Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Lauren Rogne, PT, DPT, PHRC San Francisco
The case of the mysterious pelvic pain – Exploring the clinical presentation of Chronic Pelvic Pain Syndrome (CPPS)
Background
Ben is a 35 year old with sudden onset of urinary tract-like infection symptoms, including urinary frequency, urgency, pain and burning. He visited his doctor, and his urinalysis came back negative for infection… but what could it be? About six months ago, Ben had transitioned from being a long distance runner to using a stationary bike at home more often for exercise. He also was sitting more for his job since COVID prevented him from going into the office as much. While working from home, he admits he is much more sedentary and there no longer is as much need to get up and go for a walk such as for a coffee break, or a walk with a coworker. Additionally, Ben reports he had COVID a few weeks prior to his symptoms beginning, and he was coughing quite a bit. Traveling also seems to aggravate symptoms. After discussing this more with his doctor, he was diagnosed with pelvic floor dysfunction, also known as chronic pelvic pain syndrome and was referred to pelvic floor physical and occupational therapy. His doctor also prescribed him an alpha blocker for the pain, which Ben reports was helpful. Unfortunately, this medication has resulted in a few fainting spells and difficulty orgasming. Ben’s goals for physical and occupational therapy are as follows:
- Treat pelvic floor dysfunction and return to a painless, normal function of my pelvic floor muscles
- Return to normal sexual activity
- Get off alpha blockers ASAP
- Learn how to improve my posture, exercise routine, and behaviors to prevent symptoms like this in the future
Objective findings
- Moderate connective tissue restrictions in the bony pelvis
- Moderate increased tightness in urogenital triangle muscles (ischiocavernosus, bulbospongiosus, deep transverse perineal muscle)
- Severe increased tightness at superficial transverse perineal muscle
- Moderate increased tightness at levator ani muscles
- Severe increased tightness of obturator internus muscles
- Limited ability to “drop” and lengthen pelvic floor muscles
- Poor ability to correctly demonstrate diaphragmatic breathing, primarily demonstrating chest breathing
- Moderate to severe myalgia at urogenital triangle
- Mild to moderate myalgia at levator ani muscles
Assessment, Plan, and Goals
Based on these findings, Ben would benefit greatly from pelvic floor PT to reduce myalgia and increased tightness of pelvic floor muscles, as well as improve connective tissue restrictions of his bony pelvis. He also would benefit from improving his motor control with diaphragmatic breathing and ability to lengthen his pelvic floor. His physical and occupational therapy plan of care consisted of patient education, manual therapy, neuromuscular re-education, and therapeutic exercise. He had a total of 17 physical and occupational therapy visits. We started with a frequency of once every two weeks, and then after six treatment sessions reduced frequency to once per month.
My goals for Ben were as follows:
- Pt will be independent with HEP in two weeks for better self management of symptoms.
- In four weeks, pt will demonstrate 10 diaphragmatic breaths without compensation to improve relaxation of pelvic floor.
- In six weeks, pt will present with 50% improvement in ROM with PF drops to improve relaxation of pelvic floor.
- In eight weeks, pt will report being able to sleep on his side without pain.
- In 10 weeks, pt will present with mild to no hypertonicity or myalgia of pelvic floor muscles to reduce pain with daily activities.
- In 10 weeks, pt will be able to safely discontinue the alpha blocker medication without increase in pelvic floor symptoms to meet his goals of not relying on this medication for pelvic floor pain management.
- In 16 weeks, pt will be able to tolerate sexual activity without provocation of symptoms.
Follow-up Sessions
Manual therapy
First, we needed to address the hypertonicity and myalgia in Ben’s pelvic floor muscles. He responded well to manual techniques including internal stretching of urogenital triangle, levator ani, and obturator internus muscles bilaterally, and we saw consistent improvements visit to visit. We also addressed his connective tissue restrictions in his abdomen, bony pelvis, and inner thighs using a technique called skin rolling. It was important to improve the mobility of these tissues to ensure adequate blood flow not only to these tissues, but also to the surrounding muscles and nerves.
