
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
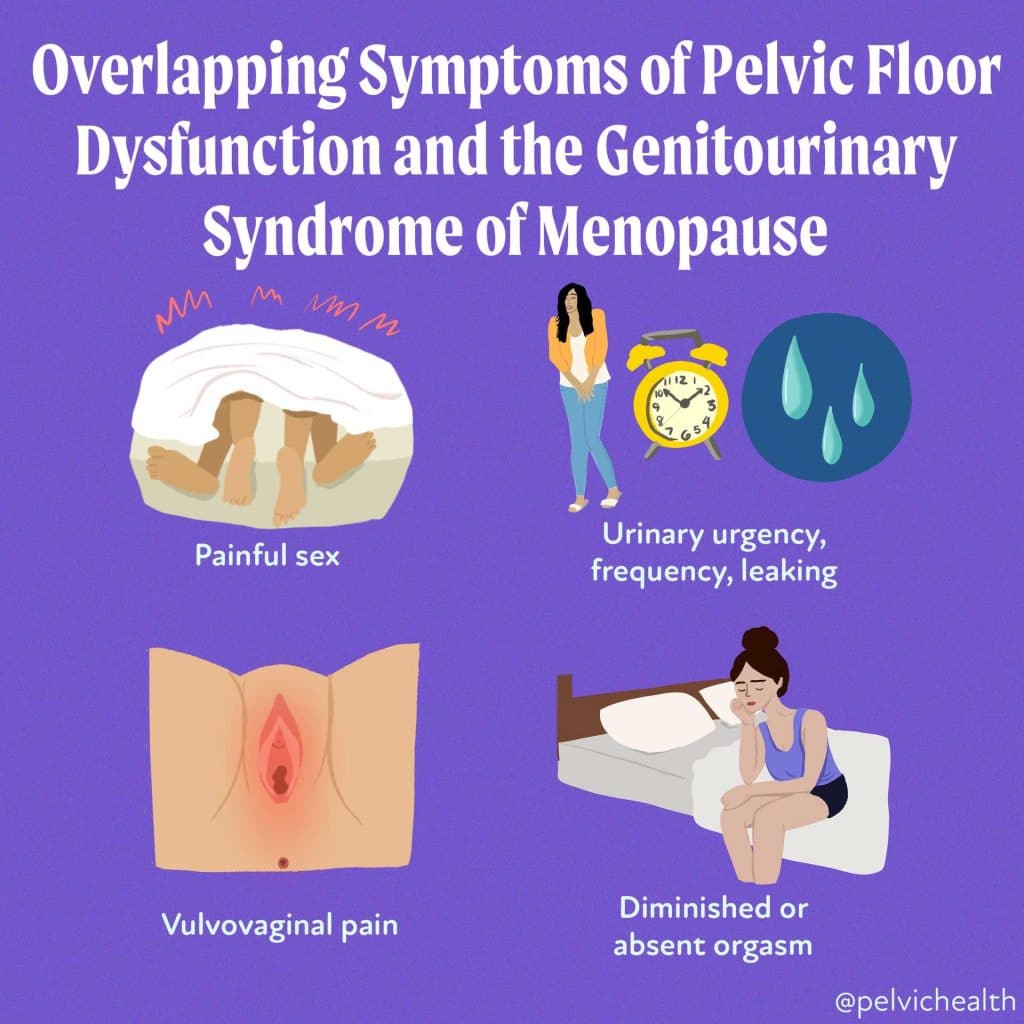
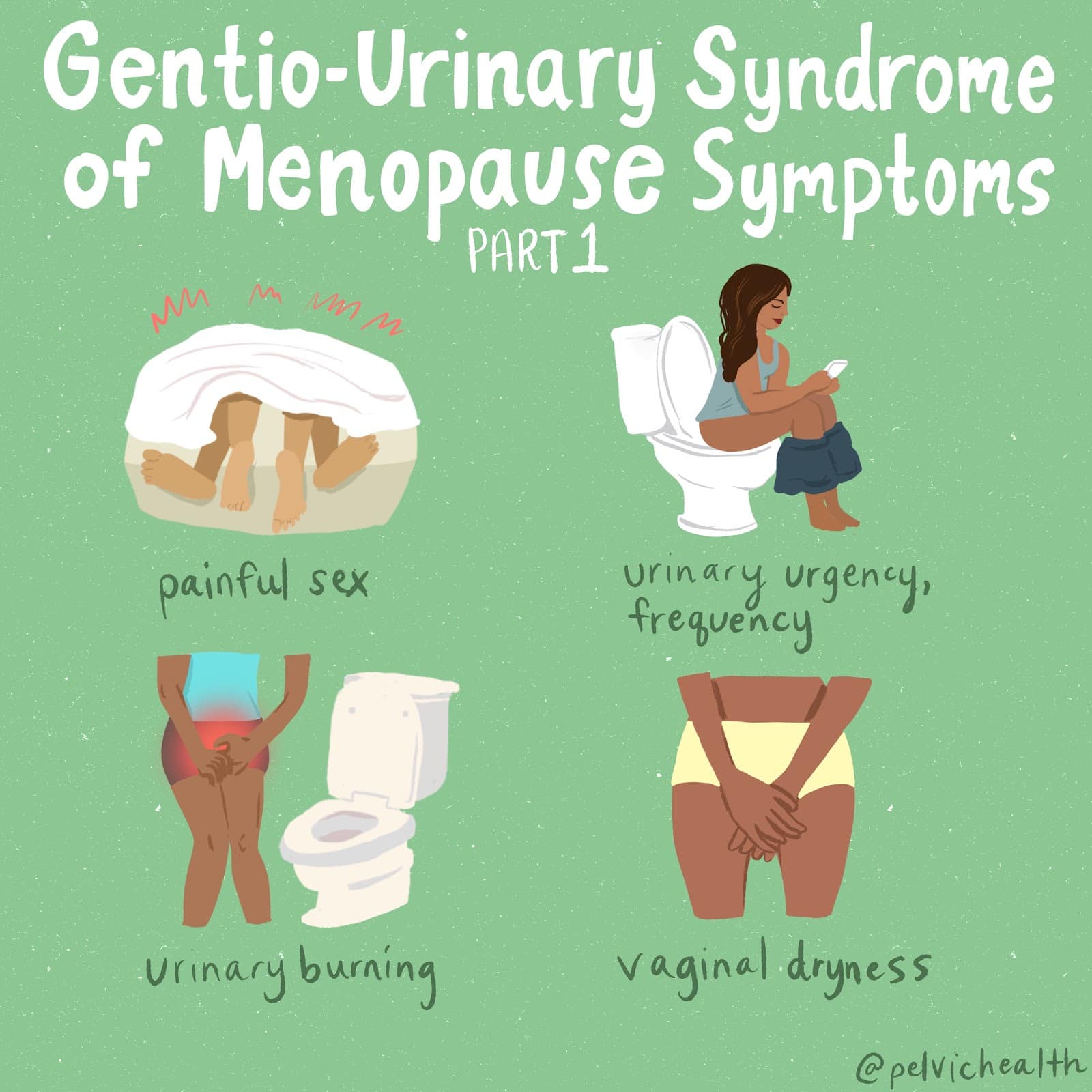
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting
An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.
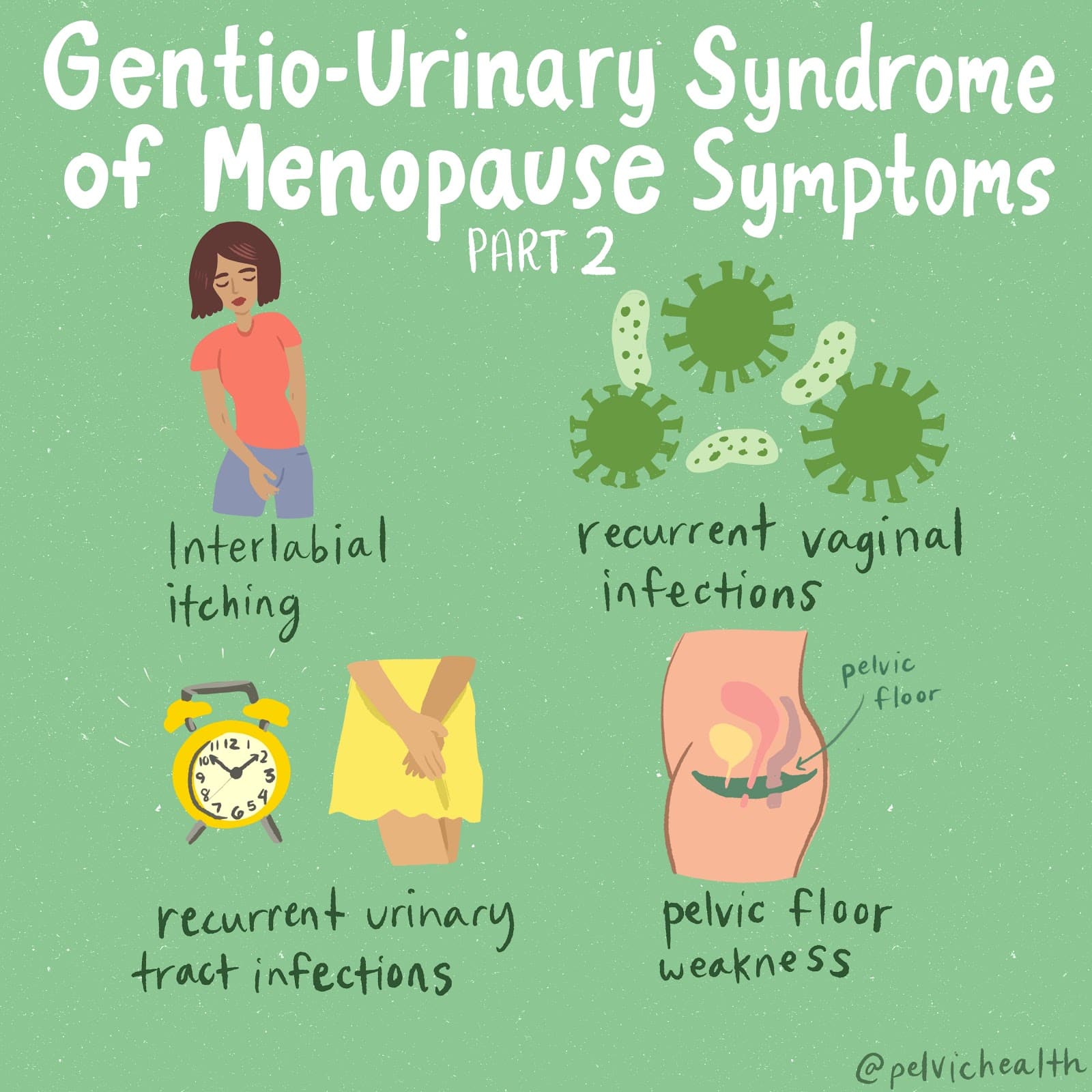
Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Rachel Gelman, DPT
“ Let’s just start with the word vagina. Vagina. It sounds like an infection at best. Maybe a medical instrument. ‘Hurry, nurse, bring me the vagina.’ Vagina. Vagina. It doesn’t matter how many times you say the word, it never sounds like a word you want to say. ”-Eve Ensler, The Vagina Monologues
There are many reasons why I think women have insecurities about their genitalia, but this quote in particular speaks to one reason; vagina is a weird word. No one wants to say it. It becomes like an anatomical Voldemort, the body part that shall not be named. So, when no one wants to say the word, no one wants to talk about it. Without healthy conversation, women are left misinformed. In fact most people do not realize that the area they are referring to is technically not the vagina, but the vulva. Today, I am here to encourage you to grab a mirror, and take the time to look at your vulva.
