
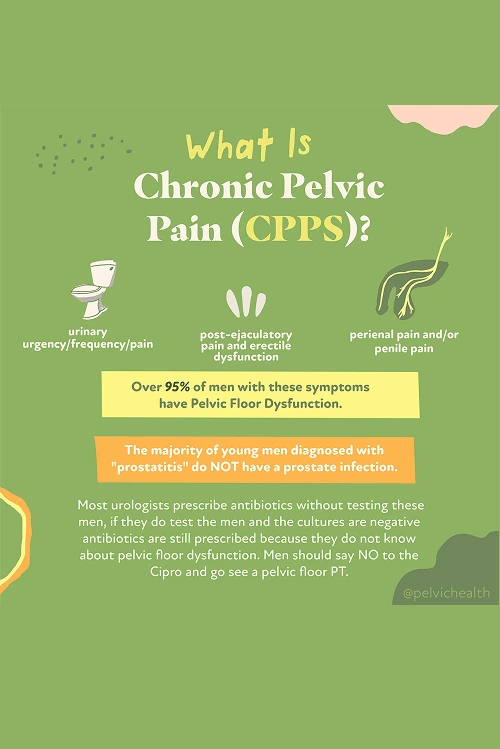
If you’re a man in Echo Park and have been living with pelvic discomfort, pain during urination, or sexual issues that don’t seem to go away, you’re not the only one. Many men deal with these same concerns, often caused by a condition called chronic prostatitis, also known as Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS). It’s estimated that roughly 10% of men will experience these symptoms at some point in their lifetime.
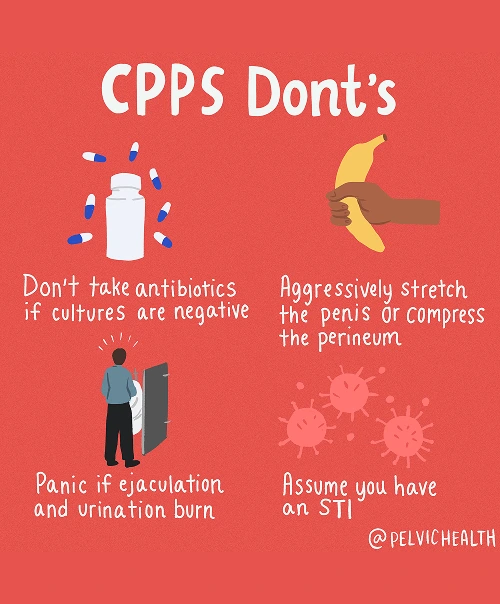
Interestingly, research has shown that about 97% of these men do not have a true prostate or bladder infection, even though antibiotics are commonly prescribed. The actual source of the pain in most cases lies within the pelvic floor muscles. When these muscles are tight, inflamed, or uncoordinated, they can create the same sensations associated with a prostate condition.
For Echo Park residents experiencing these frustrating symptoms, pelvic floor physical and occupational therapy at PHRC offers real hope. Our dedicated team of pelvic floor physical and occupational therapists focuses on relieving muscle dysfunction, restoring mobility, and easing tension in the pelvic area. By addressing the muscular causes rather than just the surface symptoms, we help you achieve lasting comfort and improved daily function.
What are the Causes of Chronic Pelvic Pain Syndrome in Men?
Chronic Pelvic Pain Syndrome generally does not result from a prostate infection, even though many men are told it does. Instead, several potential factors, primarily related to how the pelvic floor interacts with other body systems, are often responsible.
- Lumbar pathology: Nerves that serve the pelvic area originate in the lower back. Issues such as lumbar disc bulges, spinal arthritis, or nerve irritation can cause pain to radiate forward into the pelvis, making it feel like it is coming from the prostate even though the underlying cause is the spine.
- Vascular pathology: Circulatory disturbances, including varicoceles, pelvic venous congestion, or altered blood flow, can produce aching, heaviness, or pressure that closely mimics prostate discomfort.
- Pelvic floor pathology: The pelvic floor muscles create a supportive hammock under the pelvis. When these muscles tighten, spasm, or lose proper coordination, they can irritate nerves and generate pain that feels as though it is coming from the prostate or bladder, but in reality, the muscles themselves are often the primary source of the problem.
Other contributing factors can include:
- Past surgeries such as vasectomy or prostate procedures
- Structural issues like hip dysfunction, scoliosis, or leg length differences
- Excessive or sudden changes in exercise
- Long hours of sitting
- Chronic constipation or frequent straining
- Trauma or stress to the pelvic area
Even though numerous factors might aggravate chronic pelvic pain, most men, particularly those struggling with urinary or bowel disturbances, have a primary issue rooted in pelvic floor dysfunction.
