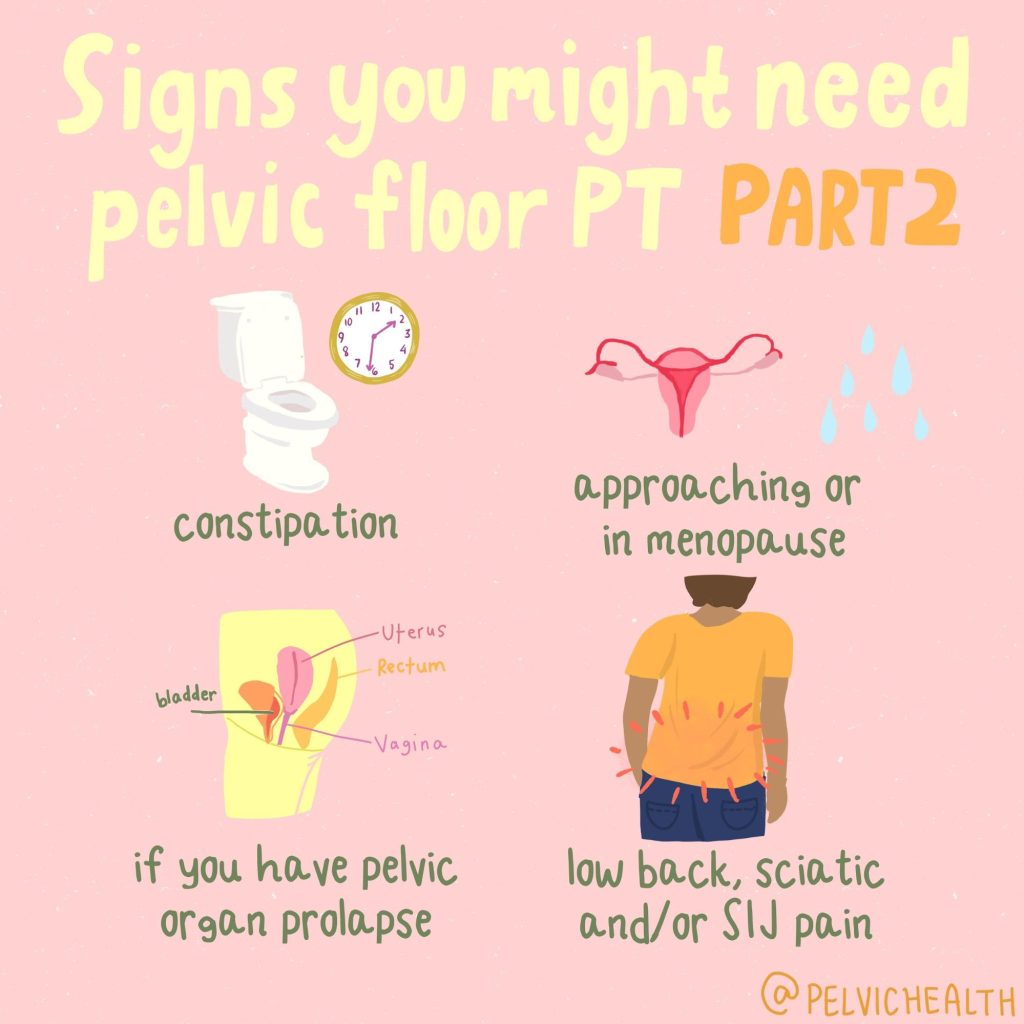
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
One Big Beautiful Bill Act: The Impact on Pelvic Health Physical and Occupational Therapy
By Stephanie Prendergast, MPT, PHRC Pasadena
In July 2025, the One Big Beautiful Bill Act (OBBBA) was signed into law, introducing transformative student-loan reform that will shape federal graduate borrowing for decades to come. Among its many sweeping policy changes, one stands out for the rehabilitation community: a recalibration – and dramatic narrowing – of what counts as a “professional degree” for the purpose of federal student loans. The ripple effects for physical and occupational therapists, Medicare beneficiaries, and the broader U.S. health-care system are profound.
