Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By: Melinda Fontaine, DPT, PHRC Walnut Creek
Lube is great! It adds moisture and decreases friction, but how do you pick from the multitude of different personal lubes on the market? Which one is the safest? Goop recently asked the same questions in response to watching an episode of Grace and Frankie in which Frankie makes her own lube. I have noticed a number of my patients can have very strong reactions to lubes including pain infection and fertility issues. Let’s take a look at what we are putting in our bodies.
What’s the Difference Between Moisturizers and Lubricants?
It’s all based on how long it is intended to stay in the body. Vaginal moisturizers are made to stay in the body for longer than 60 minutes, and are applied every 1-3 days to alleviate dryness. Vaginal moisturizers are classified as Medical Devices by the Medicines and Healthcare products Regulatory Agency because they last so long, which means they have been tested for safety and efficacy. They last so long because they contain polymers to adhere water to the vaginal lining. Lubricants are made to be used short term during sex. Some may be better than others for various activities.
Which Lube can I use with condoms or toys?
Lubricants may be water-, silicone-, mineral oil-, or plant-based. Water-based lubricants are non-staining, easy to wash off, and safe to use with all condoms and toys. Silicone-based lubricants are thicker and tend to hang around longer, so they are preferred by women who are past menopause or don’t want their lube to disappear too quickly. However, silicone-based lube required soap and water to get off and should not be used on silicone toys because it will basically dissolve the toy. Oil-based lubricants are least likely to irritate vaginal or anal tissues but cannot be used with condoms because they will break, and should not be used with toys because it will coat them in oil and prevent them from ever getting clean. Plant based-lubes, such as aloe vera are generally considered safe.
Can I Get an Infection from Lube?
Products, such as KY Jelly, Replens, Gynol II, and Astroglide leave you vulnerable to infection because they kill the good bacteria, lactobacilli, that keep you healthy. You may have noticed that everyone is talking about probiotics to replenish the good bacteria in our gut. Our vaginas and rectums also have good bacteria that play a vital role in our health. An important type of good bacteria called lactobacillus maintains a good pH in the vagina and prevents bacterial vaginosis. Low estrogen levels (as occur post menopause, postpartum, and after prolonged use of oral contraceptives) also reduce the vaginal pH and can lead to infection. Healthy vaginal pH is 3.8-4.5, and rectal pH is about 7.0. A good lube would have a pH value similar to your tissues or slightly higher.
What is Osmolality and What Does it Have to Do with Lube?
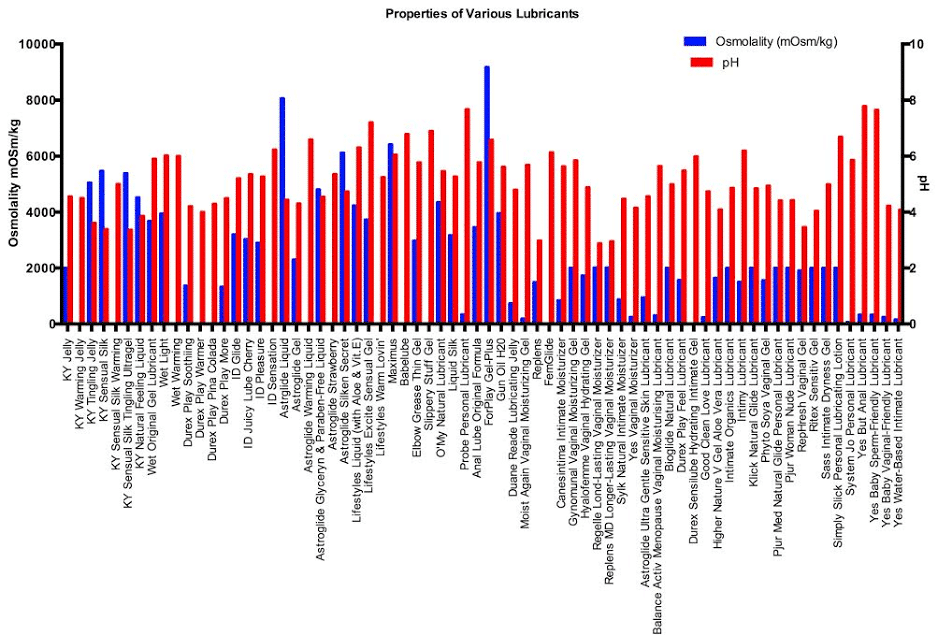
Osmolality is the concentration, or how many solutes are present in the lube. Products with high osmolality lead to damage of the tissues lining the vagina or rectum, causing irritation and leaving the tissues vulnerable to infection². The World Health Organization (WHO) recommends osmolalities of less than 380 mOsm/kg, or at most 1200 mOsm/kg. For example, Astroglide Liquid has an osmolality of 8064 and should be avoided. Lubes with osmolalities less than 316 mOsm/kg showed no adverse effects and include Good Clean Love, Slippery Stuff, Sliquid, Babelube, Probe, and Femglide. Silicone-, Plant, and Oil-based lube are also less likely to irritate, but their osmolality cannot be measured. See the figure for some common water-based lubricants with their osmolalities and pH values³.