A majority of my female patients tell me they have never looked “down there.” Many express concerns that their genitals look “bad” or “wrong.” I always find it interesting that my male patients never report concerns about the appearance of their penis. In fact, many of my male patients have given me in-depth descriptions of their genitalia. I always think how impressive it would be if one of my female patients could describe her labia with such accuracy. Obviously, men are at an advantage as the penis is external and easier to check out on a daily basis. However, there is still a level of shame or insecurity surrounding the vulva. There is the obvious history in our culture that has led to this, especially during the Victorian Era, which founded the idea that women should not be sexual beings, and that their genitals are meant to be kept private. One could also look at the impact of pornography and the recent rise in labiaplasties as a contributing factor into why women worry that their genitals don’t look “right”. Now, I think pornography can be a great tool to spice up a relationship, but it should not be used as a way to judge a typical body type. Porn is basically an X-rated Hollywood. When someone worries their genitals do not look the same as an adult film star, it is equivalent to saying, “My face doesn’t look like Angelina Jolie on the cover of Elle!” It is just not a realistic expectation. Women should start to see this part of their body as they would any other physical feature; as something unique to only them. It should be a source of confidence, not discomfort or embarrassment.
I will step down from my feminist soap-box, and now tell you why it is important for your health to look at your vulva. As a woman, your body will go through many changes thanks to hormonal fluctuations that come along with puberty, pregnancy and menopause. Therefore, it is important to be aware of what your “normal” is regarding your genitals, so that you can monitor if any changes occur as you age. Also, there are some dermatological conditions, cancers, STDs and side effects of certain medications that if caught and treated early can be no big deal, but if left unchecked can turn into a bigger issue.
You can also think of this as an opportunity to become friends with your vulva. Even if you just become acquaintances, the more you “get to know” your body the better you will begin to feel about it. That kind of confidence can help with your overall self-esteem and can improve your sexual function. You should know your body best and take pride in it’s uniqueness.
So, what should your vulva look like?
