Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
Pudendal neuralgia is an often misunderstood and misdiagnosed source of chronic pain. Additionally, this condition doesn’t just cause pain; it can affect how you sit, move, and live your life.
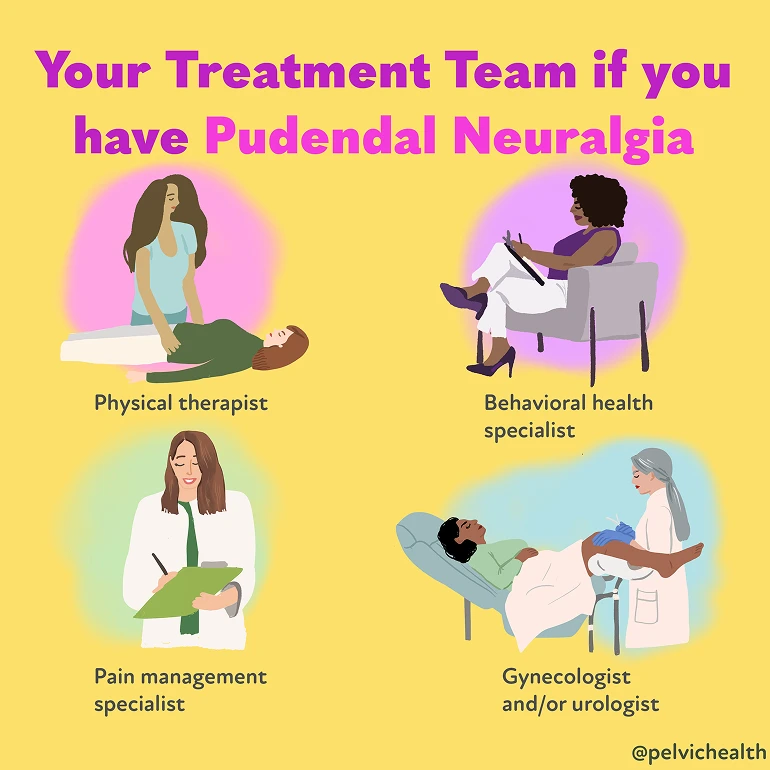
At the Pelvic Health and Rehabilitation Center (PHRC), we specialize in treating pudendal neuralgia. PHRC cofounders Elizabeth Akincilar and Stephanie Prendergast specialized in this condition in the early 2000’s. They recognized the need for medical professionals to undergo training to diagnose and treat pudendal neuralgia and developed the first continuing education course for medical professionals on this topic in 2007. They taught the course over 40 times around the world and regularly lecture about pudendal neuralgia at medical and physical and occupational therapy conferences.
As pelvic floor physical and occupational therapists, we work closely with individuals who have spent years searching for answers, often seeing multiple providers before receiving an accurate diagnosis. There is simply a shortage of medical doctors and pelvic floor physical and occupational therapists qualified to treat this diagnosis. Through a combination of expertise, evidence-based care, interdisciplinary management with trusted colleagues, and a deep understanding of the pelvic nervous and musculoskeletal system, we help clients find relief, regain function, and feel like themselves again.
