
The Facts
Ehlers-Danlos Syndrome is a group of genetic conditions that affect how the body builds and maintains connective tissue (the material that supports skin, joints, blood vessels, and organs). When connective tissue is weak or too stretchy, it can lead to joint instability, fragile skin, and a range of physical symptoms.
There are 13 recognized subtypes of EDS, each with its own characteristics. Hypermobile EDS (hEDS) is the most common subtype and currently has no known genetic marker, which makes diagnosis more difficult.
People with EDS often appear healthy, but the underlying tissue fragility and joint hypermobility can cause chronic pain, fatigue, and functional challenges. Although it affects roughly 3% of the global population, EDS is often underdiagnosed or misdiagnosed. Recognizing symptoms early and working with a knowledgeable care team can improve long-term outcomes.
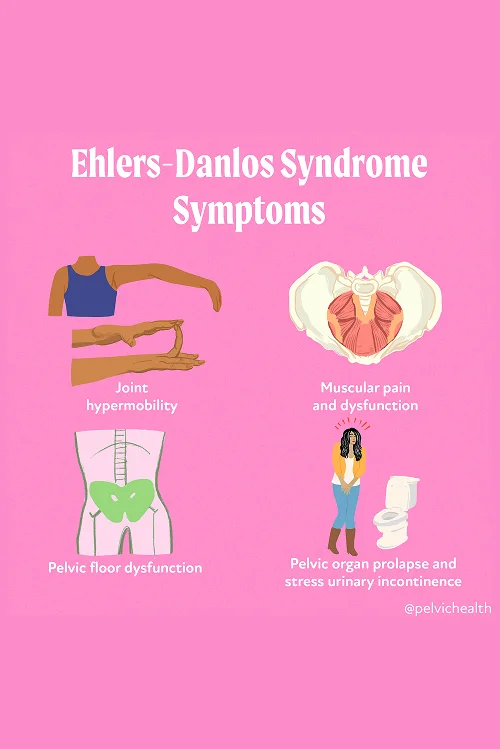
Symptoms of Ehlers-Danlos Syndrome
EDS symptoms vary, but the most commonly reported issues include joint hypermobility, headache, arthritis, IBS, poor wound healing, nerve compression, and more (pictured below).
Associated Diagnoses
People with Ehlers-Danlos Syndrome often experience a range of coexisting conditions that complicate both diagnosis and treatment. Common associated diagnoses include:
- Hypermobility Spectrum Disorder (HSD): Shares many features with hEDS but does not meet full diagnostic criteria.
- Postural Orthostatic Tachycardia Syndrome (POTS): Causes dizziness, fatigue, and rapid heartbeat when standing.
- Mast Cell Activation Syndrome (MCAS): Leads to allergic-like reactions from seemingly harmless triggers.
- Chronic Fatigue and Pain Syndromes: Persistent exhaustion that doesn’t improve with rest.
- Neurodivergence and Anxiety Disorders: Often reported alongside physical symptoms, and can influence how patients are perceived and treated by the medical system.
These above conditions frequently overlap and interact, requiring a nuanced and multidisciplinary approach to care.
Causes of Ehlers-Danlos Syndrome
EDS is a genetic disorder caused by mutations that disrupt collagen synthesis and structure. Collagen is a major component of connective tissue, providing strength and flexibility to skin, joints, blood vessels, and internal organs. In most subtypes of EDS, a specific genetic mutation can be identified. However, in the case of hypermobile EDS, no genetic marker has yet been discovered, which adds to the complexity of diagnosis and research. The inheritance pattern varies by subtype but often runs in families.
Diagnostic Challenges
Diagnosing EDS, especially hEDS, can be difficult and is often delayed. The lack of a known genetic marker for hEDS means that diagnosis relies heavily on clinical criteria, patient history, and a thorough physical exam. Additionally, symptoms can mimic or overlap with other disorders, leading to years of misdiagnosis or dismissal. Many patients report feeling invalidated or gaslighted by providers unfamiliar with connective tissue disorders. At PHRC, we take a trauma-informed approach to care, listening carefully to each patient’s experience and working collaboratively with specialists to reach an accurate diagnosis and build a sustainable treatment plan.