Your vulva should have a few keys parts:
- A mound of fatty tissue, usually covered in pubic hair known as the mons pubis
- Two outer skin folds which are known as the labia majora
- Within the labia majora are a smaller set of skin folds known as the labia minora
- At the top, which can be considered 12:00 if the vulva was a clock, is the clitoris, under the clitoral hood
- Below the clitoris, is the urethra, the opening where one urinates from
- Below that is a larger opening, the vagina, that leads to the vaginal canal
- Directly below the vagian is a small patach of skin known as the perineum
The appearance of a woman’s vulva can vary from person to person. There has been a lot of research over the years that supports the fact that there is no “normal” standard regarding female genitalia and, even more, the data collected shows that the dimensions of a woman’s vulva can vary from person to person. Some women’s labia majora and minora are the same size, while other women’s labia minora are bigger than their labia majora. There are many variations, which is why I often tell patients that their vulva’s are snowflakes, each unique in their own special way. So next time you have a moment alone, grab a hand mirror and say “hello” to your vulva. Try to identify the different structures listed above and take note of what your vulva looks like. Are there any moles or markings on the skin? Notice if there is any discoloration of the skin or tissue of the vulva, especially if this is new for you and you are having other symptoms such as pain with intercourse, itching, difficulty with urination etc. Also, vaginal discharge can be normal but contact your doctor if the discharge is any of the following: green or dark yellow, foamy, has a strong odor, or there is a change in the amount or consistency. Try to make a vulvar self-examination part of your health routine, as you would a self breast examination. However, just like brushing your teeth everyday does not replace a trip to the dentist, a vulvar self-examination should not replace your annual trip to the gynecologist.
Hopefully this post has inspired you to bust out your hand mirror and take a peek, but if you are still unsure or maybe just want to read more, I suggest you check out the following sites (some may be NSFW):
http://www.ourbodiesourselves.org/health-info/self-exam-vulva-vagina/
http://www.labialibrary.org.au/
http://101vagina.com/about/vagina-vs-vulva/
http://deconstructingtheidealvulva.tumblr.com/
https://pelvicguru.files.wordpress.com/2015/03/exploring-your-genitals-1.pdf
Readers we want to hear from you! How well do you know your vulva? Please share in the comments section below!
And if you haven’t already, SUBSCRIBE to this blog (up top, to the right, under Stephanie’s photo!), so you can get weekly updates in your inbox, and follow us on Facebook and Twitter where the conversation on pelvic health is ongoing!
Rachel Gelman, DPT
is a Bay Area native, and currently practices in our San Francisco office. She received her bachelor’s degree in Biology from the University of Washington in Seattle and her Doctorate in Physical and Occupational Therapy from Samuel Merritt University. Rachel grew up dancing and is excited to have recently returned to the dance studio. Outside of dance, Rachel enjoys going to the gym, discovering new brunch spots and spoiling her adorable niece and nephew.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
Vaginal yeast infections aka candidiasis, are an uncomfortable and common issue that many women find themselves dealing with at some point. Three out of four women will experience at least one vaginal yeast infection in their lifetimes-many will experience two or more. If you’ve had one you know that the symptoms can be enough to drive you crazy:
-severe vaginal/labia itching
-burning during intercourse or urination
-genital redness/swelling
-sometimes (but not always) you will see a thick, white discharge *think cottage cheese*
If you are experiencing any of these symptoms and have not gotten checked out by your doctor-do it. A simple yeast infection can be easily treated by an over the counter or prescription antifungal. Here is what happens when we get a yeast infection:
Candida albicans-a fungus related to yeasts that are common in many of the bread products out there-is the most common type of yeast that we find in and on the human body. When balanced the candida albicans and other microbiota that reside in and around the vaginal canal work together to maintain a healthy environment. However, sometimes situations can go awry and the yeast is able to overproduce. This often leads to a full blown infection and an onset of the symptoms listed above.
The most common causes of a yeast infection are:
-Antibiotic use. Antibiotics not only kill the “bad” bacteria that is being targeted, but they virtually destroy all of the good bacteria that we have developed in our intestines and vagina. The good bacteria keep yeast from growing from their normals levels to infection status.
-Hormonal changes such as pregnancy, hormonal contraceptives, and right before menstruation will change the pH of the vagina, making it a more ‘hosptible’ enviornment for yeast to proliferate.
-Douching and/or inadequate lubrication with sexual activity
-Finally anything that compromises our immune system, such as diabetes, AIDS, cancer, stress, a poor diet, and lack of sleep
If you have any of these symptoms and are dealing with one or more of the above common causes of a yeast infection, I encourage you to get evaluated by a medical professional. Yeast infections are no picnic, but when diagnosed and treated properly they can resolve pretty quickly.
Now that we’ve covered the basics of a typical yeast infection, let’s talk about something that we deal with on a daily basis at PHRC: What happens when you have the symptoms, tested positive for yeast, treated it, but nothing changes? Or, what if you are feeling all of these symptoms, but you doctor was unable to find anything wrong?
Here is what could be going on:
It could be that you had a yeast infection and because a yeast infection is exactly what it sounds like-an INFECTION-your body is going to do whatever it can to protect you against this threat. Your pelvic floor muscles will, outside of your awareness and control, tighten up causing myofascial trigger points, pudendal nerve irritation, and connective tissue restriction. Even though you have taken the antifungal-your pelvic floor muscles may not have gotten the memo and are continuing, though ineffectively, to try to protect you against what it thinks is impending doom. So we have pain, itching,and redness caused by an initial yeast infection, followed by pain, itching, and redness due to our muscles being tight. This then reduces blood flow to the area, irritates the nerves and tissue, and thus becomes a safe harbor for inflammatory chemicals** to camp out. So begins the cycle of pelvic floor muscle dysfunction following a yeast infection.
