Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
We live in a different time. I remember when chat rooms and meeting people from the internet was the plot line for a Lifetime movie. Now, we get in cars driven by strangers and fall in love via sophisticated algorithms and profile pictures. What a time to be alive! It is pretty apparent that technology plays a huge role in our lives. Since I live in the tech mecca of San Francisco, I am surrounded by techies and have connected with several start-ups that specialize in a field that I hold very near and dear to my heart: sex! At first, I thought that I had discovered a small niche in the tech community; now I know that technology and sexual health have quite the relationship, one that is more extensive than you might guess.
These days, the role of technology in sex is so much more than online pornography, although that market is still booming (or so I’ve heard). First, there is a whole wide world of alluring apps. There are apps, such as Kindu and Undercovers, that allow you and your partner to find new sexy things to try together. Think R-rated truth or dare, but sans slumber party with the added bonus of being able to potentially play on your commute! There are apps that give you ideas for new sex positions to try or even places to try them in. Finally, there are the obvious hook-up dating apps, including some that help you find a third (or fourth) should you be in the mood for some late night company.
Then there are some apps with not-so-carnal intentions, such as Tabú, a start-up that I have recently become involved with as a “sexpert.” And yes, my parents are “so proud.” Tabú helps promote sexual education via an app that allows its users to post questions and receive answers from their peers, as well as “sexperts,” who have been approved by Tabú as being knowledgeable in the field of sexual health. Tabú also has a college ambassador program to allow college students to provide quality sex education via campus workshops . Per Mia Davis, the founder of Tabú, “the goal of Tabú is to empower ‘millennials’ to take control of their sexual health. We understand that misinformation is rife in sexuality, and to truly break down the myths and taboos, we need to provide young people with answers. We believe that to open up a dialogue, we need to approach young people where they are – their phones, social media, and for college students, on their campuses.” With more and more people using smartphones and apps to interact, having resources to provide solid education to people is crucial. And education can be as simple as knowing about your own body. As you know, I am a big advocate for getting to know yourself, which I discussed at length in this post. Luckily, there are many apps that allow people to learn all about their sexual health and health in general. Certain apps, such as Clue and Glow, allow people to track their menstrual cycle, ovulation and other details relating to fertility. Some, such as Pelvic Track, even allow individuals to track symptoms related to pelvic floor dysfunction, such as pain and incontinence.
Some apps even connect with other devices to help improve pelvic floor motor control ( like a fitbit for your vagina). Here is one example. Another company, Lioness, has developed a “smart” vibrator that helps users to better understand how they experience sexual pleasure. The vibrator pairs with an app that provides biometric data about how quickly the user becomes aroused and how long it takes to orgasm. The app allows the users to share this information with their partner. Some other vibrators on the market even allow your partner to control the device from afar via their cell phone! This can be useful for long distance relationships or for patients with pelvic pain who cannot tolerate penetration but still want sexual intimacy with their partner.
Intimacy is a key word. Smartphones and laptops have almost become a silent partner for most of us. It brings us information from other people that makes us feel like we are in constant contact without having any real contact at all. This brings me to one of the downsides of the internet and technology in general: everyone has access to it and can therefore contribute content. I frequently see patients who — terrified after reading about someone who was bed bound with pelvic pain for five years — ask, “Will that happen to me?” The thing I remind my patients is that it is impossible to know who your new internet “friend” really is. The person writing could be a thirteen year old teen who thinks it is hilarious to post in forums for people with chronic pain. Why? We may never know. Just like Pokemon-Go’s popularity, some things may never make sense. Just like the person who posted that he cured himself with some wonder-herb and is living the pain-free dream. Maybe he did, and that is great, but that doesn’t mean he has a medical background or any knowledge about your unique history and symptoms. In other words, Basically why should internet user #10065 be trusted to give you advice? The internet is not the end-all, be-all of information. I mean, Dr. Google didn’t even go to medical school! However, you can find a lot of well researched information online. Please refer to Liz’s post on determining what articles are legitimate. Yes, the internet can create great communities as a way to form support groups of people who share similar experiences, but remember to, always take information with a grain of salt.