What Else Could Be in My Lube?
Parabens, glycols, microbicides, and preservatives in many personal lubricants and moisturizers are also concerning. Most lubricants list the ingredients on the package, so you can find out what is in your lube. Parabens are preservatives and are similar to the female sex hormone, estrogen. It has been suggested that they may disrupt the endocrine system function in both sexes, and they have been detected in breast tumors. Glycols are molecules responsible for maintaining moisture, so they are used in many lubes, such as Durex Play Feel, ID Glide, and Pjur Woman Nude. Too much glycol can lead to vulnerability to herpes simplex virus 2, bacterial vaginosis, and yeast infections¹. The WHO advises that glycerol should be less than 9.9% mass fraction and propylene glycol should be less than 8.3% mass fraction³. Nonoxynol-9 is a compound added to lubes, such as Gynol II, for contraception because it kills sperm. It also damages the vaginal and rectal lining and increases risk for herpes and HIV². Chlorhexidine is a preservative associated with a 100-fold increased susceptibility to chlamydia¹ and is in KY Jelly and Astroglide.
How Does Lube Affect Fertility?
Some products, such as Astroglide, KY Jelly, and Replens, make it hard for little swimmers to swim, while sperm-friendly lubes (Pre-Seed and Yes Baby) have no effect². Low pH and high osmolality decrease sperm motility. The best conditions for sperm survival is pH 7.2-8.5 and osmolality 270-360 mOsm/kg. Interestingly, studies done on couples trying to conceive did not find a difference in fertility between couples who did and did not use lube¹.
What Lube Do you Recommend for People with Pelvic Pain?
Lubes that cause damage and irritation to the lining of the vagina or rectum can create pelvic pain or make existing pain worse.
- Pure coconut oil or aloe vera are the least irritating, but remember oil cannot be used with condoms.
- Silicone-based lubes without the above listed preservatives would be my second choice for someone with pelvic pain and can be used with condoms.
- Of the water-based lubes tested, Good Clean Love, Slippery Stuff, and Sliquid Organic are the safest.
- For couples trying to conceive, I recommend Yes Baby Sperm-Friendly Lubricant.
- For, anal play, a lube should have a higher pH, so I would choose Yes But Anal Lube.
- Lastly, in order to avoid tissue damage and infection, everyone should steer clear of the ever popular KY Jelly and Astroglide.
Every person has different preferences and tolerances, so experiment a little to find out what works for you. If you are plagued by recurrent infections or chronic pain, it might be worthwhile as Dr. Maggie Ney suggests, to take a break from all lubricant to see if it improves.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual physical and occupational therapy appointments too!
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Like us on Facebook,
Subscribe to our YouTube Channel,
and follow us on Twitter, Instagram, Tik Tok and Pinterest!
References
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Stephanie Prendergast, MPT, Cofounder, PHRC Los Angeles
The Situation Room: Why do men have to see Women’s Health Physical and Occupational Therapistss?