Neuromuscular Re-education
Addressing deficits in motor control of pelvic floor lengthening and proper diaphragmatic breathing was crucial to improving the tightness and pain found in Ben’s pelvic floor muscles. Re-learning to breathe properly sounds like something we would never have to do, but it’s so common! We see this a lot in our patients. We have several accessory breathing muscles like our scalenes, sternocleidomastoid, and trapezius muscles, which all help lift up our chest when we’re breathing heavy. We do not need to use these muscles when we are breathing quietly throughout the day, but many of us get in the habit of using these all the time. The diaphragm is our biggest breathing muscle, so we should use it! When used properly, it works like a piston with the pelvic floor. As we inhale and our diaphragm descends, our pelvic floors descend and lengthen. Diaphragmatic breathing is a great way to bring movement and length to the pelvic floor muscles.
Patient education
Ben was waking at night with pelvic pain, solely when sleeping on his side. A simple tip of putting a pillow between his knees when laying on his side seemed to do the trick. We also discussed healthy sitting habits, best ergonomics when sitting, and the importance of getting up once every hour. We talked about the importance of proper breathing and the relationship of the diaphragm to the pelvic floor. This really helped Ben understand why we did so much breathing during our sessions and as part of his home program.
Therapeutic Exercise
We initially started with an emphasis in breathing and stretching to help improve the muscle pain and tightness found in the pelvic floor. I also had Ben use foam rolling as a way to address the connective tissue restrictions in his legs and bony pelvis. He responded great to these. Once symptoms had improved about 75%, we began progressing to more global strengthening to provide support for the pelvic floor muscles including gluteus muscles and abdominal muscles. This also would help us meet Ben’s goals of learning how to improve his exercise routine.
Outcomes
-normal tone of pelvic floor with mild increased tightness of urogenital triangle
-mild to no connective tissue restrictions of bony pelvis
-good execution of diaphragmatic breathing
-good pelvic floor drop during diaphragmatic breathing
-no longer taking alpha blockers
-sexual function returned to normal and no pain
-able to run three to four miles a few days per week without symptom aggravation
Discussion and Conclusion
There are many reasons why Ben could have developed his pelvic floor symptoms initially. We usually see the “perfect storm” with an onset of pelvic floor pain. Ben recently took up cycling, he was sitting more at work, and he was coughing a lot when he had COVID. Cycling can put a lot of compression on the pelvic floor and the pudendal nerve, the main nerve that controls the pelvic floor muscles. Sitting more for work or traveling can put more strain and compression on the pelvic floor as well; and coughing certainly puts more strain through the pelvic floor. All of these things likely had a compounding effect on one another, resulting in pelvic floor pain for Ben.
Ben had made significant progress after just six follow up sessions, but during re-examination, we continued to find increased tightness of his pelvic floor muscles. That is why we decided to continue with once monthly sessions to continue addressing pelvic floor impairments, but encourage more independence for Ben. Throughout this time, Ben experienced a couple of flare-ups. One was due to traveling to Europe, which involved a long flight and lots of sitting. Another involved more stress at work and prolonged sitting. Having monthly visits allowed us to work through these flare ups and give him more tools to self manage his symptoms in these times, as well as address tension that developed in the muscles and keep his pelvic floor healthy. We also were able to progress him as he was able to return to more difficult exercises like running three to four miles a few days per week!
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Stephanie A. Prendergast, MPT, Cofounder, PHRC Los Angeles
What are Tarlov Cysts? Tarlov cysts (a.k.a. perineural cysts) are cerebrospinal fluid-filled sacs found near the nerve roots at the lower end of the spinal canal, most commonly in the sacral spine area (the lower back and tailbone).
While it is not known exactly what causes these cysts, they have been linked to trauma from childbirth or injury, an abnormal separation of layers within a nerve root sheath, weakened vessels between nerve root filaments, dysfunction of lymphatic drainage and/or hydrocephalus.
Symptoms associated with Tarlov cysts can vary depending on their size and location. Some individuals may never experience any problems from them at all.
