Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By Wendy Powell, Postpartum Exercise Expert, Founder + CEO of MuTu System
This information relates to every woman who is having, has had, or will ever have a baby, who wants to regain full use and look of her beautiful pre-baby body (who doesn’t?). Whether she has just had a baby, has teenage children, or if she is about to give birth, she needs to know about Wendy Powell and the MuTu System. Wendy is an expert in post partum and post pregnancy exercise, and after working with thousands of women, Wendy realized how misinformed most of them were, specifically when it came to exactly how their abdominal muscles change as a result of pregnancy. Mothers who suffer from Mommy Tummy (aka pregnancy belly and a weak pelvic floor) are often misinformed. Medically endorsed MuTu System is a 12-week program with a whole-body approach to alignment and foundation core connection for natural activation. It can help help all moms, new and old, rebuild a foundation for a strong core, a healthy pelvic floor, and will get them on the road to achieving their pre-baby body. No mother will want to miss this.
Mommy Tummy Begone: tighten pregnancy muscles in 12 weeks or 12 YEARS later. Your prayers are answered!
It happened. You can’t believe it did. But it did. The evidence is there. Staring you in the face. Demanding your attention with every cute little cry and tiny little eyebrow. Yes, that one carefree night 9 months ago (well, 10 months ago) led to the birth of your beautiful new baby. You never thought you could love something so much. And then you met your little one, and your entire world changed.
And so did your body.
It’s hard to admit it, but though you are over the moon about your new bundle of joy, every time you look down at your body, you don’t recognize it anymore. And if you’re being honest, you don’t love what you see. What’s really got you down is that brand new pudgy belly you can’t seem to shake off no matter how many planks you suffer through, no matter how many green juices you drink, and no matter how many sit ups you can muster, you simply cannot get your “mommy tummy” to go back to it’s pre-baby fabulousness. Even your doctors will tell you, “That’s just how your body is, does, and feels now.” Don’t stand for mediocrity.
Wendy Powell knows your plight. A fitness expert with 2 kids of her own, specializes in post partum and post-pregnancy exercise, Wendy developed a technique called MuTu System, which has been endorsed by specialist physical and occupational therapistss and physios worldwide. It’s specifically designed to help mommies rebuild the foundations of their core and pelvic floor in just 12 weeks, so they can go on to flatten their aptly named Mummy Tummies and continue being the great moms they are.
You see, that’s just it. No one tells women how to get their entire bodies (INSIDE and out) back into fighting shape after giving birth. They are either told to just workout, or they are kindly but tersely reminded that they had a baby (thanks Captain Obvious), and that their bodies are just going to be different now.
Well that’s just not good enough! Under no circumstances do you have to go through life with a body that no longer makes you feel sexy, confident, and whole just because you decided to have children.
“I know you may be feeling disconnected from your body, guilty or self indulgent for wanting to change it, dis-empowered or dismissed by medical professionals. I know you feel like everyone else has it all worked out, and it’s only you floundering. I can tell you right now that they don’t, and you’re not. I’ve been there and I’ve worked with thousands of women around the world who all feel the same. It CAN be better than that, and you deserve A LOT better.”
But let’s deal with the main issue, the one that MuTu System addresses: diastasis recti, also known as abdominal separation, is commonly defined as the gap between the two sides of the rectus (aka your 6 pack) abdominis muscle (although this itself, is caused by the larger problem of misalignment). It happens during pregnancy to almost 100% of women! Your body has to not only rearrange your organs, but also, your muscles in order to make room for your baby. But after birth, the muscles don’t always reconnect. This leads to diastasis recti…or the “no-pack.” Research confirms that merely aspiring to “close the gap” is neither helpful nor anatomically correct. MuTu System provides the ability to connect with, restore & use the deep muscles of your core correctly…which is vital to gaining back your function and strength. Merely pulling the gap closed (like some methods suggest)…isn’t. MuTu helps moms achieve deep connection, along with the whole body, and natural movement rather than excessive or isolated “core work”.
And because of this separation, you can do plank all day long and follow it up with a thousand sit-ups and green salads, but you will never (ever) get your post baby pudge to budge. In fact, trying to strengthen the muscles in this way actually makes things worse, weakening your pelvic floor, and leading to more instances of wetting yourself after becoming a mom, an all too common, embarrassing and yet preventable situation. You have to reconnect the muscles before you can strengthen them. Period. There is no other way.