In the other scenario-you are experiencing the completely maddening symptoms that are so famously associated with a yeast infection, but you go to the doctor and they find nothing. In this case, they will often write you a prescription for an antifungal anyway just in case it is a less common strain of yeast causing the infection (requires a wet mount of vaginal discharge to determine, so not always done initially). You take the antifungal, nothing happens, and you are about to check yourself into the nearest mental health facility because you are losing your mind over the vaginal/vulvar itching, pain, redness, and swelling. *Personal note: I have been this person and it was all I could do to make it into the office and keep my pants on.
What this might be is an onset of myofascial pelvic pain/dysfunction that is basically mimicking a yeast infection. Because the muscles, nerves, and tissues in the pelvis are in charge of performing so many different functions, our proprioception (awareness of how our are body parts are positioned in space) in this area can easily be way off. So if you are the type of person that runs the risk of getting pelvic floor muscle pain/dysfunction, what feels like a yeast infection may in fact be nothing of the sort.
In the 2015 Guideline on Vaginal Candidosis, Mendel reports “Although itching and redness of the introitus and vagina are typical symptoms, only 35-40% of women reporting genital itching in fact suffer from vulvovaginal candidosis.”1 In other words about two thirds of women reporting vulvovaginal itching don’t actually have a yeast infection! By the time someone with this type of presentation makes it into our office they have likely been through quite a few pelvic exams, swabs, antifungals, or home remedies. Not only is the majority of the general public underinformed when it comes to this issue, but a lot of the medical community may not know much about this either.
When you are evaluated by one of the PHRC therapists for this issue we will want to know the background. The who, what, when, where, and why, as it were. Then we will want to look at you objectively. The main areas of concern for us will likely be the adductors, the vulvar and perianal connective tissue, the pudendal nerve, and the deep and superficial pelvic floor muscles. If you are still also experiencing infections we will also work with your medical team or help you find a team that will help get the infections under control once and for all while we treat the musculoskeletal consequences in physical and occupational therapy. (Check out this blog post for a better idea of what a typical first appointment for pelvic floor physical and occupational therapy will look like.)
The bottom line is that if you are experiencing some or all of the symptoms that I have listed in this blog post (vaginal/vulvar pain, itching, redness, and swelling) and you have been through all of the first line steps but are STILL having issues, get evaluated by a physical and occupational therapists that specializes in pelvic floor dysfunction. Your symptoms may not actually be a yeast infection, but may be the pelvic floor muscles masquerading as such. Here is a link with some tips to find a pelvic floor physical and occupational therapists in your area.
Readers we want to hear from you! What are some of your experiences with yeast infections? Please share in the comments section below!
And if you haven’t already, SUBSCRIBE to this blog (up top, to the right, under Stephanie’s photo!), so you can get weekly updates in your inbox, and follow us on Facebook and Twitter where the conversation on pelvic health is ongoing!
** One of the main inflammatory chemicals hanging around in this situation are histamines. Sound familiar? As in anti-histamine…as in benadryl? Histamines are famous for causing redness and itching.
- Mendling W1. Guideline: Vulvovaginal Candidosis (AWMF 015/072), S2k (excluding chronic mucocutaneous candidosis). Mycoses. 2015 Mar;58 Suppl 1:1-15. doi: 10.1111/myc.12292.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
This week writer Jackie White, writer, educator, and creator of the website Sexual Healing, shares her colorful story and essay on pelvic pain. Growing Pains: A Story of Sex, Vaginsmus, & Clinically Approved Dildos
Not Just Another Blog Post, Folks…
Back in September 2014, the North American chapter of World Sexual Health Day announced that my personal essay “Growing Pains: A Story of Sex, Vaginsmus, and Clinically Approved Dildos” had won their first ever writing contest. Though I try to incorporate my own first-hand experiences into these blog posts, the main purpose of Sexual Healing has always been to communicate info that women in pain might want to know or consider. However, this personal essay had an entirely different goal in mind. I wanted to tell my story in a humorous way, while linking it back to the way society treats female sexuality as a whole. In fact, the content of this essay is far more personal than even the most embarrassing anecdotes I’ve shared with Sexual Healing readers.
So why am I sharing it on Sexual Healing? Of course, it could be of interest to those who want to know a little more about my early years with pelvic pain, or those who are preoccupied with the way women internalize society’s simultaneous adoration and disdain of the female form. But my reasons delve a bit deeper than that. I hope that this essay will somehow relate to women who are struggling with sexual pain, wrestling with their self-image, or trying to discover what it means to be a sexually secure person. Lofty goals, I know, but it rarely hurts to be too ambitious. You can find my personal essay below or check out the PDF version here.