How Does the Pelvic Floor Contribute to EDS?
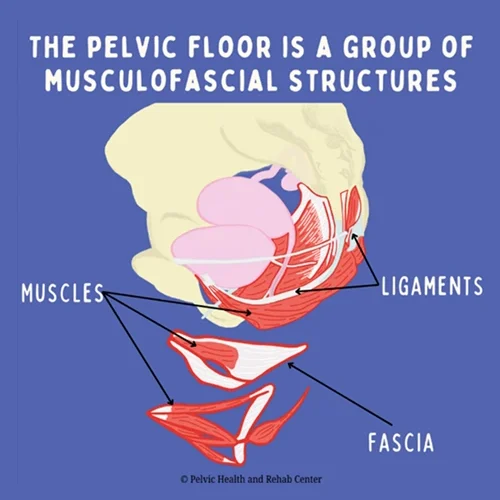
The pelvic floor plays a key role in stabilizing the body, supporting pelvic organs, and managing bladder, bowel, and sexual function. In people with EDS, the connective tissues that make up and support the pelvic floor can be weak or overly elastic. This lack of structural integrity can lead to a range of symptoms, including pelvic organ prolapse, urinary or fecal leakage, pain with intercourse, and generalized pelvic pain.
Because the pelvic floor relies on collagen for strength and elasticity, the collagen defects present in EDS can disrupt normal function. Muscles may become overactive to compensate for instability or underactive due to fatigue and pain. At PHRC, we understand this complex interplay and address not only the muscular and structural imbalances but also the nervous system’s role in chronic pain and dysfunction.
How Does the Pelvic Floor Contribute to EDS?
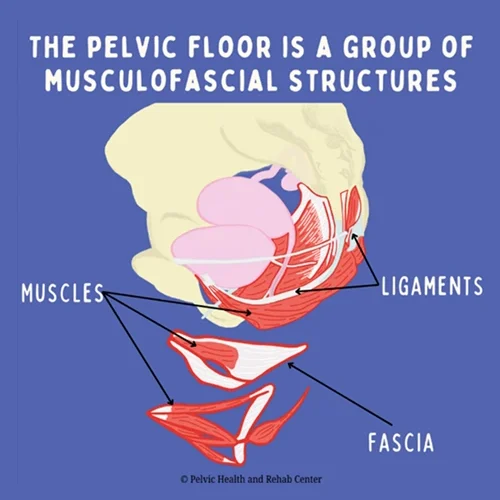
The pelvic floor plays a key role in stabilizing the body, supporting pelvic organs, and managing bladder, bowel, and sexual function. In people with EDS, the connective tissues that make up and support the pelvic floor can be weak or overly elastic. This lack of structural integrity can lead to a range of symptoms, including pelvic organ prolapse, urinary or fecal leakage, pain with intercourse, and generalized pelvic pain.
Because the pelvic floor relies on collagen for strength and elasticity, the collagen defects present in EDS can disrupt normal function. Muscles may become overactive to compensate for instability or underactive due to fatigue and pain. At PHRC, we understand this complex interplay and address not only the muscular and structural imbalances but also the nervous system’s role in chronic pain and dysfunction.
How Our Team at PHRC Can Help You
Treating Ehlers-Danlos Syndrome requires much more than a standard physical and occupational therapy plan. At PHRC, we approach each patient with EDS through a personalized, hands-on, and collaborative model. Pelvic floor therapy for EDS is not just about building strength, it’s about understanding how your connective tissue, nervous system, and musculoskeletal patterns interact and contribute to symptoms like pain, instability, and dysfunction.
We start treatment with a thorough one-on-one evaluation. Your therapist takes time to understand your full medical history, coexisting conditions, past treatments, and current quality of life. We listen carefully, especially because many patients come to us feeling dismissed by other providers. From there, we build a care plan that’s realistic, flexible, and specifically geared toward your body’s unique needs.
How Our Team at PHRC Can Help You
Treating Ehlers-Danlos Syndrome requires much more than a standard physical and occupational therapy plan. At PHRC, we approach each patient with EDS through a personalized, hands-on, and collaborative model. Pelvic floor therapy for EDS is not just about building strength, it’s about understanding how your connective tissue, nervous system, and musculoskeletal patterns interact and contribute to symptoms like pain, instability, and dysfunction.
