
If you’ve been dealing with ongoing pelvic pain, discomfort with urination, or sexual symptoms that never seem to improve, you’re not alone. Chronic prostatitis, also known as Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS), is a condition that affects men of all ages. In fact, about 10% of men experience prostatitis-like symptoms at some point in their lives.
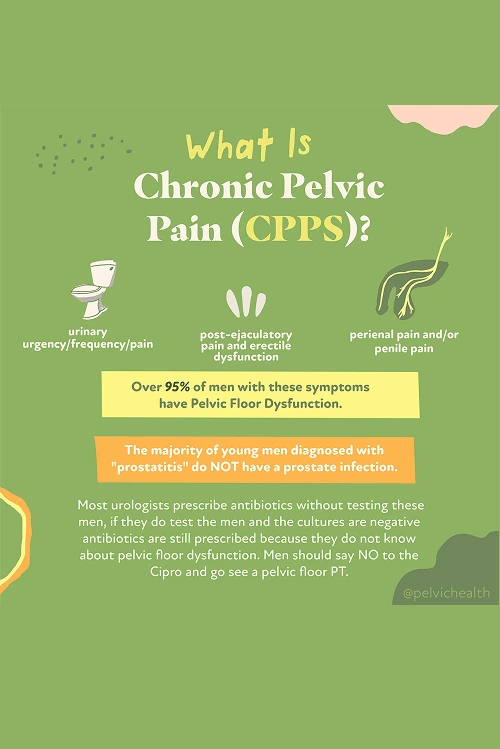
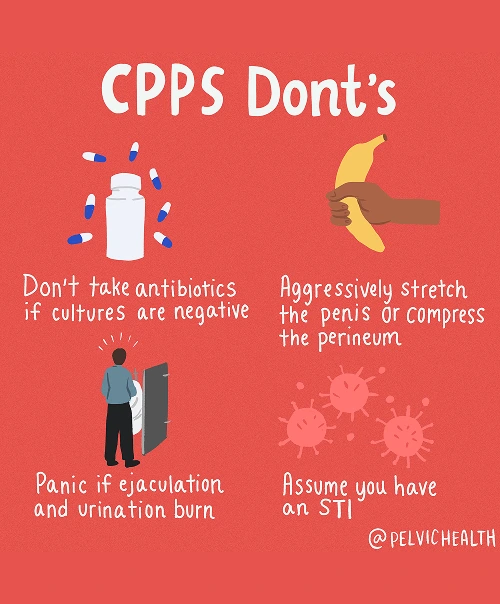
But here’s what’s surprising — 97% of these men do not actually have a prostate or bladder infection, yet they are often prescribed antibiotics anyway. For the vast majority, the problem isn’t an infection at all. Instead, the symptoms are often caused by the pelvic floor muscles. When your pelvic floor muscles become tight, irritated, or uncoordinated, they can trigger the same symptoms you might expect from a prostate issue.
That’s why many men who have been diagnosed with chronic prostatitis can benefit from pelvic floor physical and occupational therapy. At PHRC, our team of pelvic floor physical and occupational therapists can help you find relief. By addressing muscle dysfunction, restoring balance, and reducing tension in the pelvic floor, we target the actual cause of your symptoms.
What are the Causes of Chronic Pelvic Pain Syndrome in Men?
Chronic Pelvic Pain Syndrome doesn’t usually come from an infection in the prostate, even though many men are told that it does. Instead, there are actually several potential sources of pain, and most of them have to do with the way your body’s systems interact with the pelvic floor.
- Lumbar pathology: The nerves that serve your pelvic region begin in the lower back. If a disc bulges, arthritis develops, or a lumbar nerve gets irritated, the pain can radiate forward and feel like it’s in your pelvis or prostate, even when the true source is the spine.
- Vascular pathology: Circulation issues in the pelvic region, such as varicoceles (enlarged veins), vascular congestion, or changes in blood supply, can create aching or heaviness that feels similar to prostate pain.
- Pelvic floor pathology: The pelvic floor muscles sit like a hammock under the pelvis. If they tighten, spasm, or lose proper coordination, they can irritate nerves and create pain that feels like it’s coming from the prostate or bladder. In reality, the muscles themselves are the main driver.