Common symptoms include:
- pain in affected areas such as the lower back or legs
- numbness or tingling sensations throughout a limb or body part
- muscle weakness or spasms in affected areas
- bladder incontinence
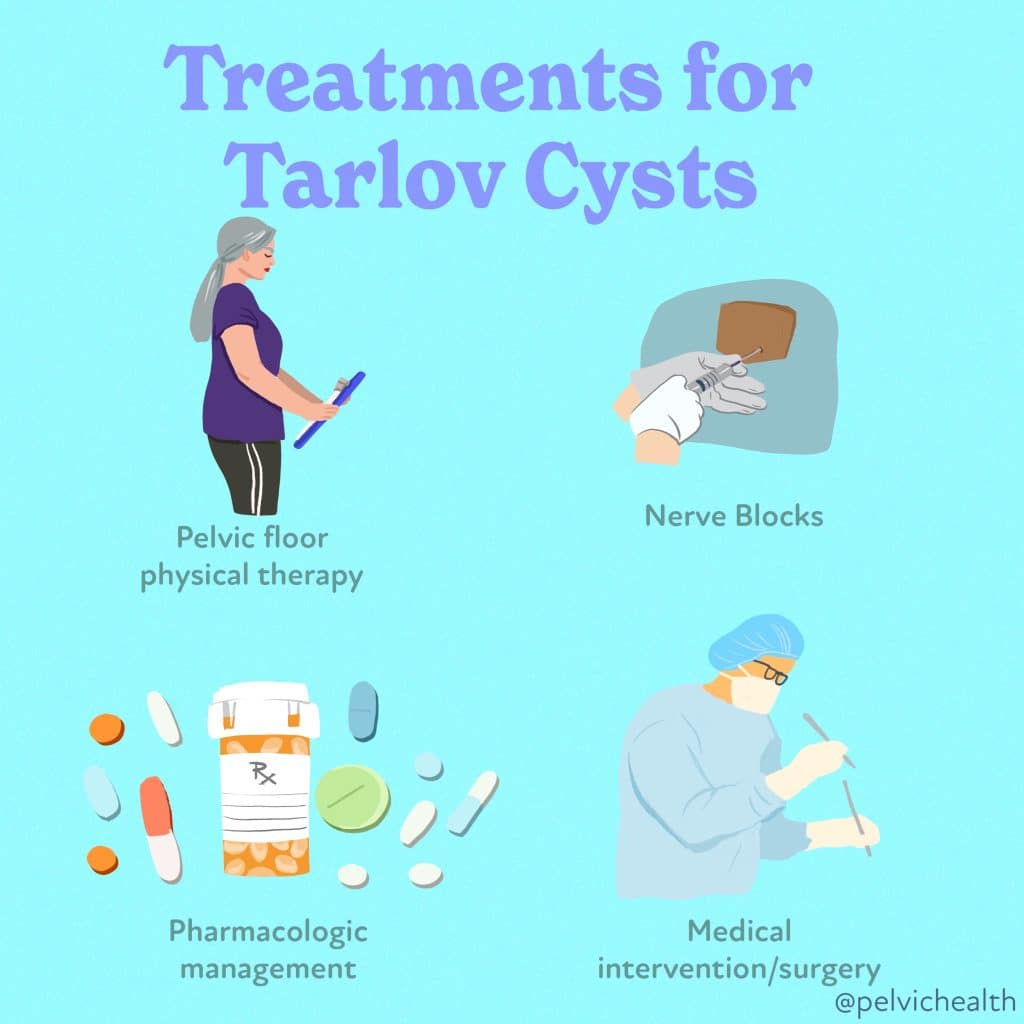
Treatments for Tarlov Cyst typically depend on severity and symptoms experienced.
Possible treatments include:
▪️ corticosteroid injections to reduce inflammation around radicular nerves
▪️ anticonvulsant meds to help manage any neurologic impairment due to irritation caused by expanded perineurals
▪️ PT or other interventions to improve posture and mobility
▪️ surgical resection if the cysts are causing severe compression.
Although Tarlov Cysts can cause significant medical complications, with proper diagnosis and treatment, individuals may be able to find relief from symptoms and regain their quality of life.
It’s essential for anyone suspected of having a Tarlov cyst to consult their healthcare provider for the best possible course of treatment. With prompt diagnosis and intervention, Tarlov Cysts may be managed successfully.
Tarlov Cysts Specific Resources:
Tarlov Cyst Disease Foundation: A non-profit foundation dedicated to research, improved diagnosis, and development of successful treatments and outcomes for symptomatic Tarlov cysts.
National Organization for Rare Disorders (NORD): rovides information about symptoms, causes, and treatments of Tarlov Cysts.
American Association of Neurological Surgeons: Offers an overview of neurosurgical techniques for symptomatic Tarlov cysts.
National Institute of Neurological Disorders and Stroke: Provides a comprehensive understanding of Tarlov cysts, patient support resources, and professional societies.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Melissa Patrick, PT, DPT, RYT , PHRC Lexington
For the estimated 15% of men worldwide who suffer from pelvic pain, finding the right providers to properly diagnose and treat their pain can be a daunting task, especially when seeking local options in their community. As a result, some patients end up traveling long distances to receive care.