Thankfully, that’s what MuTu System does! The Mummy Tummy workout system is a complete body makeover for moms who want to lose the baby belly, improve pelvic floor function, strengthen their core and get strong, fit and truly body confident.
So what are you waiting for? Try the MuTu system today! If you have any questions about the MuTu system or if you’re unsure if it’s appropriate for you, ask your physical and occupational therapists.
Be Well,
Wendy
Wendy Powell is the creator and founder of the medically endorsed MuTu® System Programs. She has extensive coaching experience in this specialist area and has worked personally with hundreds, and ‘virtually’ with many thousands, of pregnant women and new moms around the world
FAQ
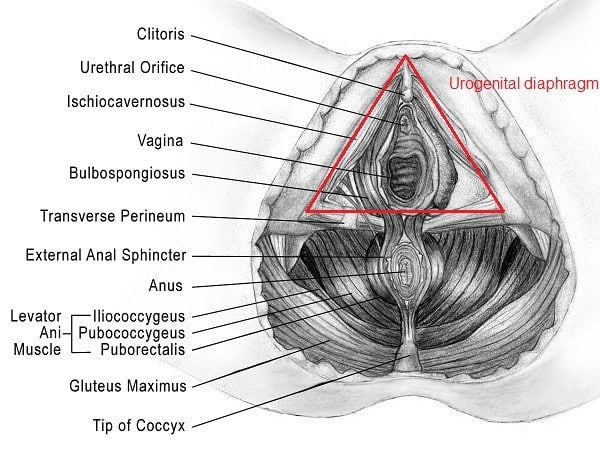
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
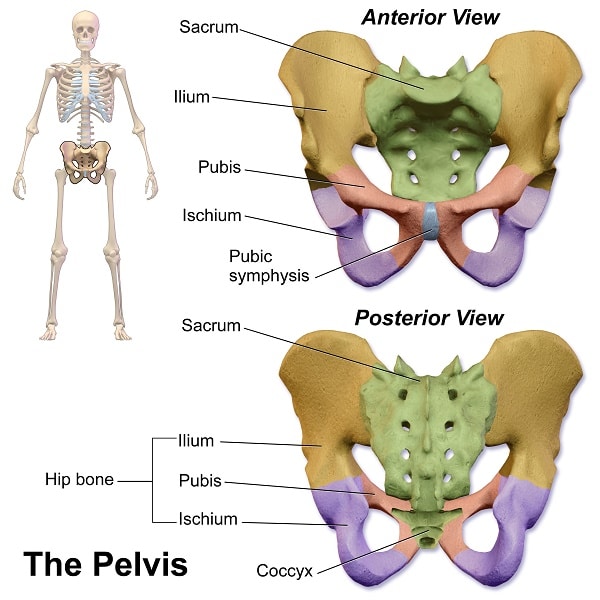
The tailbone (also known as the coccyx) is often dismissed by some as a vestige of our prehistoric ancestors. Whether or not that is true, this is a bone that we need to examine further in order to appreciate. Not only is it a major attachment site for the pelvic floor muscles, but it can also become a huge source of discomfort if injured. More often than not a patient will tell me that they hurt their tailbone and went to see a doctor, only to be given a donut cushion and sent on their way. This is not the way to effectively manage and resolve tailbone pain, but I am getting ahead of myself…
First, let’s learn the anatomy: The coccyx extends off of a large triangular bone at the base of the spinal column called the sacrum. It is made up of 3 to 5 bony segments which are connected to each other by ligaments, joint capsules, and fascia. There is a nerve that runs through the coccyx called the sacrococcygeal nerve which innervates the skin above the coccyx and sacrum. The tailbone serves as a bony attachment site for the entire deep layer of pelvic floor muscles (levator ani) and some of the superficial layer muscles (urogenital diaphragm) as well.