Now, if you think the present world of sex and tech is amazing, wait till you hear what the future holds. Love and sex with robots may be here sooner than we think. I wonder, will the legalization of robot marriage be a future debate topic? Will 3-D printed robot babies be the new norm? The ethical and philosophical questions that go along with a robotic romance are endless, and if I am brave enough, I may explore it in a later post (or while watching Westworld). Sex-bots may still be in the future, but this sweet virtual reality sex jumpsuit is currently available in — surprise — Japan! While these developments make me question what this means for the future of intimacy and relationships, virtual reality and robots may have a positive impact on controlling STD/STIs and unplanned pregnancies. Furthermore, this type of technology may let you discover your own wants and needs without the pressure of a (human) partner being present.
As a provider, I find the potential future impact of technology on sexual health both fascinating and at times frightening. Someday, will I be treating patients who can’t have sex with their robot husbands? Or will I be treating robots which have such advanced Artificial Intelligence that they have chronic pelvic pain and are unable to function as “human beings?” But what scares me is this: what if I already am?
FAQ
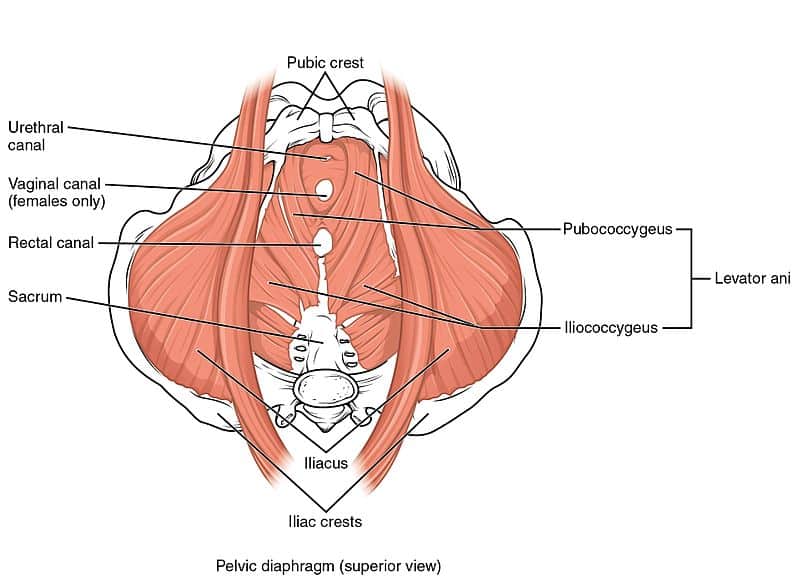
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Admin
During pregnancy and the postpartum period, many women suffer from both functional and cosmetic issues caused from the widening of the abdominal wall from stretch and pressure generated from the growing uterus. This stretching can result in a separation of the rectus abdominis muscle, known as a diastasis recti (DR). Diastasis recti occur in approximately 66% of women in their third trimester of pregnancy 1, many of which continue to suffer even 1-year postpartum, despite physical and occupational therapy or exercise programs designed to close this gap. In addition to the pregnant/postpartum population, others can suffer from this as well, including athletes, babies, and even patients who have undergone laparoscopic surgery such as hysterectomy, endometriosis, and prostatectomy.
Malinda wrote a great blog all about DR that you can read here that discusses functional limitations a DR could impose, how to check for it, and some basics on how to close it. This blog will focus on the ongoing debate of what researchers and clinicians believe is the best way to rehabilitate diastasis recti.
Is it really important that there is a wider gap than before pregnancy or surgery? Should we focus on crunches, abdominal bracing, or surgery? What should be done when exercise is not enough? And ultimately, how does one know when someone may require surgical intervention?
Anatomy of diastasis recti
The rectus abdominis is what we commonly think of as our six-pack muscle that connects from our sternum all the way to our pubic bone. We have two of them, one on the right and one on the left, that are separated by a dense band of connective tissue known as the linea alba. The linea alba is made from a continuation of our internal obliques, external obliques, and the transverse abdominal muscles.
What is the function of our abdominal muscles?