We start treatment with a thorough one-on-one evaluation. Your therapist takes time to understand your full medical history, coexisting conditions, past treatments, and current quality of life. We listen carefully, especially because many patients come to us feeling dismissed by other providers. From there, we build a care plan that’s realistic, flexible, and specifically geared toward your body’s unique needs.
At PHRC, we use an individualized, evidence-informed approach to help patients with EDS manage symptoms, build stability, and improve function. Our care combines manual therapy, patient education, and collaboration with your extended medical team.
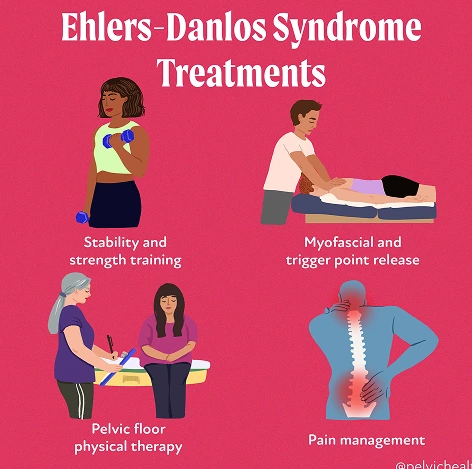
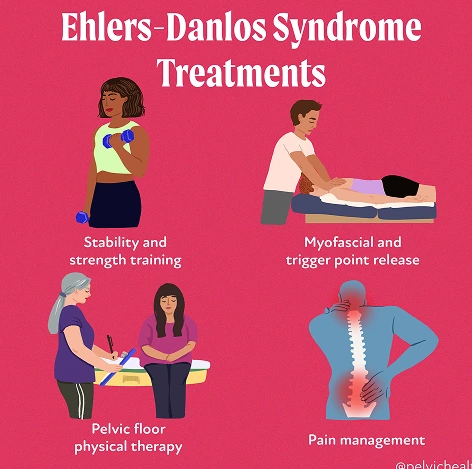
Treatment options include:
- Pelvic Floor physical and occupational therapy: One-on-one sessions that assess and treat the muscles, nerves, and connective tissue of the pelvic floor to reduce pain and improve function.
- Myofascial and Trigger Point Release: Hands-on techniques to reduce muscle tension, improve tissue mobility, and address overactive or tight areas contributing to pain.
- Stability and Strength Training: Targeted exercises that focus on safely building strength in the core, hips, and pelvic floor while respecting joint hypermobility.
- Pain Management: Practical strategies to reduce flare-ups, calm the nervous system, and help you regain control over daily life.
- Posture and Movement Retraining: Corrections to movement habits that strain joints or tissues, with a focus on safer alignment and long-term relief.
- Functional Rehabilitation: Gradual return-to-activity planning to build stamina and confidence while avoiding setbacks.
- Education and Support: Tools and tips for energy conservation, symptom tracking, and pacing that support daily routines.
- Collaborative Care: We coordinate with pelvic pain specialists, allergy experts, surgeons, and others involved in your care for a fully integrated approach.
Additionally, if you experience sexual pain, bladder or bowel dysfunction, or ongoing pelvic discomfort, pelvic floor therapy can help identify how your muscles and tissues are involved. Through careful assessment of your joints, nerves, muscles, and movement, we determine what’s contributing to your symptoms and what can be improved.
Most treatment plans involve weekly or biweekly sessions over a few months, with a mix of in-person work and home strategies. No two cases of EDS are alike, and we approach every patient with that in mind. At PHRC, we’re here to help you feel more in control of your body, reduce pain, and regain the confidence to move through life again.
Find Relief at PHRC
At PHRC, our goal is to provide compassionate and comprehensive care to help you manage and overcome pain from EDS. By understanding the underlying causes and providing targeted treatments, we work to improve your quality of life and restore your health.
We also recognize the challenges some people might face in accessing in-person care, which is why we offer virtual sessions through telehealth after your initial consultation. These sessions allow for continuity of care and accessibility for those unable to travel to one of our clinics.