Other contributing factors can include:
- Past surgeries such as vasectomy or prostate procedures
- Structural issues like hip dysfunction, scoliosis, or leg length differences
- Excessive or sudden changes in exercise
- Long hours of sitting
- Chronic constipation or frequent straining
- Trauma or stress to the pelvic area
While there are multiple possible contributors, the majority of men with chronic pelvic pain, including those with urinary or bowel symptoms, have pelvic floor dysfunction as the underlying problem.
Symptoms of Chronic Pelvic Pain Syndrome
The symptoms of CPPS can be very confusing and frustrating because they often feel like a prostate or bladder problem, even though the issue could actually be coming from the pelvic floor muscles. If you’re dealing with CPPS, you might notice one or more of the following:
- Aching, pressure, or sharp pain in the perineum, pubic area, or lower abdomen
- Discomfort that feels like it’s coming from the testicles, tip of the penis, or inside the urethra
- Urgency, frequency, weak stream, or the sensation that you can’t fully empty your bladder
- Burning or stinging, even when no infection is present
- Pain with or after ejaculation, erectile discomfort, or reduced sexual satisfaction
- Tightness or aching that overlaps with pelvic discomfort
- A sense of heaviness, pressure, or tight muscles in the pelvic floor area
Associated Diagnoses
Chronic pelvic pain in men can be connected to a range of many recognized conditions. Some involve the spine, some the blood vessels, and many the pelvic floor muscles themselves.
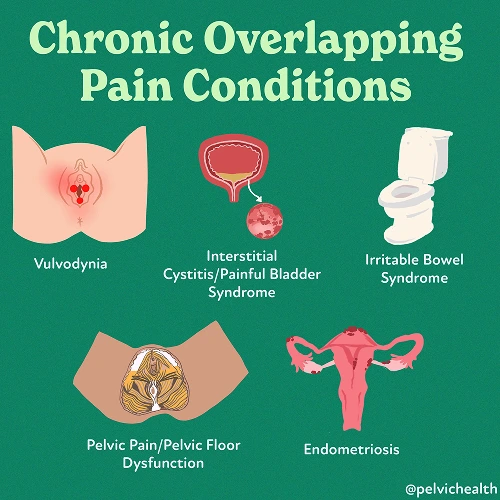
Low back problems like lumbar radiculopathy, disc injuries, or arthritis can create nerve irritation that radiates into the pelvis and mimics prostate pain. Issues such as varicocele, testicular torsion, or pelvic venous congestion can alter blood flow and lead to aching, heaviness, or sharp pain. And while Chronic Pelvic Pain Syndrome is the most common, pelvic floor dysfunction can also overlap with pudendal neuralgia, painful bladder syndrome, or conditions like hard flaccid syndrome.
In many cases, pelvic floor dysfunction acts as the underlying link, either directly creating pain or making symptoms from the spine or vascular system worse.
Diagnostic Challenges
One of the biggest frustrations for men with CPPS is getting the right diagnosis. Many are told they have prostatitis and are given antibiotics, even when no infection is present. In fact, research shows that more than 90% of men with pelvic or genitourinary pain do not have a bacterial prostate infection.
Instead, most fall into the National Institutes of Health (NIH) Category III classification of prostatitis:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Instead, most fall into the National Institutes of Health (NIH) Category III classification of prostatitis:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Because lumbar and vascular problems can often mimic pelvic floor pain, and because testing often comes back “normal,” men tend to be left without any clear answers. This overlap delays proper treatment and leaves many cycling through rounds of antibiotics, referrals, and frustration before discovering that pelvic floor physical and occupational therapy can target the true source.
Symptoms of Chronic Pelvic Pain Syndrome
Because CPPS is rarely caused by infection, treatment looks different than just taking antibiotics. The focus is on restoring balance to the pelvic floor, calming the irritated nerves, and addressing any other systems that are contributing to your pain.
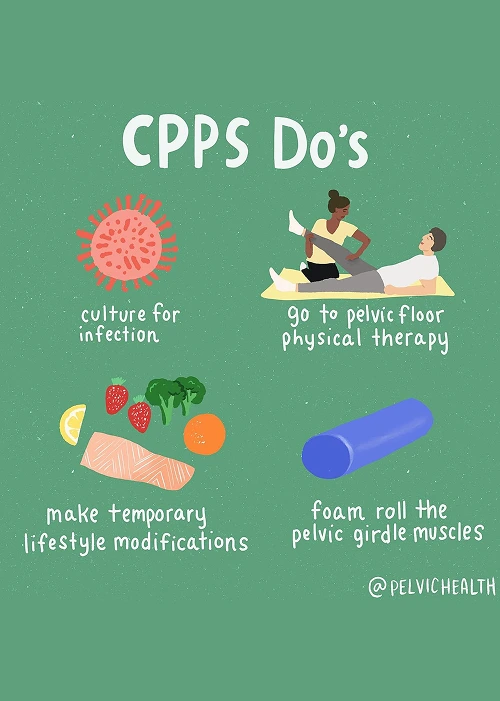
- Pelvic floor physical and occupational therapy: This is the foundation of treatment for most men with CPPS. Therapy helps release tight pelvic floor muscles, retrain coordination, and calm down irritated nerves that drive pain and urinary symptoms.