For providers working in specialized, high-needs areas such as pelvic health rehabilitation – clinically managing conditions like urinary incontinence, sexual pain disorders, and bowel dysfunction – the implications feel deeply personal. But beyond personal frustration lies a structural reckoning. This law risks destabilizing our clinical pipeline, restricting educational access, and ultimately reducing care availability for the patients who need us most.
The Legislative Change – and who it leaves behind
The OBBBA eliminates Grad PLUS, replacing it with a bifurcated definition of post-baccalaureate borrowing:
- Students enrolled in designated “professional degree programs” may receive up to $50,000 annually, with a $200,000 lifetime cap.
- Students in all other graduate programs – classified under new policy as “non-professional degree programs” – are capped at $20,500 annually, with a $100,000 lifetime borrowing limit, representing an effective reduction of roughly 50% compared to prior borrowing norms.
The list of approved “professional degree programs” remains largely unchanged from legacy policy definitions, emphasizing physician and select medical specialties including: physicians, pharmacists, and attorneys.
Notably excluded from this designation, and therefore reclassified as “non-professional degrees”, are: physical and occupational therapists, nurse practitioners, physician’s assistants, certain mental health professionals, and speech-language and audiology doctorates.
This reclassification was confirmed in recent rulemaking commentary, which explicitly noted that rehabilitation professions and graduate therapy degrees are no longer eligible for the professional borrowing limits afforded to medical degrees.
The real-world cost of a semantic downgrade
Language drives policy. Policy drives financing. And financing drives workforce behavior.
Physical and occupational therapists follow a training pathway that rivals many degree tracks deemed “professional” under the new rule. The process includes:
- Four years of undergraduate education
- Three years of clinical doctorate graduate training, including full-time clinical clerkships
- Passing difficult federal and state licensing boards
- Maintaining licensure with required continuing education hours and mandatory clinical competencies
And for those committed to pelvic health rehabilitation – a specialty serving patients with severe, complex, often disabling symptoms – the financial burden climbs even higher. Post-graduate pelvic-health training programs often cost thousands to tens of thousands of dollars, typically paid out-of-pocket, including advanced fellowships, certifications, and residencies.
Impact on pelvic health patients
The pelvic health patient population is often in dire need. Therapists in this area commonly treat conditions such as:
- Pelvic Floor Dysfunction
- Diagnoses such as Endometriosis, Vulvodynia, Vestibulodynia, Interstitial Cystitis, Chronic Pelvic Pain Syndrome, Pudendal Neuralgia
- Neuroplastic pain syndromes
- Urinary and fecal incontinence
Interdisciplinary pelvic pain requiring both rehab and medical management.
Crucially, evidence consistently shows that medical management alone is rarely sufficient for treating chronic pelvic pain and dysfunction – a fact that underscores the need for interdisciplinary rehabilitation. Pelvic-health therapists do not “replace” medicine – we partner with it, addressing neuromuscular impairments, functional disability, tissue sensitivity, behavioral pain-science education, and return-to-life outcomes that pharmaceuticals alone cannot restore.
If therapist numbers decline, so does the patient’s ability to achieve continence, sexual function, and pain reduction, all of which directly influence psychosocial participation, mobility independence, sleep, emotional health, and societal productivity.
Medicare: coverage vs capacity vs reality
The OBBBA does not directly amend Medicare coverage rules for therapy – but its indirect impact on the coverage landscape may be even more powerful.
Therapy reimbursement under Medicare is governed largely by:
- The Centers for Medicare & Medicaid Services
- Budget-neutrality requirements
- Therapy caps historically imposed and intermittently removed
- Relative Value Unit (RVU) classifications that often undervalue rehabilitative care
Even before OBBBA, rehab providers have weathered perennial reimbursement erosion despite rising overhead costs – supplies, clinic leases, documentation compliance systems, liability insurance, and salary competitiveness.