Fortunately, the pandemic has brought about increased accessibility to virtual healthcare, offering a potential solution for those struggling with pelvic pain. Jim, a 57-year-old successful teacher, mentor, and writer, is one such individual who found relief through virtual healthcare. He had been dealing with a history of several diagnosed bouts of non-bacterial prostatitis since he was sixteen years old, with the first episode occurring after his mother’s passing.
During these bouts of prostatitis flare ups, Jim experienced varying presentations of pelvic pain symptoms, including pubic bone pain and penile discomfort. In November 2021, he faced a particularly severe bout of pelvic pain which also included testicular pain and a unique “binder clip” pinching sensation near his urethra, precisely where his pubic bone was located. This sensation became more pronounced after moving student desks in his classroom. Furthermore, Jim often felt as though he was sitting on a golf ball, and this discomfort was exacerbated while riding or driving in a car.
Medical literature suggests that roughly 8-12% of men will experience symptoms that mimic prostatitis at some point in their lives and that more than 90% of those men have symptoms that are consistent with chronic pelvic pain syndrome, also known as CPPS, which occurs due to causes other than the prostate, such as neuromuscular impairments (muscles, nerves, connective tissue).
In March 2022, Jim came across my therapeutic yoga services through the PHRC Youtube page. We ended up working together virtually for nine months over Zoom. I am happy to share that with the help of virtual healthcare, Jim has successfully kicked his non-bacterial prostatitis to the curb and is now free of pelvic pain. To know more about Jim’s journey to recover and the impact of virtual healthcare, continue reading to discover his inspiring successes with this innovative approach.
One of Jim’s main frustrations when receiving his prostatitis diagnosis was the lack of clear indicators of an enlarged prostate, an elevated PSA, or any signs of infection, which made him hesitant to follow the repeated courses of recommended antibiotics. Men are often given unnecessary antibiotics without positive tests for bacterial infection. You can learn more about why this is the case, and educate yourself on urologic testing, by checking out this related blog article with information from a trusted urologist colleague.
After a familiar four-week course of Cipro antibiotics failed to fully alleviate his symptoms, Jim sought help from the Pelvic Health and Rehabilitation Center. He discovered my therapeutic yoga videos on the PHRC Youtube channel in March of 2022 and began practicing “A Stretch Routine For Your Pelvic Floor:”
Although initially skeptical of yoga, Jim decided to give it a try in the hope of finding relief from his symptoms. With consistent practice of the yoga routine, which included cat & cow, bird dog, low lunge, and hamstring stretches, he noticed a positive impact on his symptoms. Encouraged by the results, Jim scheduled a virtual therapeutic yoga evaluation with me through Zoom.
Although treating Jim over Zoom did mean that I was never able to get a full physical assessment of his musculoskeletal system, I could observe his movements on screen, gaining insights into his body mechanics and posture and how they influenced his symptoms. Through detailed questioning, I learned about repetitive activities in Jim’s daily life, such as commuting or moving student desks, which were triggering his symptoms.
Our ongoing virtual discussions allowed me to identify the likely culprits behind Jim’s pain: primary pelvic muscular dysfunction with secondary pudendal nerve irritation. It became apparent that Jim was overusing his rectus abdominis muscle (the ‘six-pack’) when flexing his trunk forward to move desks, likely aggravating and exacerbating tight, trigger points in the muscle. This repetitive motion caused the ‘binder clip’ sensation at the pubic bone, extending into his penis.
Jim’s standing posture, with his weight predominantly on the front of his feet and pelvis protruding forward in front of his ribcage, further strained his rectus abdominis and his pelvic floor muscles, too. Additionally, he admitted to unknowingly clenching his pelvic floor muscles during times of stress, which can lead to reduced blood flow and compression of the pudendal nerve, likely driving the stinging, needle-like pain he described at the tip of the penis.
The sensation of sitting on a golf ball after commuting was traced back to the overactivity of the obturator internus muscle, caused by prolonged abduction of the hips while driving and chronic muscle shortening.
Together Jim and I set goals, including enhancing core stability, improving hip and pelvic mobility, maintaining proper posture throughout the day, and modifying activities like driving and moving student desks.
