Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
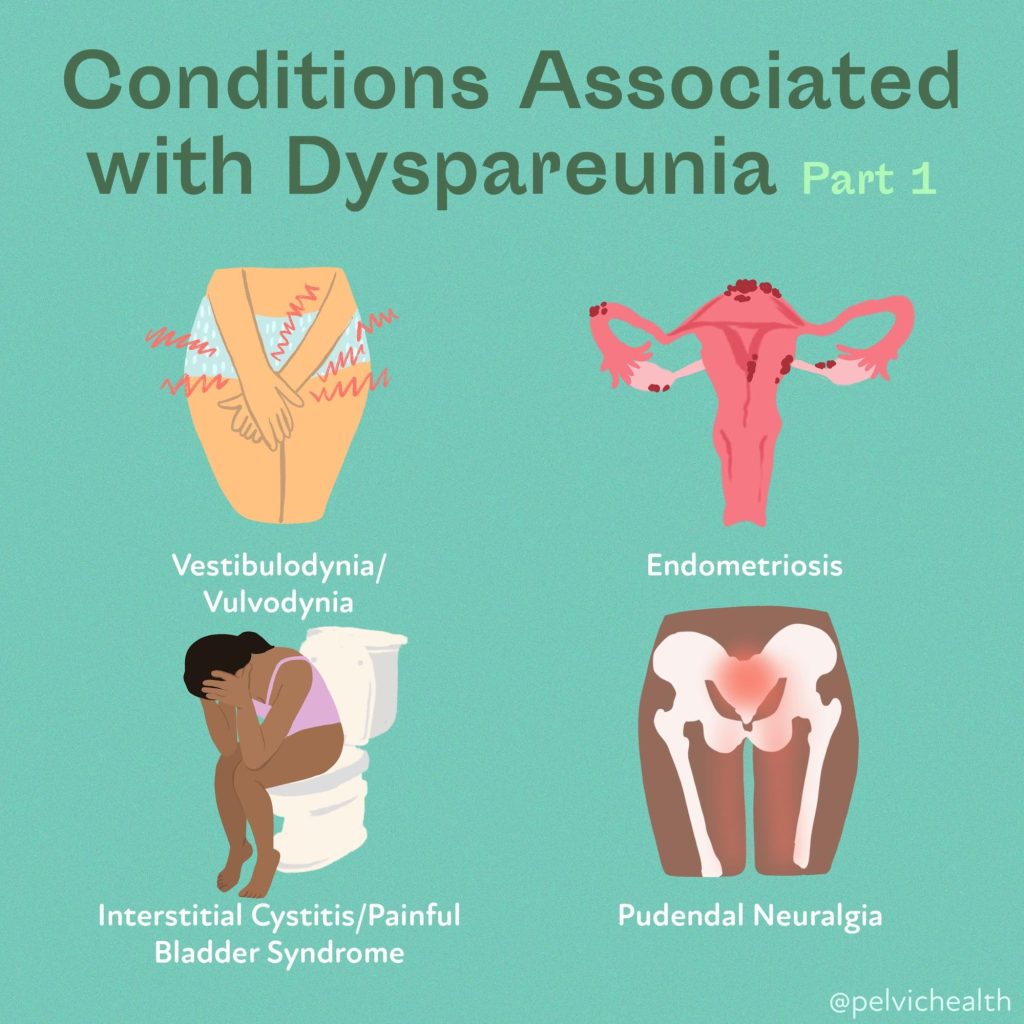
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


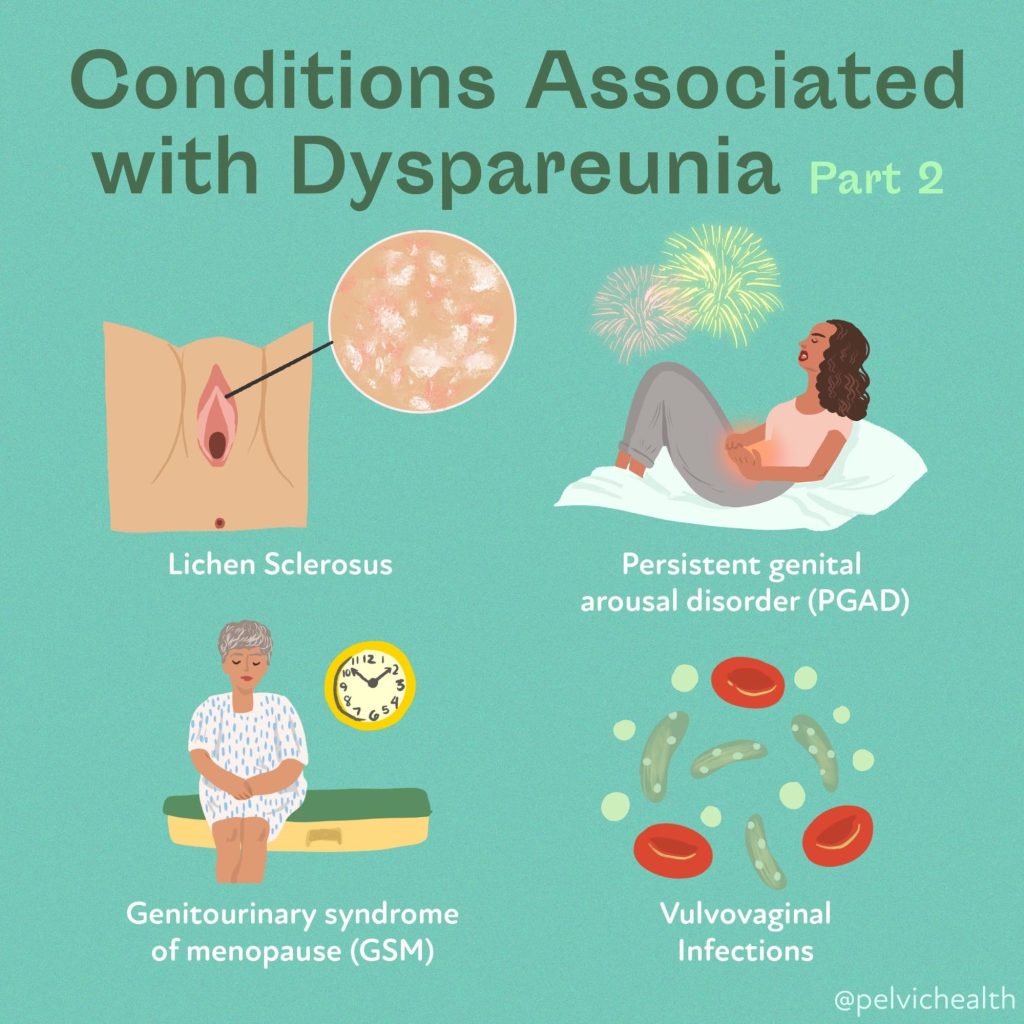
Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Stephanie Prendergast, MPT, PHRC Pasadena
Pain science education (PSE)—sometimes called pain neuroscience education—aims to help people understand what pain is, how it’s produced by the nervous system, and why it can persist even after tissues have healed. In chronic pelvic pain, where biological, psychological, and social factors often intertwine, that reconceptualization can be powerful: it can lower fear, boost self-efficacy, and open the door to graded movement, pelvic floor relaxation, and other active strategies. But how strong is the evidence specifically for pelvic pain?