If clinician supply drops, payors are likely to see PT and OT services as less central – more discretionary, further compromising future payment schedules for therapy, just as we see rising barriers for care access in underserved populations including rural communities, Medicaid beneficiaries, and disabled Medicare recipients.
Already, non-physician graduate providers such as nursing and rehab professions have voiced national opposition, warning that the policy threatens clinician access, patient care access, and educational affordability.
Provider frustration and burnout: a documented crisis
Working in health care is a constant battle. Rehab providers face:
- High student-loan burden
- Salaries that often fail to keep pace with inflation
- Declining reimbursement rates
- High documentation burden for insurance compliance
- Specialty training costs largely out-of-pocket
- Longer patient waitlists with fewer clinicians
- Rising provider burnout across allied health
Meanwhile, private insurance stakeholders continue posting record profits. For example:
- UnitedHealth Group
- Humana Inc.
Insurance profits have rarely correlated with rehab care sustainability – and the result is visible: burned-out clinicians and suffering patients with less access to skilled providers.
National journalism has already warned of clinician outrage and pipeline risk, particularly for professions excluded under the new borrowing rules like nursing and rehabilitation.
When patients pay the price for policy abstraction
If nothing changes, federal policy could fuel cascading harm:
- Fewer students able to afford PT/OT doctorate programs
- Fewer clinicians able to afford pelvic-health specialization
- Longer wait times
- Clinic closures or capacity reductions
- Fewer interdisciplinary partners for pelvic pain care
- Lower reimbursement justification due to workforce scarcity
- Patients left untreated – or under-treated
This means that patients suffering pelvic pain or dysfunction might wait months to be evaluated, lose access to conservative care options entirely, or be returned to a solely medical path that is statistically less sufficient for functional restoration.
The call to action
This is a moment for advocacy – not passive acceptance.
Professional associations including the American allied-health coalition have already mobilized opposition, warning that programs like DPT and OTD are essential, intensive, and must be recognized as professional-level training tracks to preserve our workforce pipeline and patient access to care.
If the rulemaking definition can be updated to reflect modern educational rigor and clinical necessity, the damage could still be mitigated. But if nothing changes, we risk losing the next generation of pelvic-health therapists – and our patients will suffer most.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Stephanie Prendergast, MPT, PHRC Pasadena
Many people think of Restless Leg Syndrome (RLS) as a sleep-related leg problem ; the irresistible need to move, the creeping sensations, the nights spent pacing instead of resting. But growing research and clinical observation suggest something much broader: RLS may be part of a whole-body sensory and motor dysregulation, with ties to bladder symptoms and pelvic floor dysfunction, including a number of pelvic pain syndromes.
At the Pelvic Health and Rehabilitation Center (PHRC), we’ve seen this overlap firsthand. Patients with persistent pelvic tension or ‘tightness’, urinary urgency and/or frequency, irritative bladder symptoms, or genital discomfort sometimes describe “restless” sensations not just in their legs, but deep in their pelvic structures. Understanding these links helps us design more comprehensive treatment plans that address both the pelvic floor and the nervous system that governs it.
Understanding Restless Leg Syndrome in Context
As outlined in our previous post, RLS is a neurological condition characterized by an urge to move the legs, especially at night or during rest. It’s thought to arise from dopaminergic dysregulation and iron deficiency in the brain, both of which disrupt smooth motor control and sensory processing.
Beyond the legs, the condition reflects a sensory hypersensitivity ; the nervous system becomes overly reactive to otherwise normal sensations. This helps explain why some individuals also experience “restless” or uncomfortable sensations in other regions, including the pelvic and genital area.
Restless Genital Syndrome: A Clue from the Pelvis
A condition called Restless Genital Syndrome (RGS), first described in the early 2000s, presents with sensations of tingling, pressure, or internal agitation in the genital or pelvic region. Importantly, these sensations are not linked to sexual arousal and often worsen at rest, just like RLS.
Neurophysiological studies have shown that some people with RGS also meet criteria for RLS, and both conditions often respond to dopaminergic medications (like pramipexole). This overlap suggests they share a common mechanism ; likely involving the lumbosacral nerves that control both the legs and the pelvic floor.