Determined to address the root cause of his problems, Jim diligently worked with me remotely twice a month. He devoted himself to daily yoga, breathing exercises, and postural awareness, along with daily walks and weight loss. He was beginning to understand the value of pelvic floor physical and occupational therapy advice to help heal his condition.
As he focused on core stability, Jim mastered the bird dog pose from my Youtube yoga stretch routine and learned how to engage his transverse abdominis (TA), often referred to as the ‘corset.’ The TA facilitates spinal stability and encourages proper alignment of the ribcage over the hips. By utilizing his TA during static standing, Jim improved his posture and avoided straining the rectus abdominis, resulting in a reduction of pain.
A significant breakthrough occurred when Jim realized the connection between his symptoms and his commute. To address the ‘golf ball’ sensation that would arise after driving to work, we utilized stretches to improve internal rotation of the hip and reduce tension in the obturator internus muscle. I recommended he purchase a wedge cushion for his car seat to promote better pelvic alignment during rides, and this simple change made an immediate difference. He truly realized the power of good pelvic posture while driving when he briefly used a loaner car, without a wedge cushion, and his symptoms returned within two days.
When we sit with an anterior pelvic tilt, using either a wedge cushion or a lumbar roll for support, it helps maintain better pelvic muscle positioning compared to slouching and tucking the tailbone under. This adjustment also reduces hip abduction, enhancing optimal alignment for the obturator internus muscle.
To enhance pelvic mobility I recommended that Jim incorporate daily anterior pelvic tilting through the cat and cow stretch. This movement not only improves lumbopelvic motion but also strengthens and elongates the rectus abdominis muscle. Additionally, I suggested he practice spinal extension while standing at the wall to stretch the front of his abdomen. These exercises proved effective in alleviating the pain he experienced near his urethra by targeting and conditioning the rectus abdominis muscles and improving the mobility of his pelvis.
Furthermore, I provided instructions on how Jim should move the student desks in his classroom differently. Instead of rounding his spine forward and using parallel feet to pull the desks, I showed him how to stagger his stance in a lunge position and maintain a straight spine. This adjustment allowed him to utilize the strength of his legs to move the desks, thus reducing strain on his rectus abdominis.
Over the course of nine months, through dedicated adherence to my recommendations and unwavering commitment to a consistent routine, Jim experienced a dramatic reduction in his symptoms. Although his progress wasn’t entirely linear and included some setbacks, which are common in pelvic health rehabilitation, Jim’s resolute determination to overcome these challenges was evident.
Jim’s journey underscores the vital importance of cultivating an understanding of one’s body and paying attention to its dynamics throughout daily activities. Small micro-adjustments in daily sitting and standing can have a profound impact on pelvic health. In the long term, building a habit of mindfulness can empower individuals to seamlessly integrate these adjustments into their daily lives with minimal effort.
Furthermore, establishing a personalized regimen of stretches and strengthening exercises designed to complement one’s body tendencies proves indispensable especially with the passage of time. It was an honor to curate a therapeutic yoga routine tailored to Jim’s unique needs, one that he embraced wholeheartedly and sometimes even practiced twice daily.
Presently, Jim has been free from pain for nearly six months. His achievements extend beyond mere relief, with a remarkable 25-pound weight loss and a consistent incorporation of daily walks and yoga sessions. Perhaps most notably, Jim’s transformation includes a newfound identity as a dedicated “yoga kind-of-guy.”
Jim’s triumph serves as a powerful testament to the transformative potential of a holistic approach to pelvic health, one that can be effectively facilitated through telehealth. His story underscores the prospect of positive change through a combination of yoga therapeutics, heightened postural awareness and thoughtful lifestyle adjustments. As we reflect upon Jim’s success, it becomes evident that the journey towards lasting well-being is attainable through commitment, tailored guidance, and a comprehensive perspective on health and self-care.
__________________
A few closing words from Jim:
“Melissa Patrick has been a wonderful blessing in my life, she always encouraged me and changed my perspective on the healing benefits of yoga. She listened patiently to my struggles and modified my routines to consider what my body was telling me. She is extremely knowledgeable about all parts of the pelvic anatomy. I credit her with taking one of the biggest crosses of my life and changing it into a positive. Doing yoga is now part of my life moving forward. My positive outlook on life has returned and I can’t express in words how much Melissa Patrick has helped me. My car seat was the hidden piece in my journey to pelvic floor health!”
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.