What PSE is (and isn’t)
PSE is not a pep talk and it’s not a substitute for medical work-up. It’s structured learning about pain biology that targets threat appraisal, catastrophic thinking, and protective behaviors (like over-guarding the pelvic floor). A recent international e-Delphi study distilled 92 clinician-endorsed learning points for pelvic pain into 13 core concepts—e.g., “pelvic pain involves changes in the nervous system,” “pain ≠ damage,” “many factors (sleep, stress, hormones, pelvic floor tone) can amplify pain,” and “pelvic pain can change and improve.” It also highlights pelvic-specific themes such as cross-organ sensitization and why flares don’t necessarily mean disease is worsening. These clinician-derived concepts provide a concrete curriculum to guide care and future trials. Frontiers
Do guidelines recommend education for pelvic pain?
Yes. A systematic review of 17 international clinical practice guidelines for benign gynecologic and urologic conditions associated with persistent pelvic pain found that two-thirds explicitly recommend patient education, though they vary on what to teach and how to deliver it (e.g., written materials, support groups). The authors also noted guideline quality was mixed and called for better, tailored education interventions. PubMed
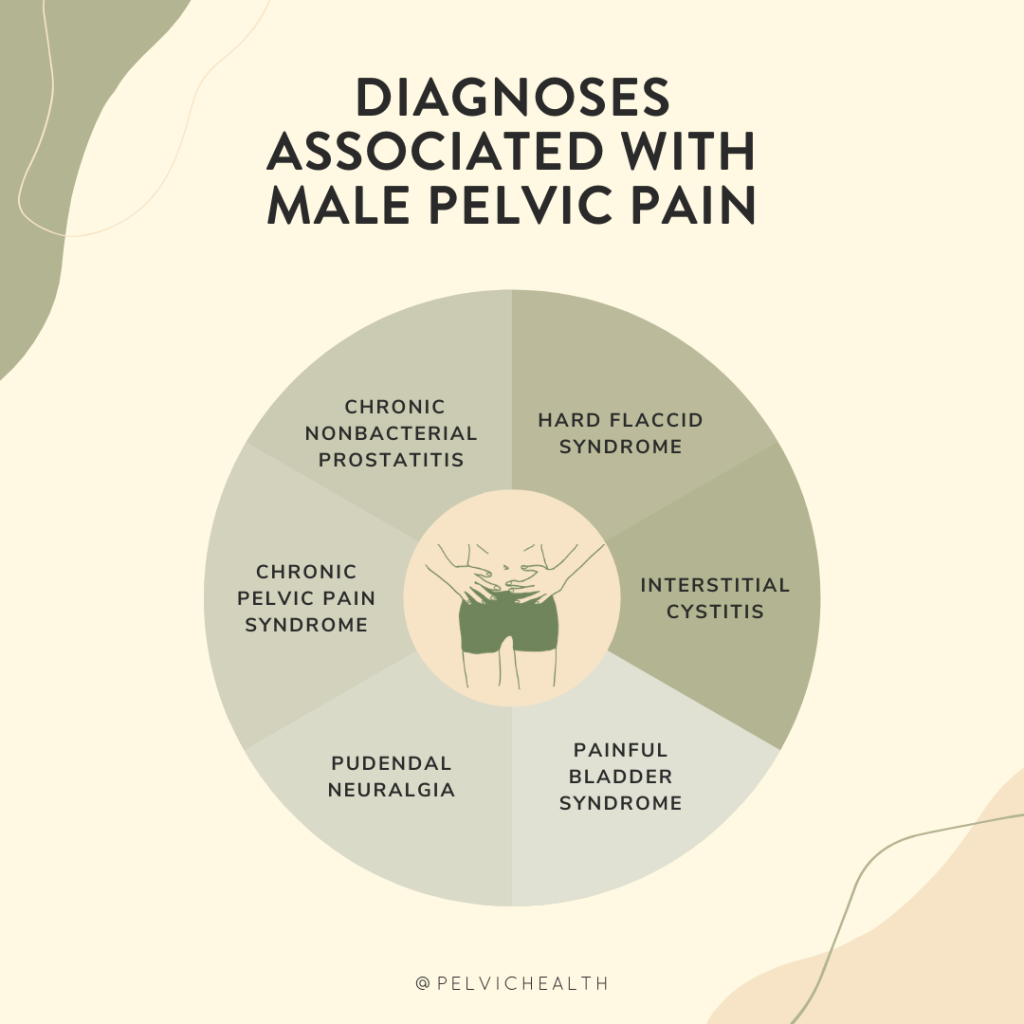
For men with chronic pelvic pain/chronic prostatitis, the 2025 American Urological Association guideline similarly emphasizes a biopsychosocial approach that includes patient education and psychological therapies such as CBT, alongside pelvic floor therapy and other modalities. American Urological Association
What’s the direct evidence for PSE in pelvic pain?