At PHRC, we think of RGS as part of a continuum of sensory-motor dysregulation. The same central nervous system patterns that drive restless legs ; dopamine imbalance, sensory hyperexcitability, and altered movement feedback ; can easily extend into the pelvic region.
Shared Pathways: The Neurology of RLS and the Pelvic Floor
The pelvic floor is more than a group of muscles; it’s a hub of sensory and motor information, richly connected through the sacral spinal cord and the pudendal nerve. These nerves share close connections with the pathways implicated in RLS.
Here’s how the two systems intersect:
- Shared nerve roots: The lower spinal cord (L2–S3) sends fibers to both the legs and pelvic organs. When these circuits become dysregulated, sensory symptoms may appear in either or both regions.
- Autonomic involvement: RLS is linked to changes in autonomic nervous system activity (fight-or-flight vs. rest-and-digest). Pelvic floor tone is also heavily influenced by autonomic balance ; many people with chronic stress or poor sleep develop hypertonic pelvic floor muscles.
- Neuroinflammation and iron metabolism: Iron deficiency, microglial activation, and dopamine dysregulation seen in RLS may also affect pelvic nerves, influencing pain perception and muscle tone.
- Movement and muscle co-contraction: Just as RLS causes involuntary leg movements, some people experience unconscious pelvic floor tightening during episodes of restlessness or nocturnal movement.
In other words, the restlessness of RLS may extend into the pelvis, resulting in pelvic floor overactivity, urinary urgency, or genital discomfort.
Bladder and Bowel Clues
Several studies have explored the connection between RLS and overactive bladder (OAB). Patients with RLS often report more urinary urgency, frequency, and nocturia (waking to urinate at night). One hypothesis is that both RLS and OAB stem from hyper-responsive sensory circuits in the spinal cord and brainstem.
Similarly, chronic constipation ; common in both pelvic floor dysfunction and RLS ; can worsen sensory feedback loops, leading to further pelvic tension. At PHRC, we see how unaddressed bowel dysfunction perpetuates pelvic and lower limb discomfort.
These observations reinforce the need to look beyond single symptoms. A patient’s nighttime restlessness, urinary urgency, or pelvic pain may all share a nervous-system origin.
The Female Connection
RLS is twice as common in those assigned female at birth, particularly during pregnancy and menopause ; life stages characterized by hormonal shifts that influence both the nervous system and pelvic tissues. Estrogen and progesterone fluctuations can alter dopamine sensitivity, while pregnancy increases venous congestion and iron demands. These same changes can trigger or worsen pelvic floor dysfunction, pelvic pain, or bladder symptoms.
Recognizing these overlapping hormonal and neurovascular influences is critical for accurate diagnosis and individualized care.
How Pelvic Floor Physical and Occupational Therapy Can Help
Even though RLS is a neurological condition, pelvic floor physical and occupational therapy can play a valuable role, especially when pelvic symptoms coexist. Here’s how:
- Muscle down-training and relaxation: Manual therapy, biofeedback, and breathing techniques help calm hypertonic muscles that may tighten reflexively during RLS episodes.
- Nerve mobilization: Gentle neural gliding and positional release techniques support the pudendal and sciatic nerves, improving blood flow and decreasing neural tension.
- Circulatory enhancement: Movement, stretching, and soft tissue work improve lower-body and pelvic circulation, which may reduce discomfort from venous congestion.
- Autonomic regulation: Incorporating mindfulness, diaphragmatic breathing, and body-scan exercises helps reduce sympathetic overactivity ; the same system that amplifies both pelvic tension and RLS restlessness.
- Interdisciplinary care: Collaboration with physicians is essential to address systemic contributors such as iron deficiency, sleep deprivation, or dopaminergic imbalance.
When treatment combines neurologic management and pelvic rehabilitation, patients often notice better sleep, less pelvic tension, and improved quality of life.