Symptoms of Chronic Pelvic Pain Syndrome
CPPS symptoms can be perplexing because they frequently resemble prostate or bladder problems even when the real cause lies in the muscles of the pelvic floor. Men who experience CPPS may notice:
- Aching, pressure, or sharp pain in the perineum, pubic area, or lower abdomen
- Discomfort that feels like it’s coming from the testicles, tip of the penis, or inside the urethra
- Urgency, frequency, weak stream, or the sensation that you can’t fully empty your bladder
- Burning or stinging, even when no infection is present
- Pain with or after ejaculation, erectile discomfort, or reduced sexual satisfaction
- Tightness or aching that overlaps with pelvic discomfort
- A sense of heaviness, pressure, or tight muscles in the pelvic floor area
Associated Diagnoses
Chronic pelvic pain in men can be related to several well-known medical conditions. Some stem from the spine, others from blood vessel complications, and many involve the pelvic floor muscles themselves.
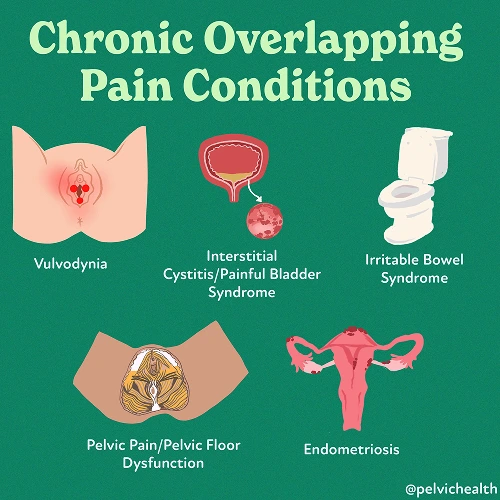
Low back concerns such as lumbar nerve compression, disc degeneration, or joint arthritis can irritate nerves that extend into the pelvic region, leading to discomfort that feels identical to prostate pain. Problems like varicocele, testicular torsion, or pelvic venous congestion can disrupt circulation and cause dull aching, heaviness, or sharp stinging pain. Although Chronic Pelvic Pain Syndrome is the most frequently identified issue, pelvic floor dysfunction often appears alongside pudendal neuralgia, painful bladder syndrome, or even hard flaccid syndrome.
In a large number of cases, dysfunction of the pelvic floor becomes the connecting factor, directly generating pain or worsening symptoms that originate from spinal or vascular causes.
Diagnostic Challenges
Many men with CPPS face years of uncertainty before receiving the correct diagnosis. It is not uncommon to be told that the issue is prostatitis and to be treated with antibiotics even though testing shows no infection. In fact, research demonstrates that more than 90% of men who report pelvic or urogenital pain symptoms do not actually have a bacterial infection in their prostate.
Most of these men belong to the Category III group under the National Institutes of Health (NIH) prostatitis classification system. The NIH divides prostatitis into five main categories:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Most of these men belong to the Category III group under the National Institutes of Health (NIH) prostatitis classification system. The NIH divides prostatitis into five main categories:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Because both spinal and vascular conditions can cause discomfort that feels like pelvic floor pain, test results often appear normal, offering little insight. Without clear answers, men are frequently sent from doctor to doctor and prescribed antibiotics that do not bring relief. The process can be discouraging until they discover that pelvic floor physical and occupational therapy focuses on correcting the true cause of their pain, allowing for meaningful and lasting improvement.
Symptoms of Chronic Pelvic Pain Syndrome
Because CPPS is not usually caused by an infection, treatment focuses on function and balance instead of antibiotics. The goal is to normalize the pelvic floor, calm the nerves, and address other physical systems that could be worsening pain or tension.