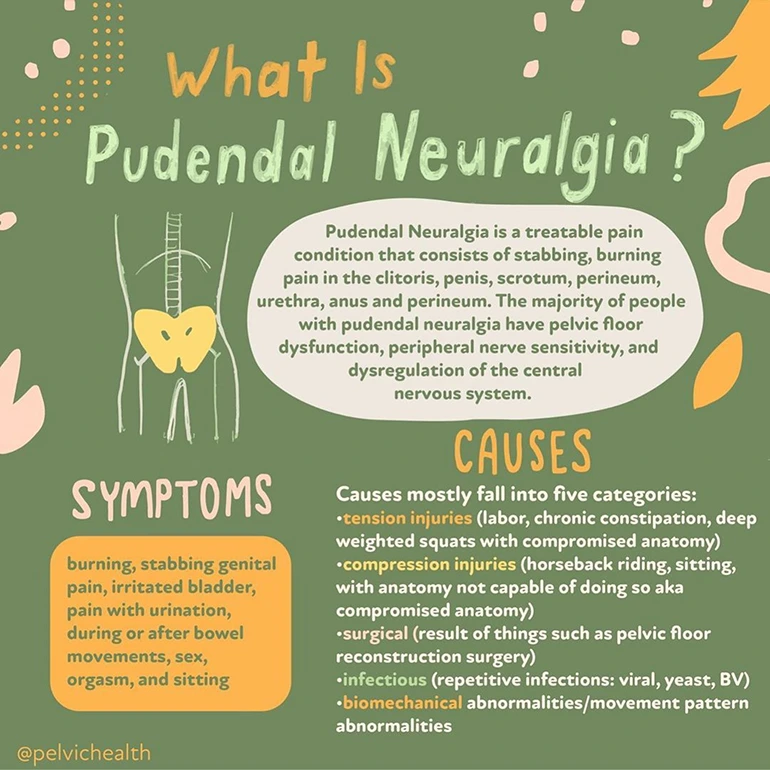
What is Pudendal Neuralgia?
Pudendal neuralgia is a common condition that causes pelvic pain. When this nerve becomes inflamed or entrapped, it can lead to burning, stabbing, or aching pain in the pelvic region, often worsened by sitting. It can lead to issues with urination, bowel movements, and sexual function.
The term ‘neuralgia’ means neuropathic pain in the distribution of a nerve. The pudendal nerve originates from sacral nerve roots two, three, and four and takes a complex route through the pelvis. This route includes the pelvic floor muscles, sacrotuberous and sacrospinous ligaments, and Alcock’s Canal. Along its path, the nerve splits into branches, making sharp angles and turns, which increases its risk of injury/compromise.
The pudendal nerve’s sensory coverage includes the vulva (clitoris, labia major/minora, vestibule), the penis and scrotum, the last third of the urethra and rectum, the anal and urinary sphincters, the perineum, and pelvic floor muscles. It is a very unique mixed nerve (it contains sensory, motor, and autonomic fibers). These components allow it to provide feeling, muscle movement, and voluntary and involuntary control of urinary, bowel, sexual function, and muscle activation.
Although pudendal neuralgia is considered rare, with some sources estimating it affects about 1 in 100,000 people, that number might not reflect the true prevalence. Many individuals go undiagnosed or misdiagnosed for years, often because few healthcare providers are familiar with the condition or how to properly assess the pudendal nerve.
At PHRC, we regularly see clients who have spent months or even years seeking answers for their pain. Pudendal neuralgia doesn’t appear clearly on imaging or standard tests, which makes a detailed clinical evaluation essential. That’s where pelvic floor physical and occupational therapists come in. Pelvic floor physical and occupational therapy is a key component of recovery, offering strategies to reduce pressure on the nerve, calm the nervous system, and improve mobility and function over time.
What are the Symptoms of Pudendal Neuralgia?
Symptoms of pudendal neuralgia include:
- Burning, shooting, stabbing pain in the genitals, perineum, or anus
- Urinary urgency, frequency, burning before, during, or after urination
- Pain before, during, or after bowel movements
- Pain before, during, or after sexual activity and orgasm
- Symptoms are worse when sitting versus standing or lying down
- Symptoms can be provoked by trunk flexion, hip flexion, external rotation of the hip, and certain exercises/activities such as squats, lunges, walking uphill, and sitting
Multiple nerves innervate the pelvic region, including the following. The symptoms of pudendal neuralgia (including burning, shooting, or stabbing pain) can occur in some or all of the structures the involved nerve supplies sensation to.
- Ilioinguinal Nerve
- Genitofemoral Nerve
- Illiohypogastric Nerve
- Posterior Femoral Cutaneous Nerve
- Sciatic Nerve
- Obturator Nerve
- Pudendal Nerve
What Causes Pudendal Neuralgia?