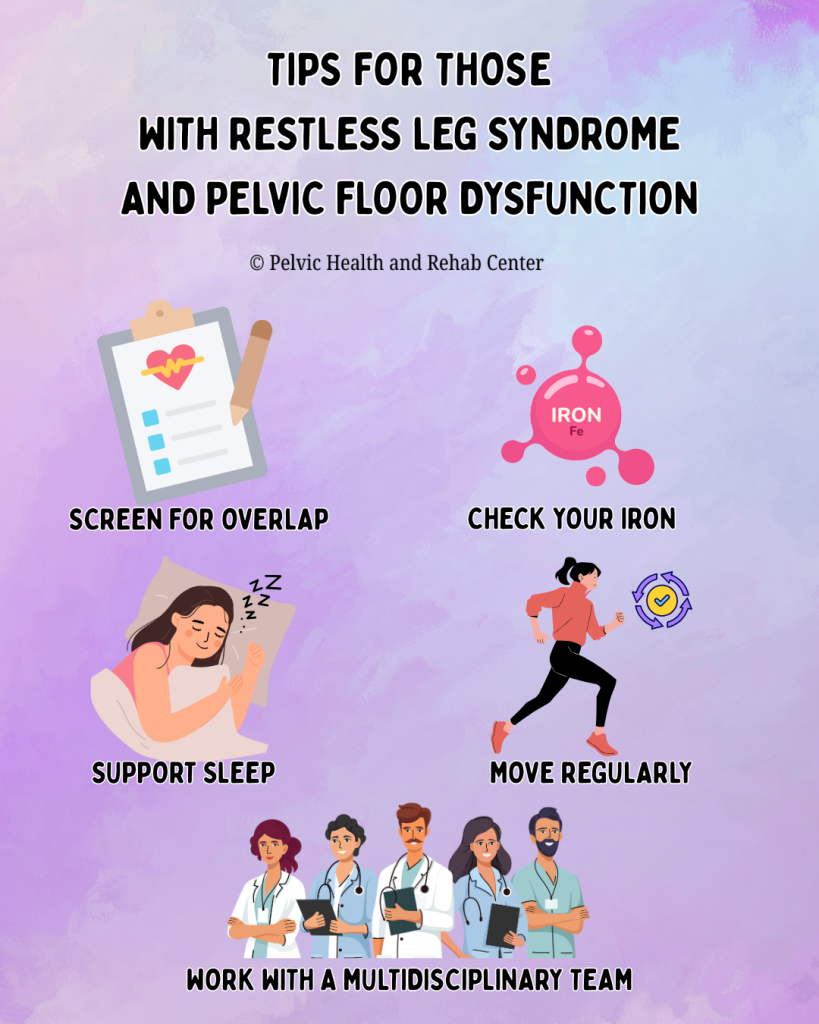
Practical Tips for Those With Restless Leg Syndrome and Pelvic Floor Dysfunction
Screen for overlap: If you have pelvic pain or urinary urgency plus nighttime leg restlessness, tell your provider. Both may stem from one nervous-system imbalance.
Check your iron: Ferritin levels below 75 µg/L are linked with RLS; optimizing iron can help both leg and pelvic symptoms.