The function of the abdominal musculature is to resist changes in intra-abdominal pressure (IAP), and transfer forces between our right and left sides during movement such as lifting our legs, twisting, etc. When there is a widening of these muscles and the linea alba becomes lax, we lose this ability, and it is possible that we may experience low back pain, weakness, pelvic girdle pain, urinary incontinence, and in time, even pelvic organ prolapse may occur.
What is normal?
In general, there is debate about how wide the inter-rectus distance (IRD) can be, and researchers have performed imaging in cadavers, as well as in women who have not had children (nulliparous), to determine what is “normal.” How wide and at which points to measure vary in the literature, and currently there is no international consensus in the best way to measure. Most recently, there was a study performed on nulliparous women that suggested a normal linea alba should be less than 15mm at the xiphoid level, 33mm at 3 cm above the umbilicus and 16mm at 2 cm below the umbilicus.3
The Debate
Most physical and occupational therapistss, trainers, and exercise programs that currently exist tend to focus on closing the gap between the rectus abdominis muscle bellies. At PHRC and many other clinics, we teach patients to pull the bellybutton to the spine (a draw-in maneuver that activates our transverse abdominis muscle also called a TrA contraction) and then with a towel wrapped around the widest part of the gap, do a mini abdominal crunch which activates the rectus abdominis muscle bellies and pulls them closer together. It has generally been thought that the TrA contraction will draw the muscle bellies of the rectus abdominis together and improve stability of the core, while abdominal crunches alone have been considered a risk for the development of DR. 4
The Research
There was a recent journal article released from the Journal of Orthopedic and Sport Physical and Occupational Therapy (JOSPT) that actually looked at the effect of a drawing-in maneuver (or TrA contraction) and the abdominal crunch in its ability to decrease the IRD. Surprisingly, it showed that doing a draw-in maneuver caused a slight widening of the IRD, while the abdominal crunch in both the gestational period (during pregnancy) and postpartum periods showed a narrowing of the IRD 2 – which has been the focus of rehab!
This was interesting because like I said before, abdominal crunches tend to not be the exercise of choice and have been thought to be a risk factor for DR. This also led to the question – does closing the gap really matter as much as we previously thought?
Technically, we do not just have patients do a draw-in maneuver, nor do we have them just do crunches or sit ups to correct the DR, we actually teach them a very specific way to do this correction exercise, and it involves a combination of the two exercises. In a very recent study by Diane Lee and Paul Hodges, they did look at what happens at the IRD with an abdominal crunch alone, and an abdominal crunch with pre-activation of the transverse abdominis muscle or a “draw-in” maneuver. What they found was that doing a draw-in maneuver with a crunch decreased the narrowing of the IRD compared to what would occur with an abdominal crunch alone. This still technically does not close the DR as well as we’d like, but it does increase the tension on the linea alba, which they propose is necessary to support the abdominal contents and to transfer force between the two sides of the abdominal wall.5
Currently, the goal of rehabilitating a DR is to reduce the IRD. This is based on the assumption that closing the gap will restore the function of the core and improve cosmetic appearance. Lee and Hodges showed the opposite in their study, and demonstrated that while we are closing the gap, we are creating more laxity or distortion on the linea alba, which makes us less likely to restore the function of our abdominal wall; this will lead to potentially poorer cosmesis of the abdominal wall.
What to do now?
It seems that closing the gap may not matter as much as we previously thought, and instead of focusing on the width of the gap, we should be focusing on optimizing the functional ability of our abdominal wall to generate enough tension to stabilize us in order to perform the activities we do on a regular basis and this will vary individually.
If you suffer from a DR and have not been assessed by a physical and occupational therapists, start there! During their evaluation, the physical and occupational therapists will be able to identify functional and structural impairments that may be contributing to ongoing symptoms, and can either help you to continue to improve your function, or have the resources to refer you to a surgeon if conservative approaches have been exhausted.
Below is a list of criteria that would identify a good surgical candidate, your physical and occupational therapists can help determine if you would benefit from a surgical consult. To find out more about pregnancy and postpartum physical and occupational therapy, visit our website or our Pinterest page.
Who actually needs surgical intervention?
According to Dianne Lee, the criteria for referral to a surgeon are summarized below:
- The woman should be at least 1 year postpartum and has failed appropriate therapeutic approaches to restore function, resolve lumbopelvic pain and/or urinary incontinence.