Symptoms of neuralgia occur when the nerve is compromised in a manner that interrupts its ability to slide, glide, and move normally. Common causes of pelvic neuralgias include:
- Surgical scars from hernia repairs, cesarean section, and laparoscopic abdominal and pelvic surgeries
- External trauma, such as car accidents or falls
- Musculoskeletal and joint dysfunction
- Hernias
The pudendal nerve has a more complicated course than other pelvic nerves, making it more prone to injury. The aponeurosis (a flat, strong layer of connective tissue) of the obturator internus muscles forms a fascial canal (a tunnel made of connective tissue) called Alcock’s Canal, which houses a main branch of the pudendal nerve. Common causes of pudendal neuralgia include:
- Obturator Internus, Piriformis, and/or pelvic floor dysfunction
- Altered lumbo-pelvic-hip mechanics
- Compression issues (sitting, cycling, horseback riding)
- Tension issues (constipation, childbirth, heavy weight lifting involving squats/lunges)
- Surgical insult (pelvic organ prolapse repair, prostatectomy)
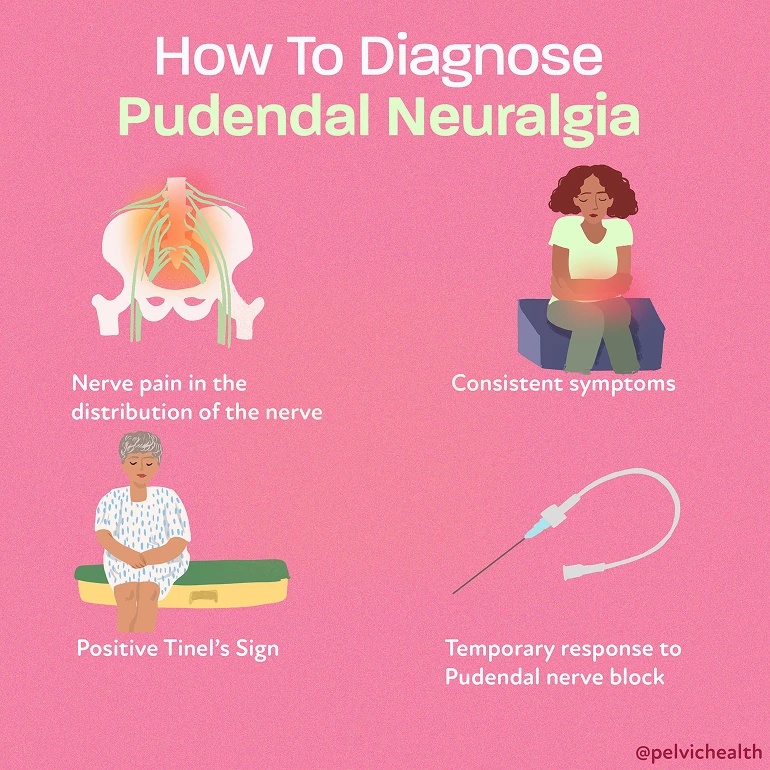
How Is Pudendal Neuralgia Diagnosed?
Pudendal neuralgia isn’t well understood by the majority of medical providers, which makes getting an accurate diagnosis difficult for most people. Medical and physical and occupational therapy schools do not include training on pudendal neuralgia. Providers aren’t trained to recognize the condition, let alone feel confident recommending treatment. Because of this, many people end up trying to diagnose themselves, often after reading online that pelvic pain while sitting might mean pudendal neuralgia.
But sitting pain or nerve pain in the vagina or pelvis can come from many different sources, and not all nerve-related pelvic pain involves the pudendal nerve. There are multiple nerves that serve the pelvic region, so it takes a skilled provider to narrow down the true source or sources of pain.
Diagnosing pudendal neuralgia involves a detailed clinical evaluation. There is no single test that confirms the diagnosis. Instead, a diagnosis is made based on your symptoms, a thorough medical history, and a physical exam that assesses your pelvic floor muscles, joint mobility, nerve sensitivity, and movement patterns. Your provider might also rule out other possible causes of pelvic pain through imaging or referrals to specialists.
One main part of the diagnostic process is identifying patterns that match pudendal nerve involvement, such as pain worsened by sitting, burning or stabbing sensations in the pudendal nerve distribution, and relief when sitting on a toilet or cut-out cushion.