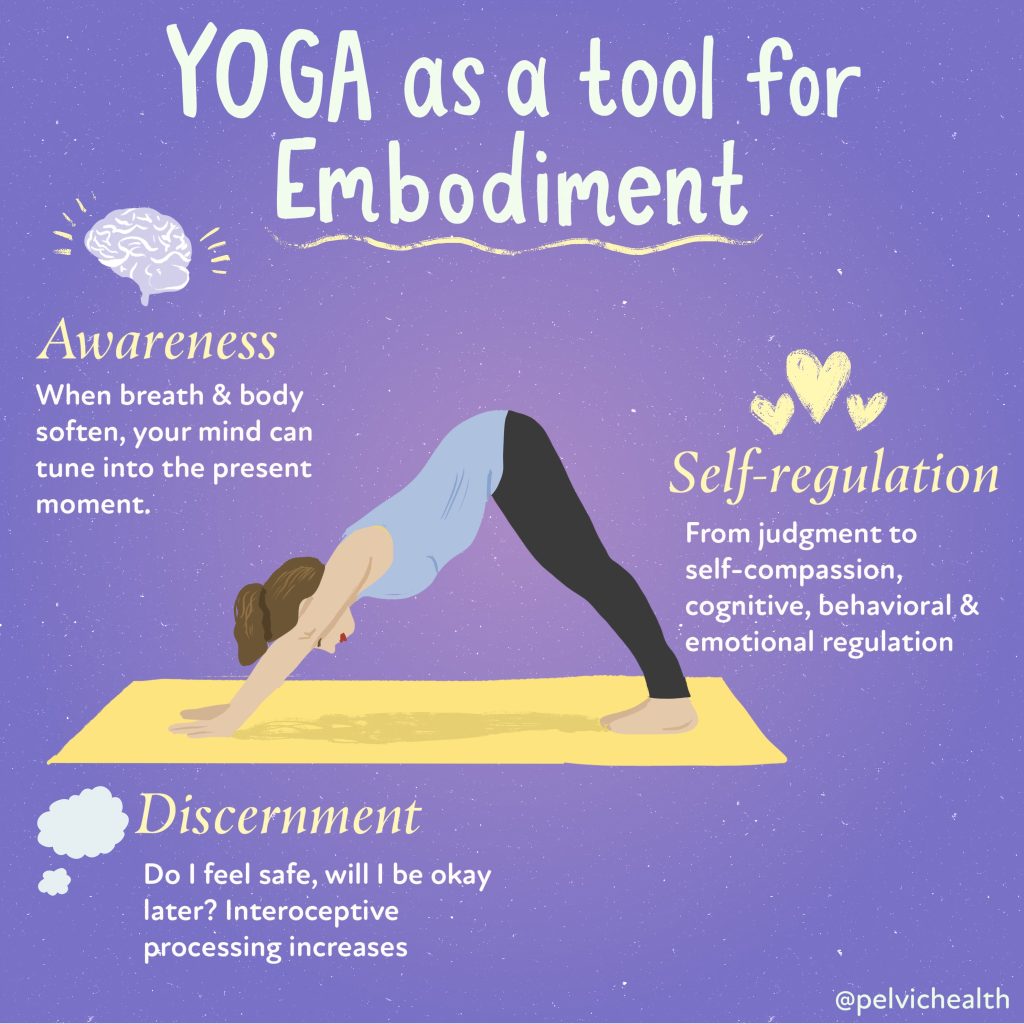
Move regularly: Gentle evening stretches, walking, or yoga reduce both leg and pelvic tightness.
Support sleep: Consistent bedtime routines, magnesium intake (if appropriate), and stress reduction lower symptom intensity.
Work with a multidisciplinary team: A pelvic health physical therapist, primary care physician, and possibly a neurologist can coordinate a plan that addresses all levels ; muscular, vascular, and neural.
The Takeaway
Restless Leg Syndrome is more than a “leg problem.” It’s a systemic sensory-motor dysregulation that can influence the pelvic floor, bladder, and even sexual function. For some, the pelvis becomes part of the “restlessness loop” ; muscles tighten, nerves fire excessively, and the nervous system can’t find calm.
The good news: once recognized, these connections can be treated. Through integrated care ; neurologic, musculoskeletal, and behavioral ; patients can regain rest, comfort, and control over both their legs and their pelvic health.
At PHRC, we treat the body as an interconnected system. Whether your symptoms start in the legs, pelvis, or both, our goal is to restore balance, reduce tension, and help you feel at home in your body again.