The facts:
15% of adult men worldwide suffer from pelvic pain. 1
8.2% of men will experience prostatitis-like symptoms at some point in their lives, and greater than 90% of those men will have symptoms consistent with chronic pelvic pain syndrome (CPPS).2,3
Symptoms of CPPS can include
- Penile/scrotal/perineal pain
- Urinary urgency/frequency
- Erectile dysfunction
- Post-ejaculatory pain
- Painful bowel movements or delayed genital/bladder pain after bowel movements
The situation:
CPPS symptoms drive men to the urologist. Tests come back normal. Men turn to Google University and usually self-diagnose themselves with pudendal neuralgia, nonbacterial chronic prostatitis, or CPPS. They discover they need pelvic floor physical and occupational therapy. They look for one…and discover that they need to see a “Woman’s Health” physical and occupational therapists?!? As if this isn’t bad enough, men then find out that many of these physical and occupational therapistss do not treat men.
Aw, NUTS!!
When it comes to physical and occupational therapy training in male pelvic floor dysfunction, we are facing a multifactorial problem. Course instructors are frustrated. Pelvic floor physical and occupational therapistss do not feel qualified based on the training. Suffering men do not know where to go for treatment, creating one more hurdle in the obstacle course of recovering from pelvic pain.
Pelvic floor muscle evaluations and treatment are STILL not yet part of the regular medical and physical and occupational therapy school curricula. Liz and I were trained on the job; we learned how to do examinations on male and female patients, starting on day 1 of our careers. This situation is not common. Instead, many physical and occupational therapistss gain pelvic floor training through continuing education courses. These courses are typically 2-3 days in length, or roughly 16 -24 hours of training. A typical course costs about $600-800 and likely involve a weekend in a bad hotel, airline ticket, and meal expenses. Physical therapists may receive a continuing education allowance for such courses of roughly $500 – $1000 per year. So, physical and occupational therapistss may be able to take about one course per year for their training.
I was horrified at my first course to learn that in these courses there are no models; we are instructed to drop our drawers and practice on each other.
The majority of pelvic floor physical and occupational therapistss are women and as a result, there are often no men in these courses. The obvious problem with this is that in the course on male pelvic health, the physical and occupational therapistss are practicing on women, not men. This does not necessarily foster confidence in the student about how to transition their new knowledge to a clinical setting. We understand this.
Several years ago, Liz and I wanted to solve this problem by hosting a course on male pelvic pain with male models. Imagine trying to hire ten models that will allow twenty women to practice pelvic floor techniques on them, for four hours a day. It was an administrative nightmare for us and raised the cost of the course to an unaffordable number for potential students.
Sandy Hilton, PT, DPT, MS, co-owner of Entropy Physical and Occupational Therapy in Chicago, and Tracy Sher, MPT, CSCS, owner of Sher Pelvic Health in Orlando and founder of Pelvic Guru, shared similar frustrations.
Sandy brought up an interesting double standard:
“Most “Men’s Health” physio courses do not require that there be male models for the assessments. I think this is unhelpful and misses an opportunity to teach comfort and confidence to the participants. If a woman comes to a pelvic health course but can’t participate in labs, she is to provide a model, if a guy goes to a pelvic health course he is to bring a female for the labs… but in the men’s health courses the females are not required to bring a male for the labs… and the courses are done anyway, leaving participants not fully prepared for their first real male patient!”
This is an excellent point. Out of curiosity I asked my partner last night if he would attend a weekend course with me and allow me to practice on his perineum for a few hours in a room full of people. He laughed right in my face and the thought of this made me laugh as well. However, this is a noted fair and practical point.
Sandy goes on to say:
“Not every pelvic health therapist wants to treat men. And they should not treat men if they are not interested or comfortable with male pelvic health challenges. And they should rapidly refer to those of us who ARE!
Around the country there are different attitudes about women treating men, and men treating women. I think this is probably part of why some female pelvic health therapists chose to not treat men. I don’t think they are comfortable, or they work in settings that are so “pink” that a man wouldn’t be comfortable there.”
Tracy adds:
“ Some female therapists simply don’t feel comfortable treating men when it comes to the pelvic region; and thus, they do not seek out additional training for this. Some would say, “oh, just get over it,” it’s more complex than that. Just as patients may have anxieties and fears about coming in for care for the pelvic region, practitioners also have their own anxieties and concerns. This can reflect personal, cultural, religious or other factors. Though it is all professional in a medical setting, this type of therapy does involve touching the pelvic region and talking about very intimate topics.