Growing Pains: A Story of Sex, Vaginsmus, and Clinically Approved Dildos
Everyone endures their fair share of sexual growing pains, but mine were especially agonizing and embarrassingly unique. While other freshmen girls were discovering the pleasurable powers of shower heads and the joys of fucking your boyfriend while your roommate was at her afternoon Anthropology class, I was popping pills and deep breathing to relaxation tapes. My body felt like an awkward, lumpy prison – as it does to most women in their late teens – but I wasn’t boosting my self-image by taking suggestive selfies or spreading my legs at a mirror to examine the mollusk folds of my vulva. Filling the gap between the glistening goddesses I saw spread across glossy magazines and the body I touched alone in the shower was a much more elaborate process for me. Ultimately though, I do believe that it was a more rewarding one.
—
After I changed into my bare-ass dressing gown and had my feet up in metal stirrups, I realized that my new GYN bore a disturbing resemblance to my ex-boyfriend’s father. I’d been trying to pinpoint why he looked familiar just a few minutes earlier as I listened to him talk in his office, but the reason had escaped me. I wished I hadn’t figured it out.
A nurse stood in the corner of the room to supervise – a bubbly, walking indemnity for the practice – as the doctor shoved the speculum in my vagina. She tried to talk to me about school and the poems of William Wordsworth as the doctor shined his headlamp towards my crotch, peering into the cave between my legs like an old coal miner. I gave her halfhearted replies, trying to relax my muscles as they struggled against the speculum.
Following the regular exam, I was poked and prodded with needles for what seemed like a small eternity. As asked, I rated the pain 1 through 10. My distress grew as the process pressed on, anxiously waiting for the agonizing electric shocks to run through my pelvis. What place did such a subjective rating system have in a doctor’s office, anyway? I pictured all the charts and graphs and empirical sheets that my nurse mother had complained my entire life. Where was all the empirical information and blood work? Though I’d been told that this doctor was one of the top GYNs in the country, I felt my hopes falling by the minute.
When we finished the exam, I changed back into my clothes and returned to the doctor’s office. It was strange to listen to someone describe your own body to you, as though you hadn’t been living inside the thing your entire life. He explained that a damaged Pudendal nerve was responsible for the agonizing stabbing sensation I felt every time I was penetrated. He had no way of telling whether the nerve was permanently damaged or being constricted by tense muscles. In one sense, hearing this explanation was a relief. My first GYN – a chronically indifferent nurse practitioner with small hands – had insisted that I either had an STD, deep-seated psychological hang-ups about sex, or simply wasn’t getting wet enough (apparently I didn’t know what foreplay was). But when my tests came back negative and her impassioned Astroglide recommendation hadn’t done the trick, she simply shrugged her shoulders and pushed me off on a pelvic pain specialist.
Of course, this sense of triumph over the incredulous nurse practitioner was quickly replaced by pure dread. The doctor thought the nerve was the source of my troubles, but he wasn’t exactly sure why. I had no name to match with my problem, nor a streamlined treatment plan. Until we discovered the exact origins of the problem, he was simply going to throw every possible remedy and experimental treatment at me until we began seeing improvements. The only solid diagnosis he could give me was a disorder that went by the rather Victorian name “vaginismus,” meaning that the nerve pain was causing my vaginal muscles to involuntarily tense up for self-protection. He told me that I’d probably be able to have penetrative sex again, though the word “probably” had the strongest presence in that statement to me. When I asked him how long I’d have to wrestle with this problem, his answer devastated me: “Most likely the rest of your life.”
Being a pessimistic person by nature, I initially walked out of that office feeling worse than when I walked in. I didn’t have a name for my disease or a shred of hope that I would ever enjoy a penis inside of me again. All I had to show for my appointment was a prescription for some archaic anti-depressants. Supposedly this medication was now used for chronic pain and insomnia, since the psychiatric world had since moved on to bigger and better things like Zoloft and Prozac. The self-loathing voice in my head whispered that these were just phantom pains conjured up by my mind like my previous GYN had suggested, that the new doctor was just trying to handle me with kid gloves and passively remedy a mental problem. Of course, doing such a thing would be highly illegal, but my anxiety rarely listens to rationality.
Regardless, the idea of taking anti-depressants certainly didn’t thrill me, but I was willing to try anything to get my sex life back to normal. In time, I did discover that the medication dulled the stabbing pains that plagued my vagina. Unfortunately, my muscles still made penetration an ordeal and left me with a terrible burning sensation afterward. The medication wasn’t without its downsides either. After a few weeks of consistently taking the meds, I found myself devouring everything in sight – particularly sweets, something I usually abandoned in favor of saltier snacks – which only enhanced my college freshmen 15.