Although the pelvic-specific PSE literature is still maturing, early data are encouraging:
- Knowledge changes after a single seminar. In a pre–post study of women with chronic pelvic pain, a 90-minute neuroscience-based seminar significantly improved scores on the Neurophysiology of Pain Questionnaire and deepened conceptual understanding. Knowledge isn’t a clinical endpoint, but it’s a key mechanism target for PSE. Sydney Pelvic Clinic
- Randomized trial in genito-pelvic pain/penetration disorder (GPPPD). A three-arm RCT tested four weekly educational workshops (covering pelvic anatomy, pain neuroscience, and sexuality) delivered face-to-face or online versus waitlist. Both active formats improved pain intensity, pain-related outcomes (e.g., catastrophizing), and sexual function—benefits that did not depend on socioeconomic status. While the package included anatomy and sexuality content alongside PSE, it’s a rare randomized signal that an education-centric program can improve clinically meaningful outcomes in pelvic pain. SpringerLink
- Biopsychosocial programs where PSE is a core component. A 2025 systematic review of 14 RCTs in women with chronic pelvic pain found CBT and ACT-based approaches, mindfulness, and physiotherapy-based programs reduced pain and improved emotional outcomes. Across intervention types, two elements kept showing up as important: pain science education and structured exposure/engagement with valued activity. This points to PSE as a common “active ingredient” in effective multimodal care. PMC
Taken together, these findings suggest PSE helps patients reconceptualize their pain and, when paired with active strategies, can contribute to reductions in pain and distress in pelvic pain populations. The evidence base is still smaller than in back or neck pain, but it’s growing.
What about the much larger (non-pelvic) PSE literature?
Zooming out helps calibrate expectations. An umbrella review across chronic musculoskeletal pain concluded that PSE added to active treatments (most often exercise) tends to yield greater improvements—especially for psychosocial targets like catastrophizing and kinesiophobia—than the same treatments without PSE. By contrast, PSE alone shows inconsistent effects on pain and disability. The message is clear: use PSE as a catalyst within a broader active plan, not as a standalone. Frontiers
What patients say they need from PSE
A 2024 qualitative study asked women with “improved” pelvic pain what PSE ideas mattered most. Four themes stood out: (1) a sensitized nervous system can become overprotective (validation), (2) pain doesn’t always mean damage (reassurance and reduced fear), (3) thoughts, feelings, and attention can amplify pain (self-management levers), and (4) pain can change, slowly (hope plus a realistic time course). These patient-voiced concepts align well with the clinician-derived curriculum above and reinforce the need for tailored, stigma-reducing language. PubMed
Practical takeaways for clinicians and patients
- Tailor the content. Start with core concepts (pain ≠ damage; sensitization; many contributors) and add pelvic-specific pieces: pelvic floor guarding and down-training, cross-organ sensitization (e.g., bladder–bowel–pelvic floor “crosstalk”), hormonal influences (adolescence, perimenopause), and how flares can be managed without panic. The new pelvic pain PSE curriculum is a helpful scaffold. Frontiers
- Pair PSE with active strategies. Use education to lower threat and increase confidence, then lock in gains with graded movement, pelvic floor relaxation training, sexual pain pacing strategies, sleep/stress skills, and goal-oriented exposure to valued activities. This mirrors what effective RCT programs actually do. PMC
