
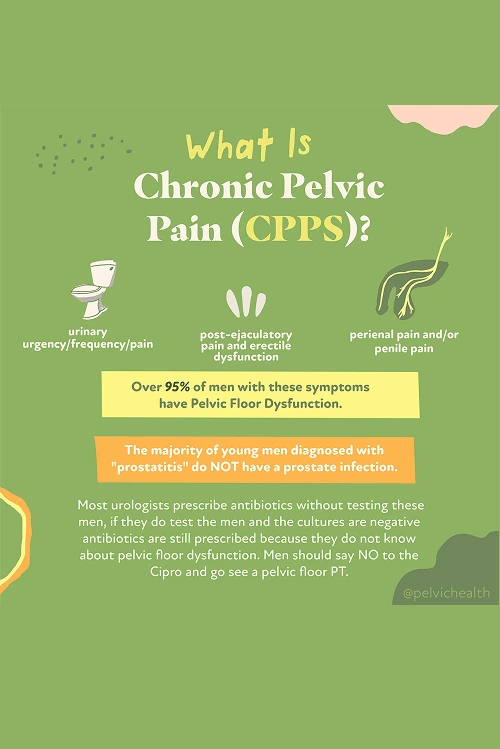
If you’re living in Silverlake and dealing with unrelenting pelvic pain, trouble urinating, or ongoing sexual symptoms, you are not the only one facing this challenge. Chronic prostatitis, also known as Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS), affects a large number of men, regardless of age. In fact, approximately 10% of men will deal with prostatitis-like issues at some point in their lives.
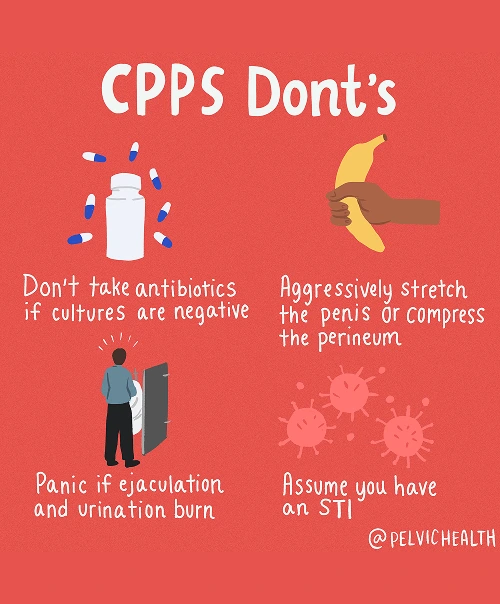
Surprisingly, medical studies show that about 97% of these cases do not stem from an actual prostate or bladder infection, even though antibiotics are often prescribed. The true cause often lies in the pelvic floor muscles. When these muscles tighten, spasm, or fail to coordinate properly, they can produce pain and urinary symptoms that mimic prostate inflammation.
For men in Silverlake experiencing these frustrating symptoms, pelvic floor physical and occupational therapy provides a highly effective, non-invasive path toward relief. At PHRC, our pelvic health specialists focus on improving the way your pelvic muscles function. Through gentle, evidence-based treatment techniques, we work to release muscle tension, restore proper movement, and help you overcome the discomfort that has been holding you back.
What are the Causes of Chronic Pelvic Pain Syndrome in Men?
Chronic Pelvic Pain Syndrome is rarely the result of a prostate infection, even though many men are told it is. Instead, the condition usually arises from several different potential causes, most of which relate to how the pelvic floor interacts with the body’s other systems.
- Lumbar pathology: Nerves that serve the pelvic region originate in the lower spine. Conditions such as disc herniation, arthritis, or nerve irritation in this area can create pain that radiates forward, mimicking pelvic or prostate discomfort, despite the spine being the actual source.
- Vascular pathology: Blood flow problems in the pelvic region, including varicoceles, venous congestion, or reduced circulation, can produce sensations of aching or heaviness that feel similar to prostate pain.
- Pelvic floor pathology: The pelvic floor muscles form a supportive layer beneath the pelvis. When these muscles tighten, spasm, or fail to coordinate properly, they can irritate nerves and generate pain that seems to come from the prostate or bladder, but in truth, the dysfunction in the pelvic floor is often the primary cause.
Other contributing factors can include:
- Past surgeries such as vasectomy or prostate procedures
- Structural issues like hip dysfunction, scoliosis, or leg length differences
- Excessive or sudden changes in exercise
- Long hours of sitting
- Chronic constipation or frequent straining
- Trauma or stress to the pelvic area
Though many potential contributors exist, most men with persistent pelvic discomfort and related urinary or bowel symptoms share a common root cause: pelvic floor dysfunction.