(Check out these blogs for a more in depth look at pelvic anatomy: male/female)
The tailbone is dynamic- as we contract our pelvic floor muscles the tailbone is flexing and extending in response. When we sit (especially when we slouch (and who doesn’t)) the tailbone becomes a weight bearing structure and when we have a bowel movement (or a more extreme scenario: give birth) the tailbone has to extend to allow evacuation through the pelvic canals (vagina and rectum).
Tailbone pain often feels dull and achy in the area between the gluteal cleft and above the anus but can also become sharp in certain situations (e.g sitting, sit to stand, lying on back). Bowel movements, penetrative sex, and orgasm can also be a source of aggravation for the tailbone. In my experience, I often find that people start having symptoms of tailbone pain but don’t seek medical attention right away because they figure that it should eventually pass…and sometimes it does. However, since the tailbone is a common attachment site for so many of our pelvic floor muscles it never really gets a break; therefore tailbone issues can develop into a persistent situation that can have a substantial effect on quality of life.
Here are some common causes of tailbone pain (coccydynia):
- A direct blow to the tailbone (i.e. fall, contact sports)
- Childbirth: during delivery, the baby’s head is positioned against the coccyx, and the pressure created during labor and pushing can result in injury to the tailbone and its surrounding structures. In rare cases, the coccyx can fracture.
- Repetitive/prolonged stress against the coccyx (i.e. cycling, rowing, prolonged sitting)
- Sometimes, the cause of coccyx pain is unknown (also known as idiopathic coccydynia)
- Less common causes of coccydynia includes bone spurs, cysts, compression of nerve roots, remote spinal injuries, local infections, and tumors. These should all be ruled out by a physician, especially if there is no clear mechanism of injury.
If you have had, or are currently experiencing, tailbone pain you can understand how troublesome it can be to deal with. It is not a part of our body that can be easily avoided and it can be difficult to access. One reason that tailbone pain can present and persist is due to pelvic girdle/sacroiliac joint bony alignment/misalignment. As we learned earlier, the tailbone forms a joint with the sacrum and becomes an attachment point for many pelvic structures. Not only can problems stemming from the sacroiliac joint give the illusion of tailbone pain, but two of our strongest pelvic ligaments (the sacrospinous and sacrotuberous ligaments) originate just above the sacrococcygeal joint (where the sacrum meets the tailbone) and can cause perceived tailbone pain when irritated.
Another reason that this symptom can become such a difficult-to-treat issue is because of relationship of the pelvic floor muscles and their physiological function. In a situation where we’ve had a direct blow to the tailbone, like a fall, there is likely a build up of inflammation in and around the bone causing a deep bruise feeling. And every time the pelvic floor muscles contract, they are tugging on the tailbone causing further irritation. This irritation then alerts the brain that there are injurious stimuli, which then cause the pelvic floor muscles to over-engage, become hypertonic, and develop trigger points. Thus, begins the vicious cycle of muscle dysfunction due to pain, a pattern that then leads to more muscle dysfunction and pain.
There are also cases in which the tailbone pain occurs either gradually or suddenly with no obvious cause. This can be due to tight pelvic floor muscles that are tight for any number of reasons: stress, previous injury, desk job, a combination of these, et cetera. It is in cases like this that the pelvic floor muscles become tight, which then pull on the tailbone and present as tailbone pain. In these cases, the tailbone is often not even painful to palpation, however if you were to palpate one of the adjacent pelvic floor muscles attaching to the coccyx (e.g. coccygeus, iliococcygeus, pubococcygeus) there is tenderness, hypertonus, and trigger points that may even directly reproduce the “tailbone” pain. This is a very common presentation that we see at PHRC.
So, I want to lay out some ideas on what to do if you are experiencing tailbone pain:
Rest: Minimize situations where you are going to be taxing the tailbone (sitting, standing for long periods, cycling). Use a cushion for sitting and try lying on your side or face down to allow plenty of blood flow to travel through the area. Here are some links to my favorite cushions:
Ice: Especially if you recently sustained a direct blow injury to the tailbone. Ice helps to constrict the blood vessels in the area and reduce inflammation. Heat is something you can also use but if it is within the first 2 weeks of injury stick with ice to flush the inflammation away from the injury site.*
Anti-inflammatories: This one you have to first discuss with your physician, but taking anti- inflammatory medication can be a huge help to interrupt the inflammatory cycle.