- Mind the psychosocials. Catastrophizing, fear-avoidance, and low self-efficacy are common in pelvic pain and are responsive targets for PSE and CBT-style skills. Major guidelines recommend integrating behavioral therapies and patient education into care plans. PubMedAmerican Urological Association
- Delivery can be flexible. Group workshops (with partner inclusion), one-to-one sessions, printed/online materials, and telehealth can all work. The GPPPD RCT suggests online and face-to-face education can be similarly effective when content and structure are sound. SpringerLink
Where the evidence is still thin
We still need larger, high-quality pelvic-specific RCTs that isolate the contribution of PSE, report core outcomes, and test dose, timing, and delivery (individual vs group; in-person vs digital). Encouragingly, researchers have now defined what to teach; the next step is rigorous trials testing how best to teach it and for whom. Meanwhile, multimodal programs that include PSE remain the most evidence-aligned option. FrontiersPMC
References
American Urological Association. (2025). Male chronic pelvic pain guideline. https://www.auanet.org/guidelines-and-quality/guidelines/male-chronic-pelvic-pain-guideline American Urological Association
James, A., Thompson, J., Neumann, P., & Briffa, K. (2019). Change in pain knowledge after a neuroscience education seminar for women with chronic pelvic pain. Australian and New Zealand Continence Journal, 25(2), 39–44. (PDF). Sydney Pelvic Clinic
Johnson, S., Bradshaw, A., Bresnahan, R., Evans, E., Herron, K., & Hapangama, D. K. (2025). Biopsychosocial approaches for the management of female chronic pelvic pain: A systematic review. BJOG, 132(3), 266–277. https://doi.org/10.1111/1471-0528.17987 (Open Access). PMC
Mardon, A. K., Leake, H. B., Szeto, K., Moseley, G. L., & Chalmers, K. J. (2024). Recommendations for patient education in the management of persistent pelvic pain: A systematic review of clinical practice guidelines. Pain, 165(6), 1207–1216. https://doi.org/10.1097/j.pain.0000000000003137 PubMed
Mardon, A. K., Leake, H. B., Wilson, M. V., Karran, E. L., Parker, R., Malani, R., Moseley, G. L., & Chalmers, K. J. (2025). Pain science education concepts for pelvic pain: An e-Delphi of expert clinicians. Frontiers in Pain Research, 6, 1498996. https://doi.org/10.3389/fpain.2025.1498996 (Open Access). Frontiers
Mardon, A. K., Chalmers, K. J., Heathcote, L. C., et al. (2024). “I wish I knew then what I know now”—Pain science education concepts important for female persistent pelvic pain: A reflexive thematic analysis. Pain, 165(9), 1990–2001. https://doi.org/10.1097/j.pain.0000000000003205 PubMed
Cuenca-Martínez, F., et al. (2023). Pain neuroscience education in patients with chronic musculoskeletal pain: An umbrella review. Frontiers in Neuroscience, 17, 1272068. https://doi.org/10.3389/fnins.2023.1272068 (Open Access). Frontiers
Lopez-Brull, A., Pérez-Domínguez, B., Cantón-Vitoria, L., Plaza-Carrasco, M., & Nahon, I. (2023). Association levels between results from a therapeutic educational program on women suffering from genito-pelvic pain/penetration disorder and their socioeconomic status. Sexuality Research and Social Policy, 20, 1180–1187. https://doi.org/10.1007/s13178-023-00790-7 (Open Access; includes RCT methods and outcomes). SpringerLink
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Stephanie Prendergast, MPT, PHRC Pasadena
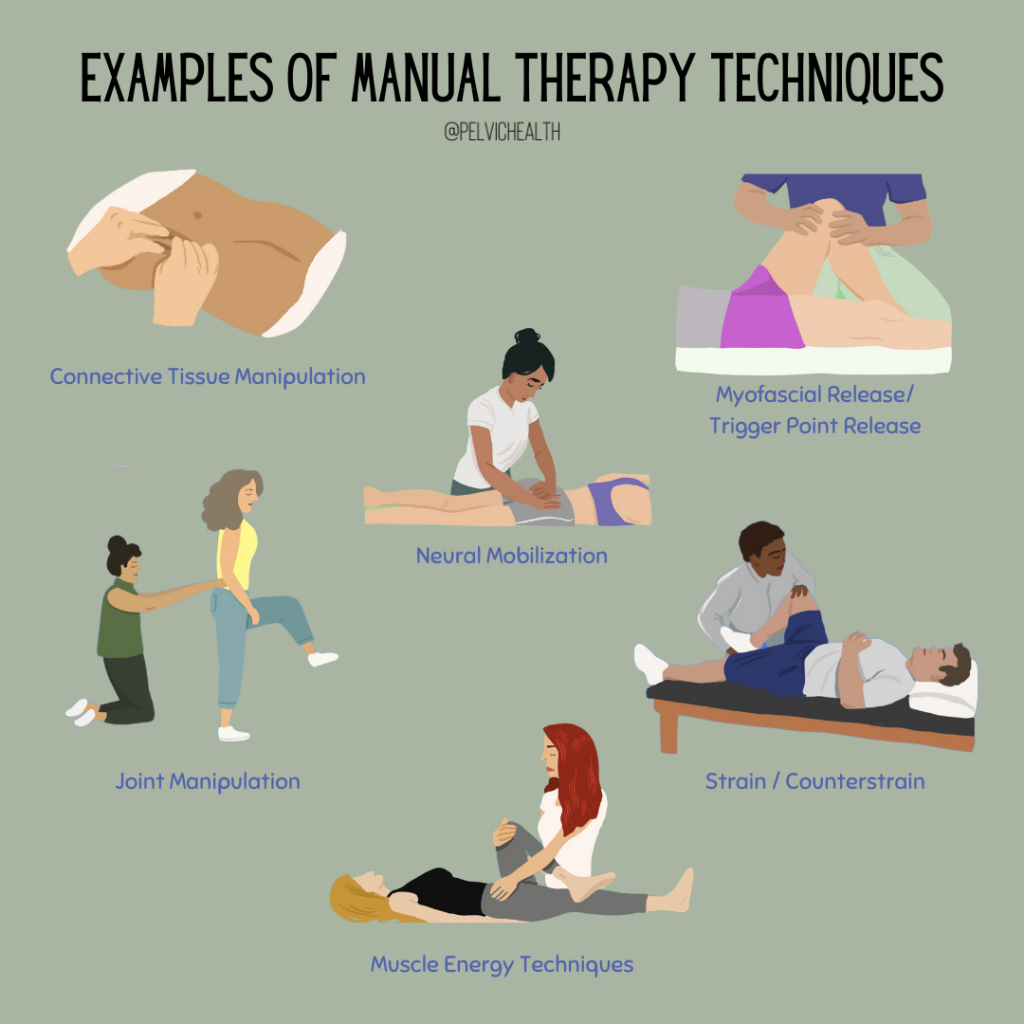
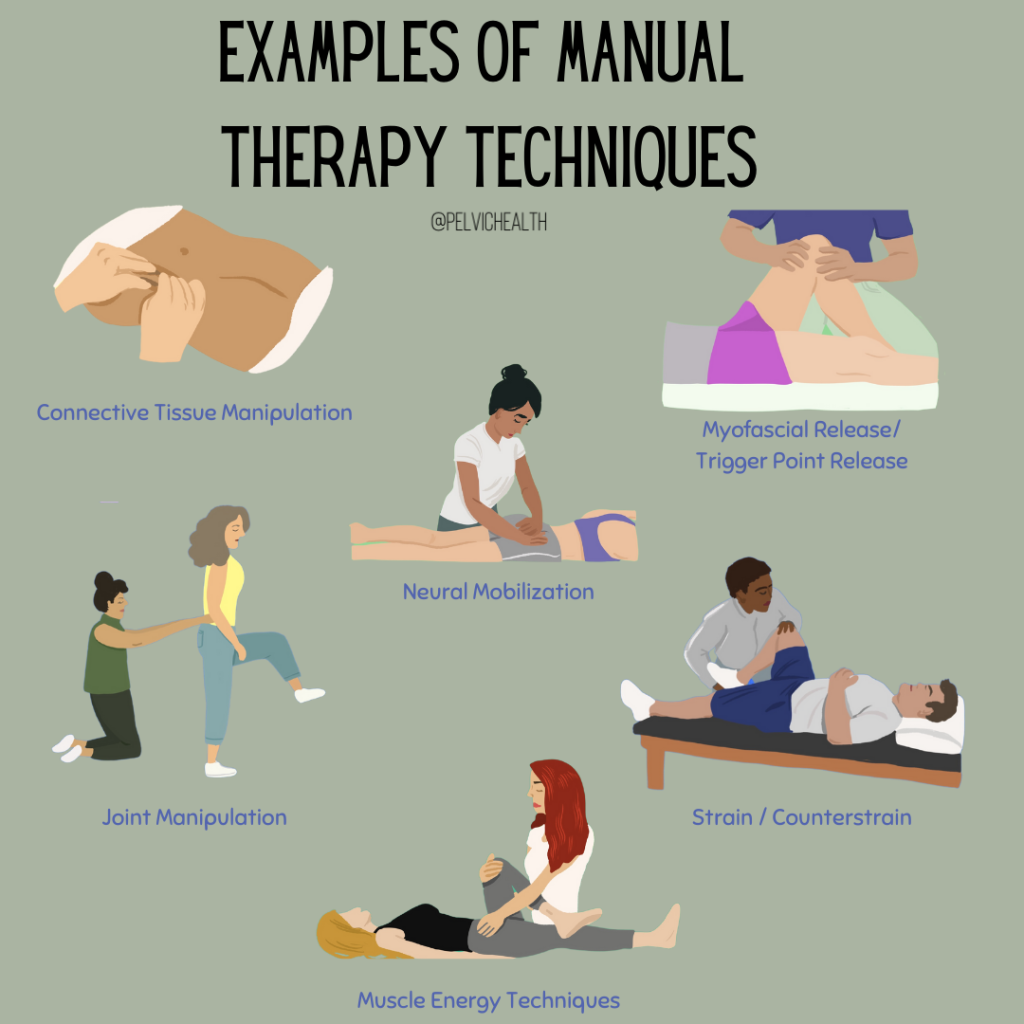
In our last blog post we summarized general benefits of manual therapy for myofascial pain. In this post, we are going to take a deeper dive and explore the benefits of manual therapy for myofascial pelvic pain syndromes. This will be a three part series, our next post examines the evidence behind Pain Science Education (PSE) for people recovering from pelvic pain syndromes.