The irreverent attitude I had towards taking pills on time didn’t help matters. The first day I forgot to take my pill, I woke up in the middle of the night unable to move, listening helplessly as people dug through the closet at the foot of my bed. They whispered that I had nothing valuable for them to take, that they were just going to rape me and slit my throat. These night terrors about menacing presences in my bedroom – far more terrifying than any illegal drug I’ve ever experienced – inspired me to stick to my pill schedule. Still, I began to question whether the side effects of this drug were worth the slight relief it gave me.
For the next few weeks, I spent my nights laying awake in my bed feeling sorry for myself. The muffled sounds of R&B hits emanating from my roommate’s headphones served as the background music to my despair, my world’s tiniest violin. I always considered myself an incredibly sexual person, and – though I didn’t believe in a higher power – I felt that I was being punished. It all seemed so unfair. For God’ sake, I’d been touching myself since I was 5 years old! I remember having my first orgasm before I’d entered the double digits. Why did the pain have to be so mysterious? I’d also read somewhere that vaginismus was usually reserved for the extremely religious and guilt- ridden. Why was this happening to me?
The doctor had also suggested physical and occupational therapy to ease my muscular problems, but I had avoided going, hoping the meds would serve me a quick n’ easy solution on a silver platter. Of course, when I returned to the doctor complaining that the meds hadn’t magically poofed my pain away, he gave me a very professional reality check. He calmly explained that the meds simply treated the nerve pain symptoms, but was doing nothing to actually repair the nerve or counteract the vaginismus. If tense muscles were constricting the nerve and causing the pain, then physical and occupational therapy could possibly get rid of my problem altogether. If nothing else, my vagina wouldn’t be inviting a penis back in anytime soon unless I trained my muscles to relax and stop associating sex with discomfort. Either way, physical and occupational therapy was an essential part of the healing process.
As he explained all this to me his voice sounded like a taut string being plucked. He had a condescending undertone that was honestly much deserved. I’d been handed the possible solutions to my problems – something that many women with these issues never get – and then threw it away because it wasn’t conducive to my lifestyle. That visit marked the beginning of a real treatment plan that I’d actively participate in, rather than a few pills popped before bedtime.
My first visit to the physical and occupational therapists’s office immediately made me feel self- conscious, not that this was a particularly difficult feat at the time. The practice specialized in pelvic therapy and as I sat in the waiting room, I realized that I was the only patient there under the age of 50. In my mind, only old people got sick and the apparent demographics of the practice only confirmed my misconception. I’d hoped to see other girls like me, but sitting in that waiting room made me feel like a defective product thrown off an assembly line.
My physical and occupational therapists was a petite red head with three young boys and a soothing voice. Occasionally I’d see her leave the practice on my way out, her fiery hair and sharp face peeking out from behind the wheel of her gargantuan white escalade, looking a little overwhelmed at prospect of wielding the beast. Initially, we discussed my issues with penetration as she gave me a preliminary exam, testing the severity of my muscle tension. I reclined on an artificially warmed bench as she placed a pair of gloved fingers inside me, putting pressure on muscles I didn’t even know I had and asking me which ones hurt the most. Meanwhile, I tried not to think about what a weird porn scene this would make. Luckily it was far too clinical to be sexy. The power of context is truly awe-inspiring.
After I got dressed again, she sat me down and began asking me questions. Gently, she asked me what my home situation was like and how I was raised to view sex. I thought about an instance where my mother – young herself at the time – had caught me masturbating as a child and warned me never to do it again. By nature I sought approval from others, so for a long time I stopped touching myself and when I did cave in to the desire, I felt incredibly guilty about it. I chalked my mom’s reaction up to confusion. After all, my parents weren’t exactly puritanical. They were agnostics who’d conceived me out of wedlock and didn’t hide the more sexual part of their relationship from me. I saw glimpses of intimacy between them throughout my childhood, the occasional passive
touch that suggested they still enjoyed a good romp in bed when I was out of their way. Surprisingly, I found all of these thoughts marching their way out of my mouth like a line of little soldiers. The physical and occupational therapists treated them with quiet interest, nodding and taking a few notes.
“This next question is completely optional, since I’m not a licensed therapist or psychologist. If you don’t feel comfortable telling me it’s fine,” she began, making me slightly nervous. “Have you been sexually abused or assaulted?”
I paused for a moment. I thought about the previous year, when one of my boyfriends and I were alone in his bedroom together. He’d put his face to my neck, kissing tenderly, but I was far too absorbed in my stresses about work and school to think about having sex. Despite my numerous protests, he’d pushed me down on the bed and hiked up my skirt. My physical resistance was minimal – nothing above some light pushes – but as he moved above me, I fought between feelings of betrayal and guilt.
He’d stopped when he saw me crying and held me on the edge of the bed with tears in his eyes when he’d realized what he’d done. He’d told me it was misunderstanding, that it would never happen again. It didn’t. But I thought about the sourness our relationship took on after that and the unexplainable pain that appeared only a month or two afterwards. I thought about his sincere tears of apology and – for reasons I’ll never quite understand – I felt that I had no right to call it rape.