Another challenge lies in separating pudendal neuralgia from pudendal nerve entrapment. While the symptoms might overlap, entrapment means the pudendal nerve is physically compressed or stuck somewhere along its path. Right now, there’s no reliable imaging or diagnostic test that can confirm pudendal nerve entrapment. The only way to know for sure is during surgical decompression of the nerve, which isn’t a path most people take without exhausting other options first.
Thankfully, awareness is growing. More providers now recognize the signs of pudendal neuralgia and know when to refer patients to specialists. At PHRC, we help clients understand what’s contributing to their pain and guide them toward a diagnosis that actually fits their experience.
What are the Associated Diagnoses?
Pudendal neuralgia often overlaps with or is mistaken for other pelvic conditions. These associated diagnoses can either contribute to pudendal nerve irritation or exist alongside it, making the pain more complex. Below are some of the most common:
Myofascial Pelvic Pain Syndrome
This condition involves chronic tightness and trigger points in the pelvic floor muscles. When the muscles stay in a guarded or overactive state, they can compress nearby nerves—including the pudendal nerve—leading to nerve-like symptoms even when the issue is muscular.
CPPS (Chronic Pelvic Pain Syndrome or Male Pelvic Pain Syndrome)
CPPS is a broad diagnosis used when men experience persistent pelvic pain without a clear infection or medical cause. Symptoms might include testicular pain, perineal discomfort, and urinary or sexual issues. In many cases, the pudendal nerve plays a role, but the pain can also stem from other nerves or musculoskeletal dysfunction.
Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often affecting pelvic structures. It can lead to widespread inflammation, adhesions, and nerve irritation. In some individuals, endometriosis contributes to pelvic nerve pain or creates a sensitized environment that makes pudendal neuralgia more likely.
Vestibulodynia
Vestibulodynia is characterized by pain at the vaginal opening (vestibule), often described as burning, rawness, or irritation. While it can have hormonal or inflammatory roots, it’s sometimes related to nerve hypersensitivity or pelvic floor muscle dysfunction that overlaps with pudendal neuralgia.
Pudendal Nerve Entrapment
This is a specific condition where the pudendal nerve becomes compressed or mechanically stuck along its path through the pelvis. While all entrapments involve pudendal neuralgia, not all cases of pudendal neuralgia are due to entrapment. Diagnosing entrapment remains difficult without surgical confirmation.
“Cyclist’s Syndrome”
This is also known as pudendal neuralgia, caused by prolonged pressure on the perineum, this condition often affects cyclists due to long hours on a bike seat. The constant compression can irritate or damage the pudendal nerve, resulting in pain or numbness in the pelvic area.
What Role Does Pelvic Floor Dysfunction Play in Pudendal Neuralgia?
The pelvic floor is a group of muscles across the bottom of the pelvis, supporting your bladder, bowel, and reproductive organs. These muscles also help with posture, core stability, and bowel and bladder control. Just like any other muscle group, they can become tight, weak, or uncoordinated—and when that happens, they can contribute to pain and dysfunction.
Pelvic floor dysfunction is often a leading cause of pudendal neuralgia. When these muscles stay in a chronically tight or overactive state, they can place pressure on the pudendal nerve or nearby structures. Over time, this ongoing tension can irritate the nerve, leading to burning, stabbing, or aching sensations along its path.
The pudendal nerve travels through very narrow spaces between muscles, ligaments, and fascia. If those tissues are restricted or inflamed, they can trap or compress the nerve. In some cases, the body reacts to this pain by guarding or clenching the pelvic floor even more, creating a cycle that’s hard to break without targeted intervention.
That’s why treating the muscular and structural imbalances of the pelvic floor is such an important part of finding relief from pudendal neuralgia.