I’m honored to be speaking at PelviCon 2025, an outstanding event created by Nicole Cozean and Jessica Reale for clinicians passionate about pelvic health. Each speaker will be delivering two lectures, and one of mine is titled:
“Pain Science Education vs. Manual Therapy: A Practitioner’s Dilemma”
To hear more about the dilemma, please check out my Pelvic PT Rising podcast interview with PelviCon Cofounder Nicole Cozean! But for now, let’s look at more evidence.
Unlocking Relief: Manual Therapy’s Role in Treating Pelvic Pain
Pelvic pain is a pervasive issue affecting many individuals—women and men alike—across their lifespan. From dyspareunia and endometriosis to myofascial pelvic pain and chronic pelvic floor dysfunction, manual therapy is gaining recognition as a valuable component in multimodal treatment plans. Let’s explore what recent studies say about its effectiveness and where evidence remains inconclusive.
What Is Manual Therapy?
Manual therapy encompasses hands-on techniques—such as manipulation, mobilization, soft‑tissue techniques, and muscle‑energy methods—administered by trained professionals (e.g., physical and occupational therapistss, osteopaths, massage therapists) to treat musculoskeletal conditions by enhancing mobility, reducing pain, and restoring function BioMed Central+7MDPI+7PMC+7Wikipedia+1.
Evidence Highlights and Recent Findings
1. Dyspareunia (Painful Intercourse)
A systematic review spanning 1997–2018 found limited but positive results: although only three observational studies and one randomized trial were included, all reported significant reductions in pain levels on the Female Sexual Function Index, supporting manual therapy’s potential benefits. However, study quality varied and sample sizes were small PMC+1.
2. Pelvic Pain in Endometriosis
A more controlled, recent RCT (2023) tested a six-week protocol combining soft tissue and articulatory techniques for women with chronic pelvic pain due to endometriosis. It produced a 30.8 % pain reduction immediately after treatment and 27.3 % at one-month follow‑up, suggesting promising effects.ScienceDirect+3MDPI+3ScienceDirect+3.
3. Myofascial Pelvic Pain (MFPP)
A narrative review and case series (2023) summarized ten manual techniques — including myofascial trigger point release, Thiele massage, perineal massage, connective tissue manipulation, visceral therapy, scar release, and coccyx manipulation. The evidence supports pelvic floor manual therapy as a promising, effective, and safe recommendation for MFPP, though more rigorous trials are needed ResearchGate.
4. Chronic Pelvic Pain More Broadly
A 2025 systematic review and meta-analysis found that multimodal physical and occupational therapy, which often includes manual interventions, demonstrated high-certainty effectiveness in women with chronic pelvic pain. ScienceDirect.
6. Case Highlight: Male Pelvic Floor Dysfunction
While not a formal study, a 2025 Business Insider story illustrates real-world impact: a man suffered for six years from pelvic symptoms before being correctly diagnosed with a tight pelvic floor. Bi‑weekly manual therapy and tailored exercises resolved his symptoms within six months—highlighting manual therapy’s relevance for men as well Business Insider.
Techniques in Focus
Manual therapy for pelvic pain may include:
- Soft tissue and articulatory techniques: Target the pelvic floor, fascia, and joints directly.
- Trigger point release & Thiele massage: Focused pressure to reduce hyperirritability in muscles.
- Muscle energy techniques (METs): Involve patient‑initiated movement against resistance to normalize muscle function.