- Spine and back treatment: If nerve irritation in the lumbar spine contributes to your symptoms, pelvic floor physical and occupational therapy can address posture, mobility, and movement patterns. In some cases, a physician may recommend injections.
- Vascular-related treatment: When circulation issues play a role, pelvic floor physical and occupational therapy can reduce muscle guarding, improve blood flow through posture and breathing work, and take pressure off congested veins.
- Biomechanical support: Addressing any hip dysfunction, mobility restrictions, or movement imbalances can reduce stress on the pelvis and lower back, making your symptoms easier to manage.
- Lifestyle adjustments: Simple changes (like managing constipation, limiting prolonged sitting, and gradually returning to exercise) help reduce pelvic strain and prevent flare-ups.
How We Can Help with Your Chronic Pelvic Pain
Men living with chronic pelvic pain often spend months or even years searching for answers. By the time you reach us, you’ve likely tried antibiotics, been told different things by different providers, and still have symptoms that disrupt your life. That’s where a focused evaluation with one of our pelvic floor physical and occupational therapists specializing in pelvic pain can help.
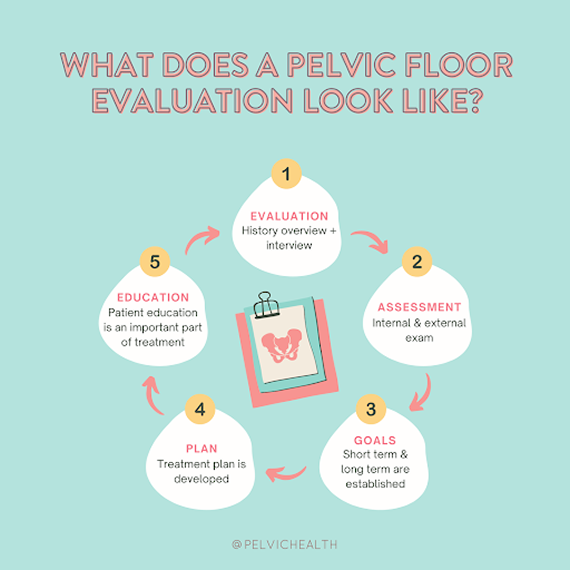
During your evaluation at PHRC, your pelvic floor physical and occupational therapist reviews your history and symptoms with you, what you have been diagnosed with in the past, the treatments you have undergone (if any), and how effective or not effective these treatments have been.
We recognize how completely exhausting this process can be, and we take the time to listen so you feel heard.
How We Can Help with Your Chronic Pelvic Pain
Men living with chronic pelvic pain often spend months or even years searching for answers. By the time you reach us, you’ve likely tried antibiotics, been told different things by different providers, and still have symptoms that disrupt your life. That’s where a focused evaluation with one of our pelvic floor physical and occupational therapists specializing in pelvic pain can help.
During your evaluation at PHRC, your pelvic floor physical and occupational therapist reviews your history and symptoms with you, what you have been diagnosed with in the past, the treatments you have undergone (if any), and how effective or not effective these treatments have been.
We recognize how completely exhausting this process can be, and we take the time to listen so you feel heard.
During your physical examination, your PHRC pelvic floor physical and occupational therapist examines muscles, tissues, joints, nerves, and your movement patterns. Once they complete the evaluation, they will review your findings with you and create an assessment that explains how you developed the pain and establish short- and long-term goals for your treatment plan.
Typically, the frequency of our pelvic floor physical and occupational therapy treatment is one to two times per week for roughly 12 weeks. You are given a home exercise program to complement your in-person sessions, and your PHRC pelvic floor physical and occupational therapist will help to coordinate your recovery with the other members of your treatment team. We are here to help you recover and finally get relief from your symptoms.