Symptoms of Chronic Pelvic Pain Syndrome
Men dealing with CPPS often find the symptoms puzzling because they mimic prostate or bladder problems, even though the source might actually be within the pelvic floor muscles. You may notice several of the following:
- Aching, pressure, or sharp pain in the perineum, pubic area, or lower abdomen
- Discomfort that feels like it’s coming from the testicles, tip of the penis, or inside the urethra
- Urgency, frequency, weak stream, or the sensation that you can’t fully empty your bladder
- Burning or stinging, even when no infection is present
- Pain with or after ejaculation, erectile discomfort, or reduced sexual satisfaction
- Tightness or aching that overlaps with pelvic discomfort
- A sense of heaviness, pressure, or tight muscles in the pelvic floor area
Associated Diagnoses
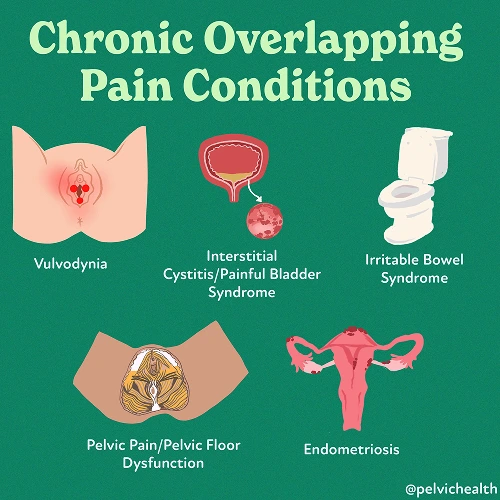
Chronic pelvic discomfort in men can stem from numerous identifiable conditions that involve different parts of the body. Some are associated with spinal nerve irritation, others with circulation or vascular tension, and many are rooted in the muscles of the pelvic floor.
Spinal issues like lumbar disc herniation, arthritis, or nerve entrapment can send pain signals into the pelvic area, resembling inflammation of the prostate. Conditions such as varicocele, torsion of the testicles, or venous congestion within the pelvis can disrupt blood movement and produce sensations of pressure, aching, or intermittent pain. Chronic Pelvic Pain Syndrome is often diagnosed most commonly, but pelvic floor dysfunction may also accompany pudendal neuralgia, interstitial cystitis, or hard flaccid syndrome.
In many of these situations, the pelvic floor acts as the underlying driver, either directly producing pain or amplifying existing irritation from the spine or blood vessels.
Diagnostic Challenges
Getting the right diagnosis is often one of the most difficult parts of managing CPPS. Many men are initially told they have prostatitis and are prescribed antibiotics even though no infection is actually identified. In fact, studies show that over 90% of men with pelvic or urinary pain do not have a bacterial infection of the prostate.
Most men with these symptoms belong to the Category III classification of prostatitis according to the National Institutes of Health (NIH). The categories are described as follows:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
Most men with these symptoms belong to the Category III classification of prostatitis according to the National Institutes of Health (NIH). The categories are described as follows:
- Category I: Acute bacterial prostatitis (true infection, sudden and severe)
- Category II: Chronic bacterial prostatitis (chronic infection, often with repeat UTIs)
- Category IIIa: Inflammatory CPPS (white blood cells seen on testing, but no bacteria)
- Category IIIb: Non-inflammatory CPPS (no white blood cells or infection, but symptoms are present)
- Category IV: Asymptomatic inflammatory prostatitis (inflammation without symptoms)
When lumbar or vascular dysfunction mimics pelvic floor pain, test results often fail to reveal what’s really happening. Many men are told that everything looks normal, which can be both confusing and frustrating. Because of this, they may undergo multiple courses of antibiotics and see several specialists before discovering that their pain actually stems from pelvic floor muscle dysfunction. Pelvic floor physical and occupational therapy can finally provide the clarity and targeted care needed for recovery.
Symptoms of Chronic Pelvic Pain Syndrome
Since CPPS is rarely caused by a true bacterial infection, the treatment strategy looks very different from simply using antibiotics. The emphasis is on correcting pelvic floor muscle dysfunction, reducing nerve irritation, and considering all other physical factors that influence pain.
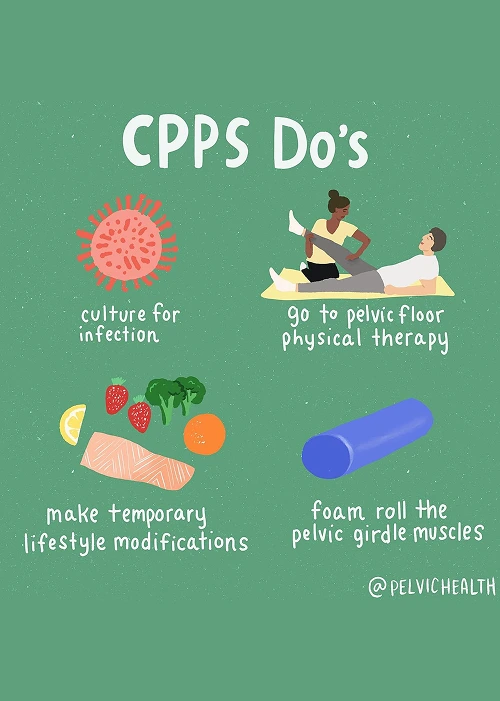
- Pelvic floor physical and occupational therapy: This forms the core of most treatment plans. The therapy helps relax overactive muscles, retrain proper movement coordination, and decrease the nerve hypersensitivity responsible for pain and urinary symptoms.