- The inter-recti distance is greater than mean values, and the abdominal contents are easily palpated through the midline fascia.
- Multiple vertical loading tasks reveal failed load transfer through the lumbopelvis.
- The active straight leg raise test is positive, and the effort to lift the leg improves with both approximation of the pelvis anteriorly, as well as approximation of the lateral fascial edges of rectus abdominis.
- The articular system tests for passive integrity of the joint of the low back and/or pelvis (mobility and stability) are normal.
References:
- Diastasis Rectus Abdominis & Postpartum Health Consideration for Exercise training: http://dianelee.ca/article-diastasis-rectus-abdominis.php
- Mota P, Pascoal AG, Carita AI, Bo K. The immediate effects on inter-rectus difference of abdominal crunch and drawing-in exercises and during pregnancy and the postpartum period. J Orthop Sport PhysTher. 2015; 45(10):781-788.
- Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA. The normal width of the linea alba in nulliparous women. Clin Anat. 2009;22:706-711. http://dx.doi.org/10.1002/ ca.20836
- Blanchard PD. Diastasis recti abdominis in HIV-infected men with lipodystrophy. HIV Med. 2005;6:54-56. http://dx.doi. org/10.1111/j.1468-1293.2005.00264.x
- Lee D, Hodges PW. Behavior of the linea alba during a curl-up task in diastasis rectus abdominis: an observational study. J Orthop Sports Phys Ther. 2016;46(7):580-589.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Shannon Pacella, DPT, PHRC Lexington
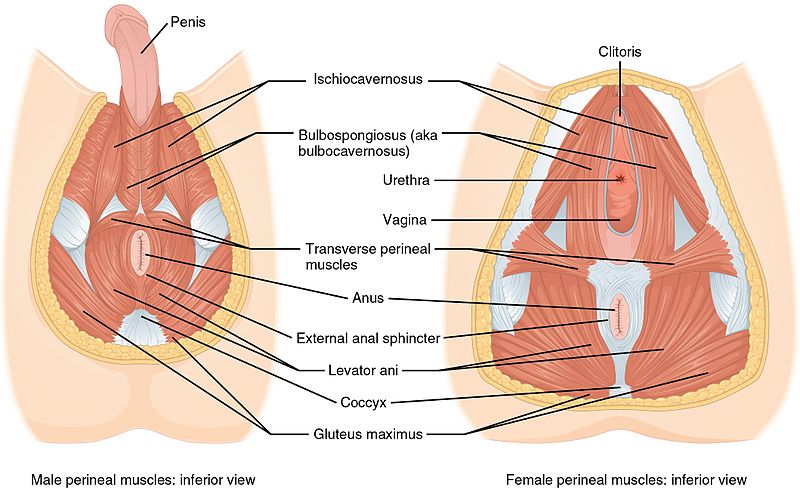
The pelvic floor is a phrase used very frequently here on the blog as well as in our clinics, but to those unfamiliar with this area of the body, it may still be this illusive mystery. I want to break down the pelvic floor into each of the muscles it is comprised of, in order for you to get a better grasp of what’s going on down there.
If you are partial to 3D visuals and videos, you can Take a Tour of the Pelvic Floor.
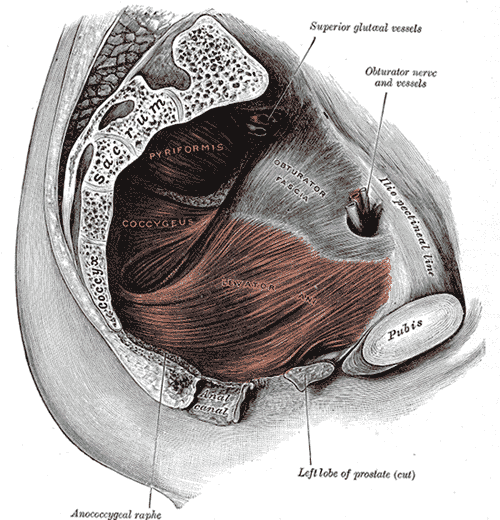
The pelvic floor is comprised of multiple layers of muscles that close off the bony frame of the pelvic outlet and are key in supporting the pelvic organs. To quote from our previous blog post: A Cock in the Hen House: A look inside the Male Anatomy, “Although the external anatomy is different, all the other internal muscles that make up the pelvic floor are the same for men and women. The muscles sit in the pelvis like a muscular bowl, providing support to the organs of the pelvis and assisting in bowel, bladder, and sexual function. In women, the pelvic floor supports the uterus, the bladder, and the colon. In men, the pelvic floor supports the prostate as well as the bladder and the colon.”