References
Malykhina, A. P. (2007). Neural mechanisms of pelvic organ cross‑sensitization. Neuroscience, 149(3), 660–672. https://pubmed.ncbi.nlm.nih.gov/17920206/
Malykhina, A. P., Sengupta, J. N., et al. (2005). Mechanisms of pelvic organ cross-talk: Impact of colorectal distention on bladder afferent nerve activity. American Journal of Physiology – Regulatory, Integrative and Comparative Physiology, 288(3), R555–R564. https://pubmed.ncbi.nlm.nih.gov/23542407/
Panicker, J. N., Marcelissen, T., von Gontard, A., Vrijens, D., Abrams, P., & Wyndaele, M. (2018). Bladder-bowel interactions: Do we understand pelvic organ cross‑sensitization? International Consultation on Incontinence Research Society. https://pubmed.ncbi.nlm.nih.gov/31821639/
Quaghebeur, J., et al. (2024). Integral theory and pathogenesis of LUTS and chronic pelvic pain. Pelviperineology, 43(1), 30‑39. https://pelviperineology.org/pdf/07d42497-fb2b-47e0-be2f-8805fa940376/articles/PPj.2024.43.01.2023-11-3/Pelviperineology-43-30-En.pdf
Ustinova, E. E., Fraser, M. O., & Pezzone, M. A. (2010). Cross-talk and sensitization of bladder afferent nerves. Neurourology and Urodynamics, 29(1), 77–81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805190/
Vlasie, A., Trifu, S. C., Lupuleac, C., & Cristea, M. B. (2021). Restless legs syndrome: An overview of pathophysiology, comorbidities and therapeutic approaches. Experimental and Therapeutic Medicine, 22(6), 1355. https://www.spandidos-publications.com/10.3892/etm.2021.11108
Moral, C., Aydın, M., Yılmaz, A., İrkılata, L., Bitkin, A., & Kırdağ, M. K. (2025). The relationship between restless legs syndrome and overactive bladder: A cross‑sectional, controlled study. International Journal of Urology. https://pubmed.ncbi.nlm.nih.gov/40045817/
American Academy of Sleep Medicine. (2024). Treatment of restless legs syndrome and periodic limb movement disorder: Clinical practice guideline. https://aasm.org/wp-content/uploads/2024/03/Treatment-of-RLS-and-PLMD-CPG.pdf
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Stephanie Prendergast, MPT, PHRC Pasadena
Have you ever felt an uncontrollable urge to move your legs when you’re trying to relax or fall asleep? If so, you may have experienced symptoms of Restless Legs Syndrome (RLS). This neurological condition affects millions of people, often disrupting sleep, causing distress, and sometimes connecting with other health issues, including pelvic floor dysfunction.
Understanding the Basics
Restless Legs Syndrome is a sensorimotor disorder, meaning it involves both the nervous system and movement. People with RLS describe sensations deep within their legs, sometimes in the calves, thighs, or feet; that create an irresistible need to move. These sensations are often described as:
- Tingling, crawling, itching, or “electric” feelings
- Deep ache or pressure inside the legs
- Restlessness that’s worse during periods of inactivity (sitting, lying down, or in the evening)
- Relief only when moving—walking, stretching, or massaging the legs
The hallmark feature is that symptoms are worse at night and improve with movement. This cycle often leads to difficulty falling asleep or staying asleep, contributing to fatigue, irritability, and reduced quality of life.
Who Gets Restless Legs Syndrome?
RLS can affect anyone, but certain factors increase risk:
- Genetics: Up to half of cases run in families.
- Sex: Women are affected nearly twice as often as men.
- Age: Symptoms often worsen with age, though they can appear at any time.
- Pregnancy: Many pregnant women experience temporary RLS, especially in the third trimester.
- Medical conditions: Iron deficiency, diabetes, peripheral neuropathy, kidney disease, and certain neurological disorders are associated with higher rates of RLS.
- Medications: Some antidepressants, antihistamines, and dopamine antagonists can worsen symptoms.
- Lifestyle factors: Caffeine, nicotine, and alcohol may intensify restlessness.
Why Does It Happen?
Although the exact cause is still being researched, studies point toward dopamine dysregulation and iron metabolism in the brain. Dopamine is a neurotransmitter that helps control movement; low dopamine levels in specific brain regions may trigger the uncomfortable sensations and motor restlessness typical of RLS.