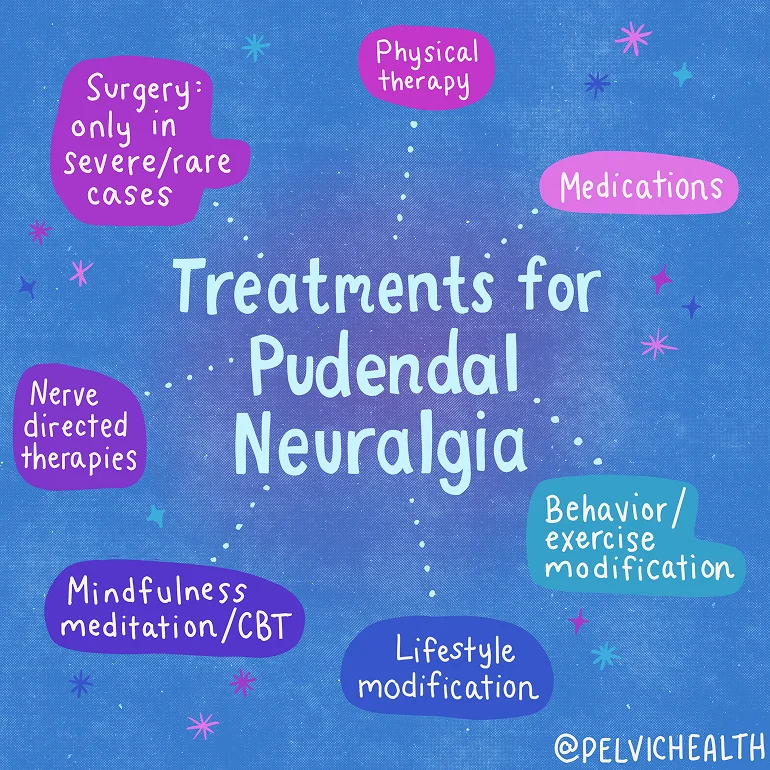
What is the Treatment for Pudendal and Pelvic Neuralgias?
Most cases of pelvic and pudendal neuralgias have a neuro-muscular pelvic floor and girdle component. Therefore, pelvic floor physical or occupational therapy should always be offered as a first-line treatment for these syndromes. Because these syndromes affect urinary, bowel, and sexual dysfunction as well as daily comfort and ability to perform professional and recreational activities, interdisciplinary care that includes the following treatments can be the most effective:
- Pelvic floor physical therapy or occupational therapy
- Pharmacologic management with a pain management doctor
- Procedural interventions (nerve blocks, Botox injections to surrounding dysfunctional muscles, regenerative injections such as PRP or stem cells, dry needling)
- Pain Science education and stress management strategies
- Temporary lifestyle modifications
- Surgical intervention in cases of suspected entrapment
How Pelvic Floor Physical and Occupational Therapy Helps
Pelvic floor physical and occupational therapy targets the underlying causes of pudendal nerve irritation by treating the muscles, joints, nerves, and soft tissue of the pelvic region. At PHRC, we use a variety of techniques to calm the nervous system, release muscle tension, and improve mobility.
Treatment includes:
- Assessing the pelvic floor muscles for overactivity, weakness, or restriction
- Using manual therapy to release tight muscles, fascia, and scar tissue
- Retraining the pelvic floor and core muscles to improve coordination and reduce strain
- Incorporating breathwork and relaxation techniques to calm the nervous system and reduce pain
- Addressing posture, walking mechanics, and movement patterns that may contribute to ongoing tension
- Coordinating care with other providers (such as pain management specialists, gynecologists, or surgeons) as part of a comprehensive approach
Pelvic floor PT is often part of a larger care plan. For many people with pudendal neuralgia, it’s one of the most effective ways to reduce pain, improve function, and return to a more comfortable life.
What To Expect During a Physical and Occupational Therapy Session
If you’re dealing with pelvic pain from pudendal neuralgia, starting with a physical and occupational therapist who specializes in pelvic pain can be an important step toward relief.
At your first visit, we take time to understand your full story. We’ll go over your symptoms, past diagnoses, previous treatments, and how those treatments have worked—or haven’t. Many people come to us feeling frustrated after seeing multiple providers, and we recognize just how challenging that journey can be.
During the physical exam, we assess your muscles, joints, connective tissue, nerves, and how your body moves. This hands-on evaluation helps us figure out what’s contributing to your pain.
After the assessment, we walk you through what we found and explain how these patterns might be related to pudendal neuralgia.