- Spine and back treatment: When discomfort originates from the lumbar spine or nerves in the lower back, therapy focuses on improving posture, flexibility, and joint mobility. Physicians may sometimes include injections for additional relief.
- Vascular-related treatment: Limited blood flow can worsen pelvic pain. Pelvic floor therapy addresses this by releasing tight muscles, improving circulation through breathing and posture correction, and easing pressure on pelvic
- Biomechanical support: Restoring balance in the hips and lower back reduces pelvic strain, allowing smoother movement and lessening muscular
- Lifestyle adjustments: Small yet meaningful changes, such as reducing prolonged sitting, preventing constipation, and pacing your physical activity, go a long way toward long-term management of symptoms.
How We Can Help with Your Chronic Pelvic Pain
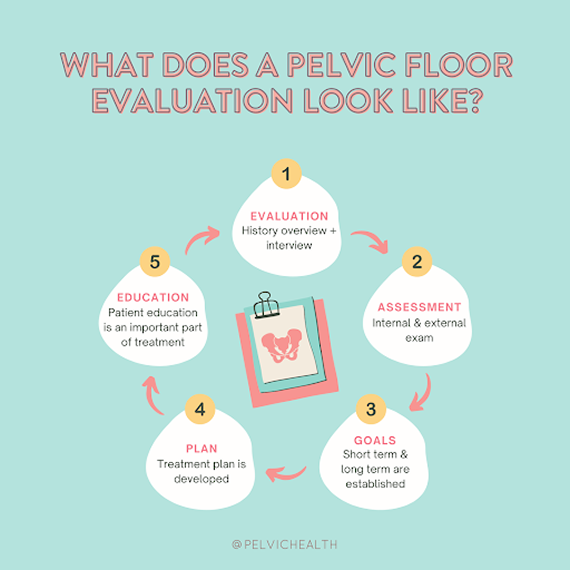
Men in Silverlake who live with chronic pelvic pain often describe feeling stuck and frustrated after months or even years of searching for answers. You may have been prescribed antibiotics several times, consulted multiple doctors, and still don’t know why your symptoms persist. When you come to PHRC, you’ll receive a focused evaluation with a pelvic floor physical or occupational therapist who specializes in treating pelvic pain in men.
Your evaluation will begin with an in-depth review of your medical background, previous diagnoses, and treatments you’ve already attempted. Your therapist will take time to understand your unique history and how your symptoms have affected your day-to-day life. We know this process can be both emotionally and physically exhausting, which is why we take great care to ensure you feel comfortable and heard throughout.
How We Can Help with Your Chronic Pelvic Pain
Men in Silverlake who live with chronic pelvic pain often describe feeling stuck and frustrated after months or even years of searching for answers. You may have been prescribed antibiotics several times, consulted multiple doctors, and still don’t know why your symptoms persist. When you come to PHRC, you’ll receive a focused evaluation with a pelvic floor physical or occupational therapist who specializes in treating pelvic pain in men.
Your evaluation will begin with an in-depth review of your medical background, previous diagnoses, and treatments you’ve already attempted. Your therapist will take time to understand your unique history and how your symptoms have affected your day-to-day life. We know this process can be both emotionally and physically exhausting, which is why we take great care to ensure you feel comfortable and heard throughout.
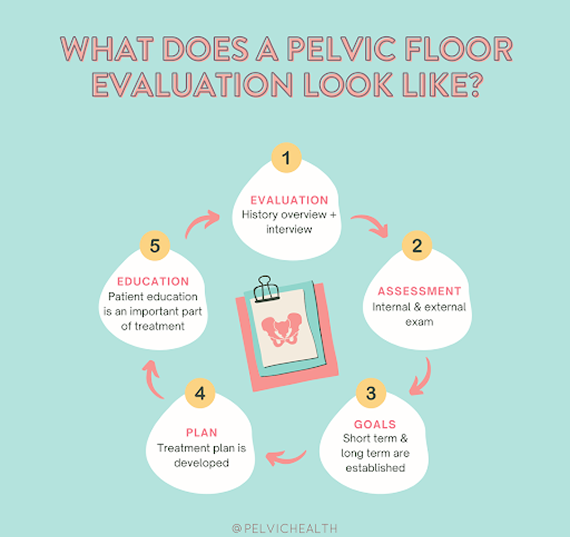
The physical assessment will involve examining your muscles, nerves, joints, and overall pelvic floor function. Once your therapist completes the evaluation, they’ll review their findings and provide a clear explanation of what may be contributing to your pain. You’ll work together to create a structured plan that includes short- and long-term recovery goals.
Typically, pelvic floor therapy at PHRC takes place one to two times per week for about twelve weeks. You’ll also be given specific exercises to do at home to enhance your results. Your PHRC therapist will coordinate your care with your broader medical team to support every aspect of your recovery. Our goal is to help you finally achieve relief and return to a more comfortable, active life.