“No. I don’t think so,” I replied. Her eyes hovered over me for a moment, but she pursued the issue no further.
During our next session, she placed a small sensor into my vagina and hooked me up to a biofeedback machine, which digitally measured my muscle tension and charted it on a graph. She looked at my chart with knitted brows, informing me that the normal levels were around a 1 or 2. I watched the red line on the graph move with the passing seconds, measuring every movement my pelvic floor muscle made. My line hovered between a 7 and 8.
In light of the tests she’d performed and the questions she’d asked, she theorized that my muscle tension came from a combination of two things: fear of penetration due to the nerve pain and pure stress. “Some people hold anxiety in their necks and backs, you hold stress in your pelvis,” she’d said. The idea seemed strange initially, but when I thought about how often I critiqued myself to death or worried about completely irrational things, I decided that her postulation was totally feasible. When I asked her if it could be easily treated, she smiled.
“Perhaps not easy, but certainly within reach,” she’d said.
This was the beginning of a strange professional relationship like no other I’d had before or since. Had we been the same age, I doubt we would have hung out together, but she was easy to talk to and I felt like I could openly discuss sex with her without fear of judgment. I told her about what boys I was chasing at the time and which boys were chasing me. I’d give her pain updates when I’d have a chance encounter. Of course, her kindness extended beyond the simple act of listening to my trivial escapades. She was incredibly considerate of the many anxieties I had. The idea of having hands in my crotch doing whatever they pleased made me uneasy, so she’d let me know exactly what she was doing as she went.
The days passed in measures of pressure points: “6 o’clock, 7 o’clock, 8 o’clock…” she’d say, keeping me updated on which vaginal muscles she was hitting with her latex-clad finger. 6 o’clock was the worst one, the one that I’d tense in anticipation of, the one that still gives me the most shit today. When I read my clock in the early evenings and see the dreaded time, I grimace slightly. A year later I would have a terrible acid trip where I was caught inside the time 6 o’clock forever. The intense connection between the sexual and the mental is astonishing, when you think about it.
That broken feeling I’d had my first day in the practice lobby slowly faded. I actually began arriving 10 minutes before my appointments to chat with the nurse at the front desk, admiring her tattoos and carefree attitude. The daily routines of muscle stretches, vaginal exercises, glute massages, and even the simple act of spreading my legs at a stranger began to reset the relationship I had with my body. As instructed, I carved ten minutes out of every day to listen to self-help relaxation tapes while holding a dilator – clinically approved plastic dildos in varying sizes – inside of me to stretch the pelvic floor muscle and build a positive association with penetration again. As the weeks pressed onward, I found the muscle tension number on the biofeedback machine descending in tandem with my pain. When my line finally reached a 2 on the graph, I was told that I could continue to maintain these levels on my own and was released from their care.
Up until that point, that physical and occupational therapy office was the only place that didn’t make me feel ashamed of my sex life or my body. Pills dulled my sexual pains, but they couldn’t combat the disdain I had for my body, my beastly anxiety problems, or my inability to trust others to interact respectfully with my body. Though I’d been having sex for years, I don’t think I truly understood what it meant to be a sexually secure person before I set foot in that office. What does this say about the society we live in?
—
Fear and stubbornness chain people to their antiquated beliefs about relationships and sexuality. A vital part of this archaic prison is a code of silence surrounding sex. If you talk about it, you’re a pervert – slut in a woman’s case – at worst and inappropriate at best. But thanks to advancing societal attitudes towards relationships and the informative powers of the Internet, the word about sexual health, consent, and body acceptance is spreading louder and further than ever before.
Unfortunately, even this comes with its downsides. Concepts that are vital to sexual wellbeing have been reduced to buzzwords and catchy headlines that trendy magazines use to pull in readers. This only seems to make skeptics even more dismissive of these ideas. I’m not suggesting that this naturalization process isn’t essential, but I am suggesting that we change the dialogue around the way we approach the topic.
When people ask me why I am so passionate about sexual health, I try to explain to them that it’s not a matter of politics or spirituality, but rather a matter of health and wellness. I speak in concrete terms, like those charts and graphs I wanted so badly to see during my GYN exam. I tell them about my own sexual struggles – gory details and all – because ultimately it’s the only way people will listen. I tell them the mental barriers we have towards sex reveal themselves in strange ways, even physically. It’s funny, really. When something that creates so much hidden suffering actually begins to manifest itself out in the open – where it finally can’t be ignored – then people finally start giving it the attention it deserves.
Jacquelyn White is a freelance writer at JW Writes and the creator of Sexual Healing, a blog about overcoming pelvic pain, dyspareunia, and low self-image. When she’s not writing for clients or talking about vaginas, she can be found hanging out with friends or relaxing with a good book.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.