Roll: Use a tennis ball and roll some of the larger hip muscles-these muscles can tighten up in the presence of tailbone pain and cause further reduction of blood flow and pain. The best way to start with this is to lean back against a wall and place a tennis ball between your buttock and the wall. Gently use your bodyweight to apply pressure and roll on the tennis ball looking for sore spots. When you find a sore spot, hold and breathe until you feel a decrease in soreness intensity.
Schedule with a pelvic floor physical and occupational therapists: Because the pelvic floor muscles are so often involved with tailbone pain, it is important to schedule with a pelvic floor physical and occupational therapists sooner rather than later. Here are two previous blog posts on what to expect from a good pelvic floor physical and occupational therapy session.
**A common misconception that we hear regularly, is that the tailbone may be “out of place” or that it needs to be adjusted. It is true that tight pelvic floor muscles can have such a strong influence on the tailbone that they can actually pull it into a lateral bend, however, the root of the problem in this situation stills lies with the pelvic floor muscles. There are specific instances where the tailbone position may be affected due to a direct blow or childbirth and that is best identified through X-ray imaging. In these cases the tailbone may heal in the new position and will need to be assessed by your practitioner.
Tailbone pain is unfortunately one issue that can be mismanaged and overlooked within the medical community. However it can wreak absolute havoc on those of us having to deal with it on a daily basis. With these tips and resources you should have a better idea of where to start managing your tailbone pain in both the short and long term. This blog is here to give you hope that you can and will get better and you are not alone.
Additional resources:
International Pelvic Pain Society
American Physical and Occupational Therapy Association
*When using ice or heat be sure to set a timer and give your skin a break every 20 minutes
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual appointments!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical and occupational therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical and occupational therapistss committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. The cost for this service is $75.00 per 30 minutes. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Stephanie Prendergast
It has been an eventful few weeks in pelvic health news! We’ve summarized the top stories and included our commentary.
“Pelvic pain may be common among reproductive-age women, NIH study finds.”
From the National Institute of Health
Article summary:
- Pain reports were highest for women with endometriosis, however ⅓ of those without any pelvic condition also reported a high degree of ongoing pain or pain recurring during their menstrual cycle.
- Many women are experiencing but not reporting some form of pelvic pain.
- Gynecologists are being encouraged to ask their patients during routine visits if they are experiencing pain, as well as the type and location of pain, and offer treatment as appropriate. Similarly, women need to report pelvic pain.” Researchers suggest physicians consider asking about pain, even during routine visits. A high proportion of reproductive-age women may be experiencing pelvic pain that goes untreated, according to a study by researchers from the National Institutes of Health and the University of Utah School of Medicine, Salt Lake City.”
The majority of the people that I treat have pelvic pain. When I first saw this study, I scoffed because of the ‘duh’ factor. As I thought more about my own gynecology visits and the stories my patients tell me, I realized this seemingly oversimplified information is exactly what gynecologists and women with pelvic pain need to hear. The fact that a 2015 study from our National Institute of Health is encouraging basic communication between physicians and patients accurately reflects the poor quality of care people with persisting pain frequently encounter.
Thankfully, there has been exponential increases in research on pelvic pain and a growing number of medical professionals committed to treating it. Drs Gyang, Hartman, and Lamvu recently published an article that is a great resource for gynecologists wanting to learn more about pelvic pain. Here is the abstract:
“Musculoskeletal causes of chronic pelvic pain: what a gynecologists should know should know”
Article summary:
Ten percent of all gynecologic consultations are for chronic pelvic pain, and 20% of patients require a laparoscopy. Chronic pelvic pain affects 15% of all women annually in the United States, with medical costs and loss of productivity estimated at $2.8 billion and $15 billion per year, respectively. Chronic pelvic pain in women may have multifactorial etiology, but 22% have pain associated with musculoskeletal causes. Unfortunately, pelvic musculo- skeletal dysfunction is not routinely evaluated as a cause of pelvic pain by gynecologists. A pelvic musculoskeletal examination is simple to perform, is not time-consuming, and is one of the most important components to inves- tigate in all chronic pelvic pain patients. This article describes common musculoskeletal causes of chronic pelvic pain and explains how to perform a simple musculoskeletal examination that can be easily incorporated into the gynecologist physical examination.