- Other supportive modalities: Scar release, connective tissue manipulation, visceral work, even coccyx mobilization—all aiming to restore mobility and reduce nociceptive input.
Why Manual Therapy May Help
Manual therapy may help pelvic pain through several mechanisms:
- Muscle relaxation and trigger point deactivation, reducing localized pain and tension.
- Improved mobility of restricted joints or fascial planes.
- Modulation of pain signaling, potentially through neurologic or biopsychosocial pathways.
- Multimodal synergy: When combined with exercise, education, and psychosocial interventions, manual therapy enhances the overall effectiveness of treatment obgyn.onlinelibrary.wiley.com+12ScienceDirect+12PMC+12PMC+3Scholars@Duke+3BioMed Central+3.
Take-Home Points for Clinicians and Readers
- Manual therapy offers real promise for various types of pelvic pain—especially when integrated into tailored, patient-centered treatment plans.
- Current evidence is supportive but preliminary. More high-quality RCTs are vital to confirm efficacy, optimize protocols, and identify which techniques work best for specific conditions.
- Clinician training matters. Therapy success depends significantly on provider skill, technique selection, and patient responsiveness.
- Approach pelvic pain holistically. Addressing physical, psychological, and social contributors can magnify benefits and improve outcomes MDPIPubMedjmig.orgResearchGateself.com+6Business Insider+6health.com+6.
References (APA Style)
- Bishop, M. D. (2020). Maximizing Effects of Manual Therapies for Pelvic Pain. Journal of Pelvic Health.
- Deodato, M. (2023). Efficacy of manual therapy and pelvic floor exercises for [abstract]. Journal of Women’s Health.
- González-Mena, Á. (2024). Treatment of Women With Primary Dysmenorrhea With Manual Therapy. Physical and Occupational Therapy Journal, 104(5), pzae019.
- Hall, H. (2016). The effectiveness of complementary manual therapies… Journal of Pregnancy Pain Management.
- Johnson, S. (2025). Biopsychosocial Approaches for the Management of Female CPP. BJOG: An International Journal of Obstetrics & Gynaecology.
- Muñoz-Gómez, E., et al. (2023). Effectiveness of a Manual Therapy Protocol in Women with Pelvic Pain Due to Endometriosis: A Randomized Clinical Trial. Journal of Clinical Medicine, 12(9), 3310.
- Sarrel, S. (2017). Physical and Occupational Therapy and Endometriosis: Using Manual Techniques. Journal of Minimally Invasive Gynecology.
- Trahan, J. (2019). The Efficacy of Manual Therapy for Treatment of Dyspareunia: Systematic Review. Journal of Women’s Sexual Health.
- Youssef, A. A., et al. (2023). Manual therapy for myofascial pelvic pain: A case report and narrative review. Pelvic Pain Journal.
- Anonymous. (2025, July). A man had to organize his day around restroom trips… Business Insider.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Stephanie Prendergast, MPT, PHRC Pasadena
I’m honored to be speaking at PelviCon 2025, an outstanding event created by Nicole Cozean and Jessica Reale for clinicians passionate about pelvic health. Each speaker will be delivering two lectures, and one of mine is titled:
“Pain Science Education vs. Manual Therapy: A Practitioner’s Dilemma.”
Why is this a dilemma?
Research consistently shows that the majority of patients with pelvic pain syndromes have neuromuscular contributions to their symptoms, involving soft tissue structures—such as muscle and connective tissue—as well as peripheral and central nervous system dysfunction. Multiple clinical guidelines, including the AUA Guidelines for Interstitial Cystitis/Bladder Pain Syndrome, Expert Consensus on Pelvic Floor Hypertonicity, Management Strategies for CP/CPPS, and the Vulvodynia Guidelines, all emphasize manual therapy as a key component of treatment.
Despite the expert evidence-based guidelines clinical professionals argue about the role of manual therapy in treating pain. It was surprising to me when tools (our hands!) that we effectively use started to be criticized. This debate began roughly 15 years ago as Pain Science Education theories emerged. I was excited to learn about Pain Science Education, in my mind it was an addition to my clinical practice, not a substitution for manual therapy. We will dive deeper into these concepts over several blog posts.
This post kicks off a series first exploring the evidence behind manual therapy’s local tissue effects and its influence on peripheral and central sensitization. I’m looking forward to sharing these insights—and sparking some important conversations—at PelviCon this September! Although the in-person event is sold out, virtual tickets are still available.
Next, we will dive into Pain Science theories.