First let’s discuss the bones that make up the pelvis/pelvic girdle. The pelvic girdle is a basin-shaped ring of bones connecting the vertebral column to your femurs. The pelvic girdle contains and protects the pelvic organs and allows for attachment of the pelvic floor muscles.
The pelvic girdle is comprised of:
- Ilium: the largest pelvic bones – when you put your hands on your hips you are touching the ilium.
- Ischium: the part of the pelvis that you sit on (aka sit bones).
- Pubis: the front part of the pelvis that joins both sides together via the pubic symphysis.
- Sacrum: the sacrum attaches to the ilium via the sacroiliac (SI) joint.
- Coccyx: also known as the tailbone, and attaches to the lower part of the sacrum.
Now that you have some reference material, let’s go through each muscle one by one:
- Bulbospongiosus: in men, this muscle runs along the underside of the base of the penis and forces blood into the penis during erection, and aids in ejaculation. In women, this muscle runs from the clitoris to the perineum along each side, constricts the vagina, and forces blood into the clitoris.
- Ischiocavernosus: attaches from the pubic symphysis to the ischial spine on each side, and forces blood into the penis and clitoris during erection.
- Superficial & Deep Transverse Perineal: this muscle has superficial (thinner band) and deep (broad) fibers that run underneath the perineum – the space between the anus and vagina (in women) or base of penis (in men). Supports the prostate and vagina.
- Ischiococcygeus (aka Coccygeus): attaches from the tendinous arc of the ischial spine to the lower sacrum and coccyx. Moves the coccyx forward and supports the pelvic viscera.
- Levator Ani is a group of muscles (highlighted above in red) comprised of:
- Pubococcygeus: attaches from the pubis to the lower sacrum and coccyx.
- Iliococcygeus: connects with pubococcygeus muscle and attaches to the coccyx.
- Puborectalis: wraps around the rectum to form a muscular sling.
- External Anal Sphincter: attaches to the tip of the coccyx and surrounds the anal canal. This muscle closes the anal orifice.
- Obturator Internus: attaches from the pubis and ischium to the femur, helps to turn your hip outward (lateral/external rotation). *Fun fact: tightness and/or trigger points in this muscle can refer pain to the coccyx/tailbone.
- Piriformis: muscle deep in the buttocks (underneath gluteals), attaches from the sacrum to the femur, also works to rotate the hip outward (lateral/external rotation). Tightness in this muscle can be linked to sciatica (nerve pain down the back of the thigh), due to its proximity to the sciatic nerve.
Whew! That was a lot of information to get through! Now that you have a better understanding of what the pelvic floor looks like, let’s go over some ways this complex area of the body may lead to pelvic floor dysfunction in men and women.
Pelvic Pain
- Vaginal/penile/scrotal/perineal or anal pain
- Tailbone/sacroiliac joint/pubic symphysis pain
- Pain that interferes with sitting and exercise
- Pain that radiates to the abdomen/buttocks/thighs
Urinary Dysfunction
- Urinary urgency, frequency, and hesitancy
- Urinary retention
- Pelvic organ prolapse & incontinence
- Decreased force of urinary stream
- Pain/straining with urination
Bowel Dysfunction
- Constipation
- Fecal Incontinence
- Pain/straining with bowel movements
Sexual Dysfunction
- Pain with intercourse/penetration
- Pain post ejaculaton
I hope this helped to give you a better understanding of the pelvic floor anatomy.
References:
- Carriere B, Feldt CM. The pelvic floor. Germany: Georg Thieme Verlag; 2006.
- Netter FH. Atlas of human anatomy. 6th ed. Philadelphia, PA: Elsevier Inc.; 2014.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.