When there’s a female therapist/male patient dynamic, some therapists would only feel comfortable treating if an assistant or another person was in the room. In some practices this is not always an available option”.
Troubleshooting the situation
Knowing our own challenges trying to host a course, I asked Tracy and Sandy how they are helping to improve male pelvic health physical and occupational therapy training.
From Sandy:
Sarah Haag and I have an Introduction to Men’s Health course which utilizes Male Standardized Patients for the lab portion. There is no pre-requisite for this course, other than having a license that allows you to do internal pelvic assessments and treatment. We welcome women and men to the course and the standardized patients provide valuable feedback. I credit Karen Liberi for this, her and I taught a men’s health course in Portland Maine some years ago based on this format.
A standardized patient (SP) (or a patient model) is the reference for those people who are paid as professional patients. Major teaching hospitals have them – that’s who the MDs and RNs train on – as opposed to PTs who volunteer as lab models!
We hire them – and they know how many internal pelvic exams they are able to do in a set amount of time. Depending on the class size, you would do some simple math to know how many ‘patients’ you would need to run the course.
This way there is no pretending that your lab partner is a guy! Plus they are exceptionally knowledgeable and provide invaluable feedback.
The cost is variable depending on the area. $50 per hour may be average?
Lab hours: for the internal exam that depends on the number of participants, but figure at least one hour for internal assessment.
Treatment is a separate lab, not using the standardized patient (SP), then the participants would be lab partners as in most courses.
There’s additional labs for manual therapy and some neurodynamics, although in depth I do that as a separate course. (And it has internal components)
Costs are not significantly higher here in Chicago but we have exceptional access. The logistics are the thing – the course has to be well crafted and the standardized patients need to be available and the schedule needs to be followed.
We pay them directly – there is a contract.
From Tracy:
I’m already making a shift now with my educational courses I teach to Pelvic PTs and other healthcare professionals. I teach a pudendal neuralgia course and a clinical competency pelvic PT “bootcamp” course. In both of those classes, I make a big effort to try to have a male model or a male class participant available and willing to allow me to do a live demonstration on all sorts of anatomy, clinical pearls, positioning strategies, etc. Each time I do this, someone comes up and says “this was worth the price of admission” because many therapists want to learn this, but just haven’t seen the practical clinical skills to feel comfortable.
One of the big challenges I still see is that even if a PT receives some training in it, they may not see males right away after training and then seem to lose confidence again.
Next, Can you tell us about how the Section on Women’s Health is working to incorporate male pelvic health as part of the section?
From Sandy:
“The board of the SOWH is supportive of the Men’s Health Special Interest Group (SIG), which is in process of creating the structure needed to be an active SIG and is extremely supportive of the Men’s Health programming at Combined Sections Meeting.
Part of the current process of the Name Change is to address the treatment of men in pelvic health. See the update on where the SOWH is in this process and please make your voice heard: http://www.womenshealthapta.org/the-sowh-name-change-task-force-the-journey/
I am happy to have met with some of the men in the SOWH and the DPT Students (men) who are passionate about being a voice in moving forward to have more trained therapists working with Male Pelvic Health as having more male therapists involved in care. “
The professionals who teach courses through Herman and Wallace and the American Physical and Occupational Therapy association are forced to work within a model that is severely flawed. I hope that these organizations, with deeper pockets than solo providers trying to run a course, will take this into consideration and modify their courses to better meet the needs of their students and men with pelvic floor disorders.
Closing thoughts
Given these circumstances, we can understand that many physical and occupational therapistss do not feel qualified to treat men. Most of the physical and occupational therapistss working at PHRC had no prior experience with male or female pelvic floor disorders, so we trained them through reading materials, our course DVD with instructional videos, and practice on patients that we accept pro-bono: in exchange for allowing our newer therapist to practice with one of us and then we do not charge them for treatment. We know this is a luxury not available to most newer therapists, particularly the solo provider.
So what are PTs to do?
- Seek out individual preceptorships with practices that may be able to help. It cannot hurt to ask.