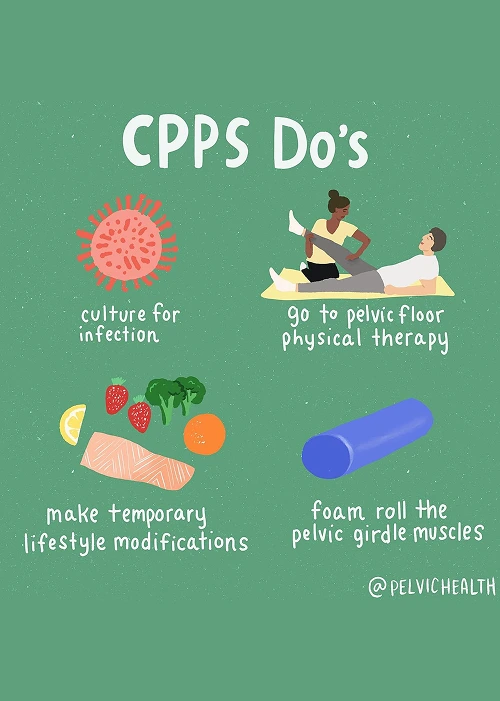
- Pelvic floor physical and occupational therapy: This remains the cornerstone of effective treatment. By releasing tight muscles, retraining movement coordination, and quieting irritated nerves, therapy helps reduce pain and restore comfort.
- Spine and back treatment: When the source of discomfort involves the lower back or sciatic nerves, therapy addresses mobility, posture, and spinal alignment. In some cases, your physician may add injections to reduce inflammation.
- Vascular-related treatment: Circulatory tension can heighten pain. Through posture work, relaxation, and breathing exercises, pelvic floor therapy improves blood flow and relieves congestion in the veins.
- Biomechanical support: Correcting alignment or movement restrictions in the hips and pelvis helps distribute pressure evenly, preventing added strain on the pelvic area.
- Lifestyle adjustments: Day-to-day changes like managing bowel health, limiting sitting time, and incorporating movement gently into your routine can all make a difference in symptom management.
How We Can Help with Your Chronic Pelvic Pain
For men in Echo Park living with chronic pelvic pain, the path to recovery can feel long and uncertain. You may have tried multiple antibiotics, received different opinions from various providers, and still haven’t found lasting relief. At PHRC, we understand your frustration, which is why we provide focused evaluations led by pelvic floor physical and occupational therapists who specialize in men’s pelvic health.
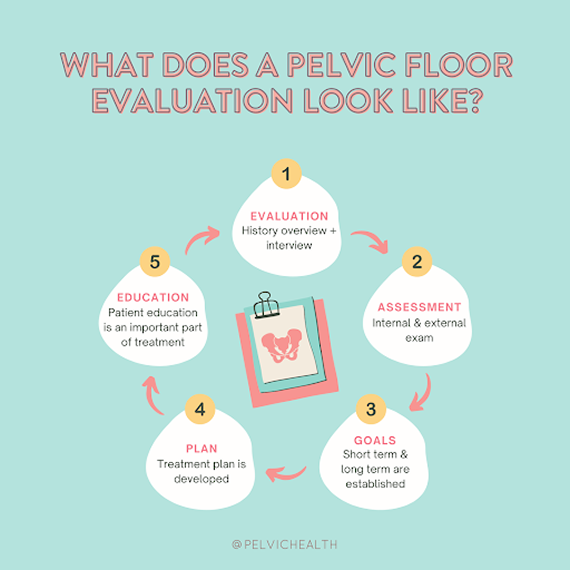
Your evaluation begins with an open, detailed conversation about your symptoms, medical history, and the treatments you’ve already attempted. Your therapist will take time to understand your story, including how your symptoms affect your work, relationships, and everyday life. We know this journey can be incredibly tiring, so we prioritize compassion, patience, and clear communication.
How We Can Help with Your Chronic Pelvic Pain
For men in Echo Park living with chronic pelvic pain, the path to recovery can feel long and uncertain. You may have tried multiple antibiotics, received different opinions from various providers, and still haven’t found lasting relief. At PHRC, we understand your frustration, which is why we provide focused evaluations led by pelvic floor physical and occupational therapists who specialize in men’s pelvic health.
Your evaluation begins with an open, detailed conversation about your symptoms, medical history, and the treatments you’ve already attempted. Your therapist will take time to understand your story, including how your symptoms affect your work, relationships, and everyday life. We know this journey can be incredibly tiring, so we prioritize compassion, patience, and clear communication.
During your physical exam, your PHRC therapist will assess your pelvic floor muscles, nerves, tissues, and movement patterns. After completing the evaluation, we’ll share the findings with you and explain how your pain likely developed. Together, we’ll design an individualized plan that addresses both immediate and long-term goals.
Typically, therapy sessions occur one to two times per week for approximately twelve weeks, paired with a tailored home exercise program to reinforce your progress. Your PHRC therapist will also coordinate your care with any other medical professionals involved in your treatment. Our goal is to help you move forward with confidence, free from the pain that has been holding you back.