Introduction
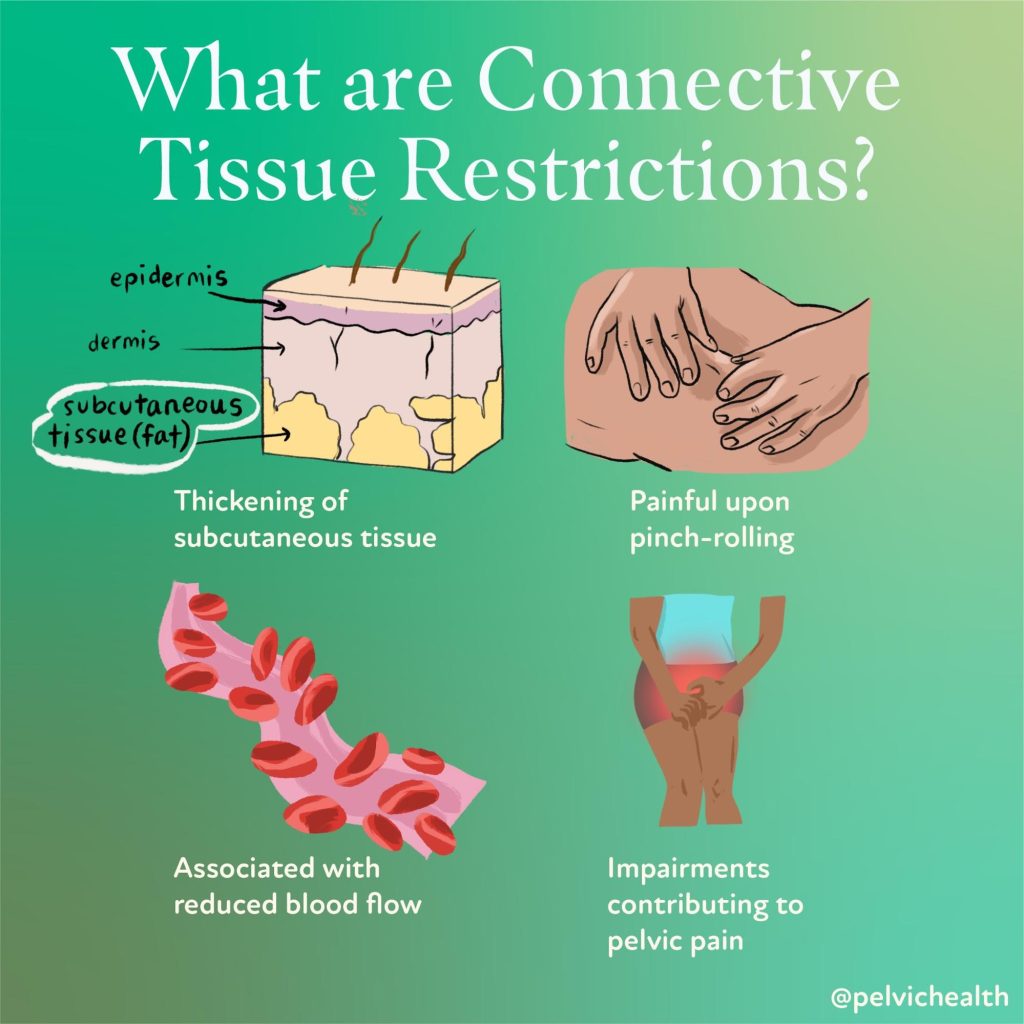
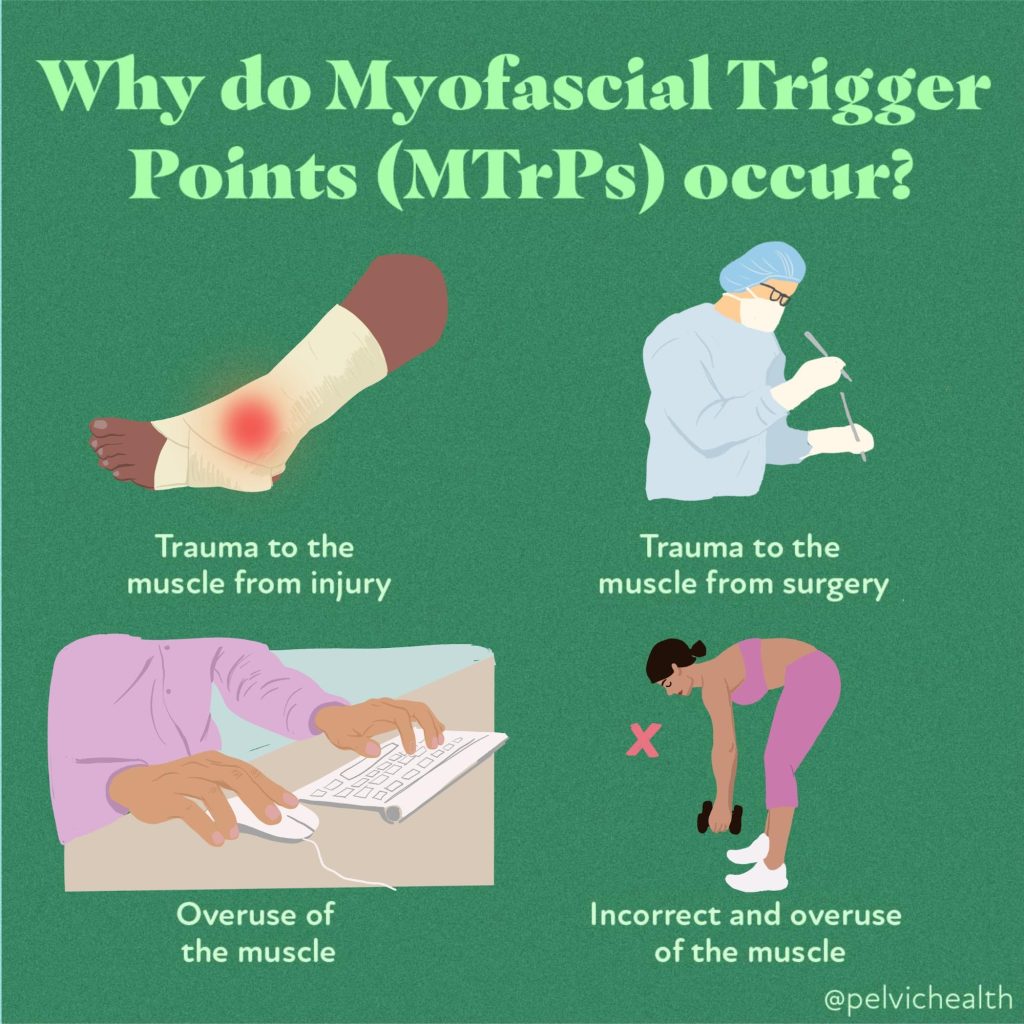
Myofascial pain is a widespread clinical complaint characterized by the presence of taut bands, trigger points, and localized tenderness within skeletal muscles or connective tissue. While the nervous system plays a central role in how pain is processed and perpetuated, the local tissue environment—including muscles, fascia, and connective tissue—also significantly contributes to both the cause and relief of myofascial pain. One widely used intervention for this condition is soft tissue manual therapy, a hands-on approach that targets the dysfunctional tissues themselves.
