NIH classifies prostatitis syndromes:
Category I: Acute bacterial prostatitis – characterized by severe symptoms, systemic infection, and a sudden onset of a urinary tract infection.
Category II: Chronic bacterial prostatitis – typically involves recurrent UTIs and ongoing bacterial presence in the prostate gland.
Category IIIa: Inflammatory CPPS – defined by the presence of white blood cells in semen, prostatic secretions, or urine samples.
Category IIIb: Non-inflammatory CPPS – where diagnostic samples show no evidence of white blood cells, despite ongoing symptoms.
Category IV: Asymptomatic inflammatory prostatitis – marked by inflammation found during diagnostic testing but with no outward symptoms reported by the patient.
Diagnostic Challenges
It’s not uncommon for men with pelvic pain to go undiagnosed or misdiagnosed for years—research indicates that it can take up to seven years to receive an accurate diagnosis. This delay is largely because the symptoms often resemble those of prostate conditions, bladder infections, or STIs. Rather than conduct the in-depth testing required to confirm a prostate infection, many healthcare providers choose to prescribe antibiotics preemptively. Unfortunately, this approach often misses the real issue: pelvic floor dysfunction. What makes things more complicated is that most pelvic floor therapists are primarily trained to treat women, leaving men underserved. That’s not the case at PHRC, where our team is highly experienced in treating male pelvic health—and on many days, we see more men than women.
It’s not uncommon for men with pelvic pain to be wrongly diagnosed with “prostatitis,” leading to unnecessary antibiotic treatments that fail to resolve the underlying issue. In reality, studies have demonstrated that more than 90% of males who report pain or discomfort in the genitourinary region do not have a bacterial prostate infection. Instead, these cases usually fall into categories IIIa or IIIb as defined by the National Institutes of Health (NIH), which are recognized forms of Chronic Pelvic Pain Syndrome (CPPS).
Here is how the NIH classifies prostatitis syndromes:
Category I: Acute bacterial prostatitis – characterized by severe symptoms, systemic infection, and a sudden onset of a urinary tract infection.
Category II: Chronic bacterial prostatitis – typically involves recurrent UTIs and ongoing bacterial presence in the prostate gland.
Category IIIa: Inflammatory CPPS – defined by the presence of white blood cells in semen, prostatic secretions, or urine samples.
Category IIIb: Non-inflammatory CPPS – where diagnostic samples show no evidence of white blood cells, despite ongoing symptoms.
Category IV: Asymptomatic inflammatory prostatitis – marked by inflammation found during diagnostic testing but with no outward symptoms reported by the patient.
Treatment:
How We Can Help You

If you’re living in Temecula and experiencing pelvic pain, seeking an evaluation from a pelvic floor physical and occupational therapists can be a vital first step toward relief. At your initial session, your therapist will take time to listen and understand your medical background, symptom history, previous diagnoses, and the effectiveness of any treatments you’ve already undergone. We understand that many men who come to us are frustrated from dealing with unresolved issues.
During the exam, the therapist will carefully assess your pelvic muscles, surrounding tissues, joints, nerves, and movement patterns. Afterward, they’ll explain the findings clearly and develop a tailored plan that outlines how your pain developed and how to address it moving forward. Most treatment plans in Temecula involve sessions one to two times per week over the course of about 12 weeks, supported by a custom home exercise regimen. Your therapist will also work in collaboration with any other healthcare providers you may be seeing. We’re here to help you restore function and get back to enjoying your life in Temecula.

Treatment:
How We Can Help You
If you’re living in Temecula and experiencing pelvic pain, seeking an evaluation from a pelvic floor physical and occupational therapists can be a vital first step toward relief. At your initial session, your therapist will take time to listen and understand your medical background, symptom history, previous diagnoses, and the effectiveness of any treatments you’ve already undergone. We understand that many men who come to us are frustrated from dealing with unresolved issues.
During the exam, the therapist will carefully assess your pelvic muscles, surrounding tissues, joints, nerves, and movement patterns. Afterward, they’ll explain the findings clearly and develop a tailored plan that outlines how your pain developed and how to address it moving forward. Most treatment plans in Temecula involve sessions one to two times per week over the course of about 12 weeks, supported by a custom home exercise regimen. Your therapist will also work in collaboration with any other healthcare providers you may be seeing. We’re here to help you restore function and get back to enjoying your life in Temecula.
How Can We Help You?
Feel free to reach out using the form below with any questions or comments you may have. Be sure to include your email address so we can reply directly to your inquiry. Rest assured, all the information you share with us will remain strictly confidential.

Join The Newsletter. Win a copy of our book, “Pelvic Pain Explained!”
We love getting to know our website visitors. Please tell us a little bit about yourself and get the latest info via PHRC e-newsletter!
*Subscribers automatically eligible to win our book, “Pelvic Pain Explained.”
At its core, Pelvic Pain Explained explores the journey of individuals who suffer from pelvic pain. It delves into the complex road to diagnosis and treatment, the hurdles both patients and healthcare providers encounter, and the overwhelming task of navigating a range of treatment options. It also sheds light on how living with a condition that can’t be seen takes a toll on daily life and personal relationships—and so much more.