Reference (Obstet Gynecol 2013;121:645–50)
Despite the recent advances, a knowledge gap exists between pelvic pain specialists, general medical providers, and patients. Societies such as the International Pelvic Pain Society, the International Society for the Study of Women’s Health, the APTA’s section on Women’s Health and The international Society for the Study of Vulvovaginal Disease are working hard to improve education and awareness, and narrow this gap, which brings us to our next news worthy item of the week.
The International Consensus Conference on Vulvodynia Nomenclature
In April, Dr. Andrew Goldstein organized a “Vulvar Pain Think Tank” with the mission of redefining and improving the 2003 definition of vulvar pain. Since 2003, studies have been conducted on possible causative factors and treatment options for women with vulvar pain. Expert researchers and clinicians were gathered and charged with the task of improving the nomenclature based on the evidence. Representatives from IPPS, ISSVD, ISSWSH, NVA and ACOG reached a consensus by the end of the meeting.
The next step was to get the new nomenclature approved by the ISSVD, IPPS, and NVA. Slight modifications were made to our initial proposal. We are extremely pleased to announce that as of this week, all three societies UNANIMOUSLY approved our new definition and categorization of vulvar pain! As a group we believe this is an important advancement for the diagnosis and management of persistent vulvar pain.
On a personal note, this conference was an intimidating but extremely stimulating event in my professional career. I am honored to have been apart of it. If you would like to read more about it check out my blog post titled “What is Vulvodynia?”.
Vulvar pain interferes with a woman’s sex life, and so does a lack of sexual desire, which brings us to the next newsworthy item of the week.
US Food and Drug Administration approves The Little Pink Pill
Similar to pelvic pain, female sexual dysfunction is under-reported by woman, misunderstood by medical professionals, and is associated with embarrassment and quality of life issues. Last week, the US Food and Drug Administration approved the first drug authorized to treat female hypodesire disorder, flibersarin. The approval of this drug is causing an uproar between its supporters and antagonists.
Why?
- Early on, the media inaccurately called this drug “Female Viagra”. It’s not. Drugs such as sildenafil (Viagra) have a transient effect on enzymes that allow erection by causing smooth muscle relaxation when sexually stimulated. It is taken before suspected sexual contact. Flibersarin works on neurotransmitters in the brain and needs to be taken daily. It works on the same neurotansmitters that are associated with anxiety and depression.
- A second battle is the ‘ gender discrimination’ vs Big Pharma controversy. Currently there are 27 medications on the market for erectile dysfunction and until now, there have been zero for female sexual dysfunction. Opponents suggest the creators of flibersarin invented ‘female sexual dysfunction’ as a money making disorder and that it does not really exist. Similar to pelvic pain, many general medical professionals are not aware of how to diagnose or treat the disorder. Women get told things like “it’s all in your head” or “drink a glass of wine”. Other opponents recognize female sexual dysfunction as a disorder but question the efficacy of the drug as treatment. Supporters attack both groups of opponents on the basis of not supporting women. It is important to recognize that sexually savvy medical professionals may not support the drug because of science, not anti-feminism.
- The drug was tested on 28 men and 2 women. Side effects include a severe drop in blood pressure that exponentially increases with alcohol use. I am not sure why a drug that is only for women was tested mostly on men. Aside from that minor issue, women taking the medication cannot have even one drink, ever, if they would like to remain conscious.
I am an advocate for women suffering from sexual dysfunction, whether it is caused by pelvic pain or a desire disorder. Both pelvic pain and hypodesire disorder are misunderstood, underreported multifactorial syndromes involving both physiological and emotional components. As medical professionals it is important to differentially diagnose the sources of each person’s disorder and customize an appropriate treatment plan for that particular person. It is as short-sighted to believe a ‘pink pill’ is effective for all women suffering from desire disorders as it is to believe a single pill can cure vulvar pain.
The bottom line is women need to report their pelvic pain, their providers need to ask about it and either treat them or help them find someone who can. If you are looking to find a provider that specializes in pelvic pain, please see this blog post to help you find someone in your area that can help.
“Thank-you and Good Night”.
Stephanie Prendergast, MPT

FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.