- Ask an experienced therapist to mentor you with one of your own male patients. In my first year of practice my mentor, Rhonda Kotarinos, came to California and treated 8 of my active patients while I observed, took notes, and asked questions. Many of those patients were men and this absolutely was the most useful learning experience in my first five years of practice.
As for the courses…
- Considering Sandy’s comments, would it be reasonable to ask male pelvic health course instructors if it is ok to bring a man to lab for practice? During lab, people are undressed but draped. With careful planning ahead this could be a reasonable solution.
- Larger organizations such as hospitals have larger budgets than solo providers like Sandy, Tracy, and ourselves, who also teach. Organizations that teach courses such as Herman and Wallace and the APTA could better support their course instructors by hiring male models.
- Given the expense of courses in terms of time, money, and energy, consider eliminating pre-requisites. To quote Sandy, one ‘shouldn’t have to go through the vagina’ to take a Men’s Health course.
As men, students, and professionals, what are your thoughts and suggestions on this situation?
Resources
Entropy Continuing Education Courses: http://entropy-physio.com/professional-courses
Pelvic Guru Courses: http://www.eventbrite.com/o/pelvic-guru-academy-and-sher-pelvic-health-and-healing-llc-4356240713
Pelvic Health and Rehabilitation Center Instructional DVD (for professionals only): https://pelvicpainrehab.com/instructional-video/
References
- Systematic Review of Acupuncture for Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Qin Z, Wu J, Zhou J, Liu Z. Medicine (Baltimore). 2016 Mar;95(11):e3095.
- J.N. Krieger, S.W. Lee, J. Jeon, P.Y. Cheah, M.L. Liong, D.E. Riley. Epidemiology of prostatitis. Int J Antimicrob Agents, 31 (Suppl 1) (2008), pp. S85–S90
- Eur Urol. 2016 Feb;69(2):286-97. doi: 10.1016/j.eururo.2015.08.061. Epub 2015 Sep 26. Contemporary Management of Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Magistro G1, Wagenlehner FM2, Grabe M3, Weidner W2, Stief CG4, Nickel JC5.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Melinda Fontaine
The physical and occupational therapistss at PHRC work as a team to help each other figure out the most efficient ways to help our patients. One way we share information is through weekly case studies, where one of our physical and occupational therapistss describes a patient’s case, why they chose to evaluate the structures they did, how the results of the evaluation lead to an assessment and treatment plan, and how the therapists carried out the treatment plan to help the patient reach their goals. This week’s blog features a case study by Melinda Fontaine, a PHRC physical and occupational therapists in our Berkeley location.
Here is what Melinda has to say:
ABOUT ROBERT
Robert, a healthy 34 year old man, started having pain in his tailbone, especially with sitting, driving, having sex, having bowel movements, and exercising. The only things he could think that might have contributed to his pain were heavy squats and abdominal workouts. He later started to have scrotal pain as well. Robert went to a doctor who did a pudendal nerve block. After the nerve block, he developed a rectal abscess at the site of the injection, which is an uncommon response to the procedure. This abscess then turned into a fistula, which is an abnormal tunnel between the anal canal and the skin. Fistulas are problematic because they can lead to serious infections. Because of this risk Robert underwent a fistulotomy, a surgical procedure to open a fistula and help it heal. This helped the fistula but his pain persisted. Robert started seeing a physical and occupational therapists, but had to stop because the drive was too long and he had tailbone pain with sitting.
ROBERT’S PHYSICAL THERAPY FINDINGS
Four years after the start of his pain, and with no relief, Robert decided to seek out pelvic floor physical and occupational therapy. He found PHRC on the web and came in for an evaluation. Since the pain started with heavy abdominal workouts, I examined the abdomen for a cause and found tight rectus abdominus muscles with trigger points. The rectus abdominus commonly refers pain to the genitals, so I confirmed that he should not be doing abdominal exercise until his rectus abdominus issues had been addressed. I looked at the muscles near the tailbone for sources of the tailbone pain and found left coccygeus trigger points externally that reproduced his tailbone pain. Also, Robert had fascial restrictions around his ischial tuberosities, or ‘sitz bones’. Because of his scrotal pain and urinary hesitancy, I also examined the muscles of the pelvic floor located near the urethra and found high tone in ischiocavernosus and bulbospongiosus. Because of their connections near the urethra, the ischiocavernosus muscles can lead to urinary hesitancy by not releasing fully and immediately. I also looked for any signs of the abscess and fistula and could not find any adherent scar tissue.