Iron plays a role because it’s essential for dopamine synthesis. Even if blood tests show “normal” iron, the brain may not have enough iron stores for proper signaling. This is why iron supplementation (guided by a physician) can be an effective part of treatment for some individuals.
Other mechanisms under investigation include neuroinflammation, peripheral nerve hypersensitivity, vascular dysfunction, and autonomic nervous system dysregulation — all of which are also relevant in chronic pain and pelvic floor dysfunction.
Restless Legs Syndrome and Sleep
Sleep disturbance is one of the most common and frustrating consequences of RLS. People often toss and turn, unable to get comfortable. Many also experience periodic limb movements during sleep (PLMS) — involuntary leg jerks or twitches that occur repeatedly and disrupt rest. Over time, this can lead to chronic sleep deprivation, mood changes, and decreased concentration.
Improving sleep hygiene—consistent bedtime, stretching before bed, reducing screen time, avoiding caffeine late in the day—can reduce symptoms and improve rest.
Possible Connection to Pelvic Floor Dysfunction
While RLS primarily affects the legs, research and clinical observations suggest possible overlap with pelvic symptoms. Conditions like overactive bladder, pelvic pain, and restless genital syndrome have been found in some patients with RLS. These links point to shared neurological and sensory pathways that influence both the legs and the pelvic region.
For example:
- The spinal and peripheral nerves that regulate leg movement also communicate with pelvic floor and bladder control centers.
- Autonomic dysregulation (how the nervous system balances “fight or flight” vs “rest and digest”) can affect both sleep and pelvic muscle tone.
- Some patients describe “restlessness” or deep discomfort not only in their legs but also in the pelvic or genital region—a condition termed restless genital syndrome (RGS), thought to be a variant of RLS.
At PHRC, we see patients whose pelvic pain, urgency, or genital discomfort are intertwined with broader nervous system hypersensitivity or RLS-like features. Recognizing this overlap allows for more comprehensive, whole-body management that includes both the pelvic floor and nervous system regulation.
Diagnosis
Diagnosis is made clinically based on a patient’s history and symptom pattern. There’s no definitive blood test or imaging scan, but your clinician may check:
- Iron studies (especially ferritin levels)
- Kidney function
- Nerve health (if neuropathy is suspected)
- Sleep quality or periodic limb movements
A thorough history is essential, especially to rule out other conditions that can mimic RLS (such as leg cramps, arthritis, or neuropathy).
Treatment Options
Treatment depends on symptom severity, frequency, and underlying causes.
Lifestyle and behavioral changes:
- Regular moderate exercise and stretching
- Good sleep hygiene
- Reducing caffeine, nicotine, and alcohol
- Massage, warm baths, or heat before bed
Medical therapies:
- Iron supplementation (if ferritin <75 µg/L)
- Dopamine agonists (e.g., pramipexole, ropinirole)
- Alpha-2-delta ligands (e.g., gabapentin, pregabalin)
- In refractory cases, other medications under medical supervision
Integrative approaches:
- Yoga, mindfulness, and breathing exercises to regulate the nervous system
- Physical and Occupational therapy to address lower-limb tension, circulation, and body alignment
- For those with overlapping pelvic floor dysfunction, targeted pelvic rehabilitation may improve muscle balance and relieve secondary discomfort
Living Well with Restless Legs Syndrome
Restless Legs Syndrome is real, and for many, it’s disruptive—but it’s also manageable. Understanding the triggers, treating underlying causes like iron deficiency, and supporting your nervous system through movement, stress management, and healthy sleep routines can dramatically improve symptoms.
If you or someone you know experiences RLS-like sensations, discuss it with your healthcare provider. Identifying it early helps avoid unnecessary distress and opens the door to effective, personalized treatment.
At PHRC, we believe the body’s systems are deeply interconnected—what affects your legs, nerves, and sleep can influence your pelvic health, and vice versa. Recognizing those links helps us treat the whole person, not just isolated symptoms.
Stay tuned to the blog, next week we will do a deeper dive into the connections between restless Leg Syndrome and pelvic floor disorders.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!