In this blog post, we explore the local (peripheral) tissue effects of soft tissue manual therapy, helping to demystify how techniques like myofascial release, trigger point therapy, and deep tissue massage work on a biological level to relieve pain and improve function.
Understanding Myofascial Pain
Myofascial pain arises when muscle fibers or fascia become stiff, shortened, or contain hyperirritable nodules known as trigger points. These points often refer pain to other areas and can lead to restricted movement, altered motor control, and autonomic changes like sweating or vasoconstriction.
While central sensitization and nervous system involvement are key components in chronic pain, many patients present with clear peripheral tissue dysfunction. This is where soft tissue manual therapy is believed to be particularly effective.
What Is Soft Tissue Manual Therapy?
Soft tissue manual therapy encompasses a wide range of techniques aimed at:
- Lengthening shortened tissue
- Reducing myofascial adhesions
- Increasing local circulation
- Modulating tissue tone
- Improving lymphatic drainage
Techniques may include:
- Myofascial release
- Trigger point pressure release
- Cross-fiber friction
- Instrument-assisted soft tissue mobilization (IASTM)
- Deep tissue massage
- Skin rolling/connective tissue manipulation and fascial stretching
While these methods vary, they all aim to improve the physical properties and function of the local soft tissues, contributing to pain relief and improved movement.
Local Tissue Effects of Manual Therapy
1. Increased Blood Flow and Oxygenation
One of the most immediate effects of manual therapy is enhanced circulation. Restricted or taut tissues often suffer from local ischemia—reduced blood flow—which limits the delivery of oxygen and nutrients and allows the buildup of metabolic waste.
Manual pressure and tissue mobilization can dilate capillaries, improving microcirculation and allowing for better exchange of oxygen and waste products. Research using near-infrared spectroscopy and Doppler ultrasound has shown increases in blood flow after soft tissue manipulation, which may support tissue healing and reduce chemical nociception from inflammatory mediators (Bialosky et al., 2009).
2. Reduction of Inflammatory Mediators
Trigger points and myofascial adhesions often show elevated levels of inflammatory and pain-related chemicals such as substance P, CGRP, bradykinin, and cytokines. Studies using microdialysis have identified these chemical changes in active trigger points.
Manual therapy may help to disperse or modulate these biochemical irritants, possibly by improving drainage and reducing stagnation in the interstitial space. Some hypothesize that repeated mechanical loading alters gene expression in fibroblasts and local immune cells, thus influencing the tissue’s biochemical environment (Srbely, 2010).
3. Mechanical Disruption of Adhesions
A core principle of myofascial therapy is the belief that adhesions or abnormal cross-linking between fascial layers can restrict mobility and sensitize nociceptors. Techniques like cross-fiber friction or fascial stretch aim to mechanically break up or remodel these restrictions, restoring the normal gliding and elasticity between layers of fascia, muscle, and skin.
While direct imaging of fascia changes is still emerging, studies using ultrasound elastography and biomechanical measurements suggest that manual therapy can improve tissue pliability and reduce stiffness in myofascial tissues (Stecco et al., 2014).
4. Modulation of Connective Tissue Cells
Fascia and connective tissue are biologically active. Fibroblasts and fascial cells respond to mechanical pressure through a process called mechanotransduction, where physical forces are converted into biochemical signals. Research shows that applying strain or shear to fascial tissues leads to:
- Cytoskeletal remodeling
- Changes in extracellular matrix synthesis
- Altered fibroblast alignment and activity
This suggests that manual therapy may alter the architecture of connective tissue over time, improving elasticity and hydration, and possibly helping prevent the recurrence of myofascial dysfunction (Langevin et al., 2013).
5. Deactivation of Trigger Points
Direct pressure to trigger points is thought to induce ischemic compression, which paradoxically increases blood flow after release. This leads to inactivation of the trigger point, possibly through:
- Disruption of the motor endplate activity
- Restoration of sarcomere length
- Reduced spontaneous electrical activity in affected motor units
Trigger point release has been shown to improve range of motion and reduce pain sensitivity at the local and referred pain site (Fernández-de-las-Peñas et al., 2005).
Emerging Research and Imaging
Recent advances in imaging, like high-resolution ultrasound, MRI, and elastography, have started to visualize real-time changes in fascial layers and trigger points. Some studies show:
- Decreased stiffness in treated areas
- Improved shear strain between fascial planes
- Visualization of fluid movement and thickness changes in tissue layers after manual therapy
This is helping validate what many manual therapists have long observed: tissues truly do change in response to skilled touch.
Clinical Takeaway
The local tissue effects of soft tissue manual therapy offer a scientifically grounded explanation for its clinical effectiveness in treating myofascial pain. While the nervous system and psychosocial context cannot be ignored, there is robust evidence supporting direct, local mechanisms including:
- Improved circulation and oxygen delivery
- Decreased biochemical irritants
- Restoration of fascial mobility
- Modulation of connective tissue cell behavior
- Inactivation of trigger points
For patients with myofascial pain, combining manual therapy with education, movement retraining, and lifestyle modification offers a comprehensive and effective treatment plan. At PHRC, we are expertly trained in manual therapy techniques to best help our patients recover efficiently. For more information and to schedule please visit our website!
References
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. (2009). The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Manual Therapy, 14(5), 531-538.
Srbely JZ. (2010). New trends in myofascial pain syndrome: pathogenesis and clinical implications. Techniques in Regional Anesthesia and Pain Management, 14(3), 114-120.
Stecco C, Macchi V, Porzionato A, et al. (2014). The fasciacytes: a new cell devoted to fascial gliding regulation. Clinical Anatomy, 27(6), 861–869.
Fernández-de-las-Peñas C, Dommerholt J. (2005). Myofascial trigger points: peripheral or central phenomenon? Current Pain and Headache Reports, 9(6), 370–375.
Langevin HM, et al. (2013). Connective tissue fibroblast response to stretching: clinical implications. Journal of Bodywork and Movement Therapies, 17(4), 397–404.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!