POTENTIAL CAUSES
I explained how repeated heavy squatting created coccygeus trigger points and fascial restrictions at the ischial tuberosities. This pulled on Robert’s tailbone creating pain. His pelvic floor started to become tight in response to the tailbone pain and new length-tension relationship in the posterior pelvic floor muscles because of the abdominal workouts. Robert reported that manual therapy had helped previously, which is often the case when there is a muscular issue. For Robert’s particular case, we don’t know if the pudendal nerve block helped because it immediately turned into an abscess. I concluded the scrotal pain and urinary hesitancy are results of the tight anterior pelvic floor muscles around the urethra and the rectus abdominis trigger points.
TREATMENT PLAN
The initial plan was to perform manual trigger point release to the rectus abdominus and coccygeus muscles, connective tissue manipulation around the ischial tuberosities, and myofascial release to the ischiocavernosus and bulbospongiosus muscles internally and externally for 8-12 weeks. Robert’s home program consisted of pelvic floor drops/releases and self myofascial release using a tennis ball around the coccygeus and pelvic girdle muscles. He was already doing a stretching routine of pigeon, butterfly, and cat/cow stretches, which he reported felt good, so he continued with these stretches.
Robert’s goals for physical and occupational therapy were:
- Tolerate sitting 1 hour at a time repeatedly for a full day of work
- Tolerate sitting 2.5 hours for car ride, which he does often with family
- Return to weight lifting without pain
- No pain with sex
- No pain with bowel movements
PROGRESS
At the third visit, Robert reported feeling “a lot better”. When the trigger points in his rectus abdominis were reduced, we started core strengthening. His transversus abdominis was weak, and I wanted it to work harder especially during his weightlifting, so that his pelvic floor did not have to work as hard, which can result in injury and likely the coccygeus, pain-causing trigger point. I waited until the point when the trigger points were relieved because I was concerned that he would activate his rectus abdominus during transversus abdominus exercises. People with pain/trigger points often have faulty motor recruitment patterns which can lead to further pain/dysfunction. When left uncorrected, the faulty motor patterns can result in normal movements causing abnormal stress on structures and subsequent impairments and pain. Once corrected, people can resume exercise without trouble. Next, we added light weight lifting exercises for the upper body in a seated position to ease the demand on the pelvic floor. At visit 4, he was sitting for 4 hours at work with standing breaks and the coccygeus trigger points were gone. Robert reported no pain with bowel movements and less pain after sex. He gradually increased the intensity of his workouts. On the 5th visit, he was sitting for a full work day with standing breaks. On the 9th visit, he increased exercises too much and felt a pull in his abdominal muscles. I treated the attachment of rectus abdominis at the pubic symphysis which reproduced his pain, and his pelvic floor muscles were more hypertonic that day as well in response to this incident. This eliminated his symptoms. After the 10th visit, he took a 5 hour flight. He had a little discomfort on the way there because he sat for almost the whole 5 hours. Otherwise, he reported no pain on the trip or after he returned! Robert and I were both pleased that his goals have been met. His progression followed what I expected given his initial assessment. We planned to have Robert increase his workout intensity and follow up with me in 3-4 weeks.
Now, several months later, Robert’s goals have been met and he has been discharged from physical and occupational therapy.
Take Away Messages from the PHRC team
Melinda did a great job identifying that Robert’s exercise routine may have specific implications to his abdominal wall and pelvic floor muscles. This suspicion guided her evaluation; she identified that palpation of these structures reproduced the pain Robert was experiencing. Malinda’s treatment plan was effective because she began with manual therapy to treat his impairments and supplemented the therapy with a home program. Then, she helped him identify faulty movement problems and weak muscles. She was able to help him correct these deficiencies and help return to exercise in a manner that was therapeutic versus provocative. The timing on how and when to introduce activities is important when restoring function and transitioning back into the very activities that initially caused problems. With proper rehabilitation it is possible!