From there, we create a plan with both short-term and long-term goals based on your needs. Most people benefit from coming to physical and occupational therapy one to two times per week for about 12 weeks. You’ll also receive a home exercise program designed to support your progress between visits.
Throughout your care, we collaborate with your broader treatment team (including medical doctors and other specialists) to keep everyone on the same page. Our goal is to help you reduce pain, move with more ease, and get back to living your life more comfortably.
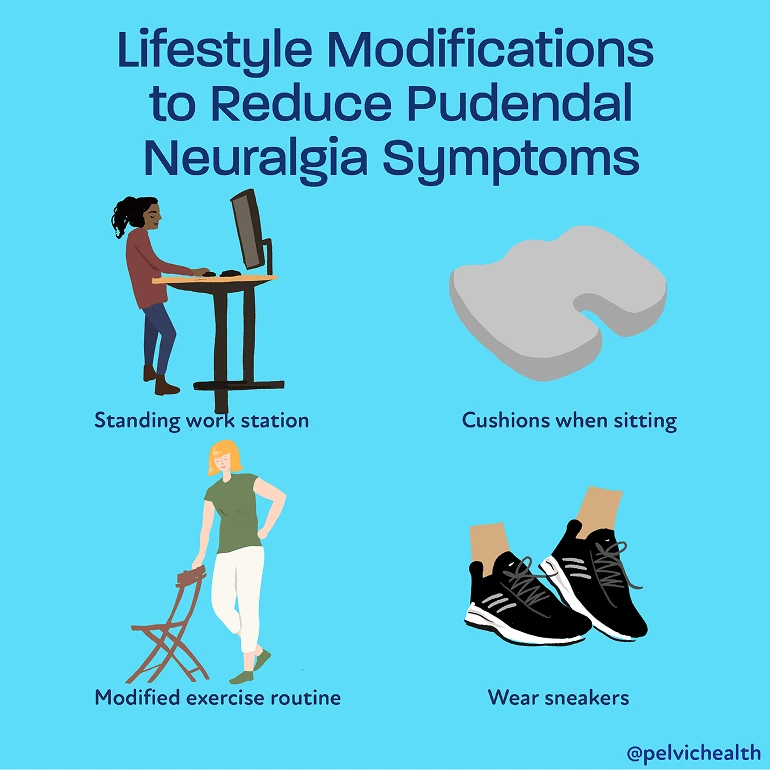
Tips for Living with Pudendal Neuralgia
Managing pudendal neuralgia often requires a mix of treatment and day-to-day strategies. While physical and occupational therapy plays a big role, small adjustments to your routine can also make a difference in how you feel. Here are some practical tips we often share with clients:
- Use a cut-out cushion when sitting to reduce pressure on the pudendal nerve
- Take standing breaks or walking breaks regularly if your job or lifestyle involves long periods of sitting
- Avoid activities that increase symptoms, such as deep squats, heavy lifting, or cycling
- Focus on gentle movement like walking, stretching, or low-impact exercise to keep circulation flowing
- Practice deep breathing and relaxation techniques to help downtrain the nervous system and reduce muscle tension
- Stay consistent with your home exercise program as guided by your pelvic floor physical and occupational therapist
- Track your symptoms to notice patterns or triggers you can adjust
- Be patient with your progress since healing from pudendal neuralgia often happens gradually
- Seek emotional support through therapy, support groups, or trusted friends, especially if the pain has impacted your quality of life
You’re not alone in this. With the right care, self-awareness, and ongoing support, it is possible to manage symptoms and reclaim your comfort.
Get Help Today at PHRC
Living with pudendal neuralgia can be exhausting, especially when answers feel hard to come by. At PHRC, we’re here to listen, assess, and guide you toward meaningful relief. We take a whole-body approach to care, focusing not just on your symptoms but on the underlying patterns that contribute to them.
Our team of pelvic floor physical and occupational therapists brings both clinical expertise and genuine compassion to every session. We work with you to build a plan that fits your life and helps you move forward.
If getting to the clinic is a challenge, we offer telehealth appointments following your first in-person visit, so you can keep making progress no matter where you are.
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
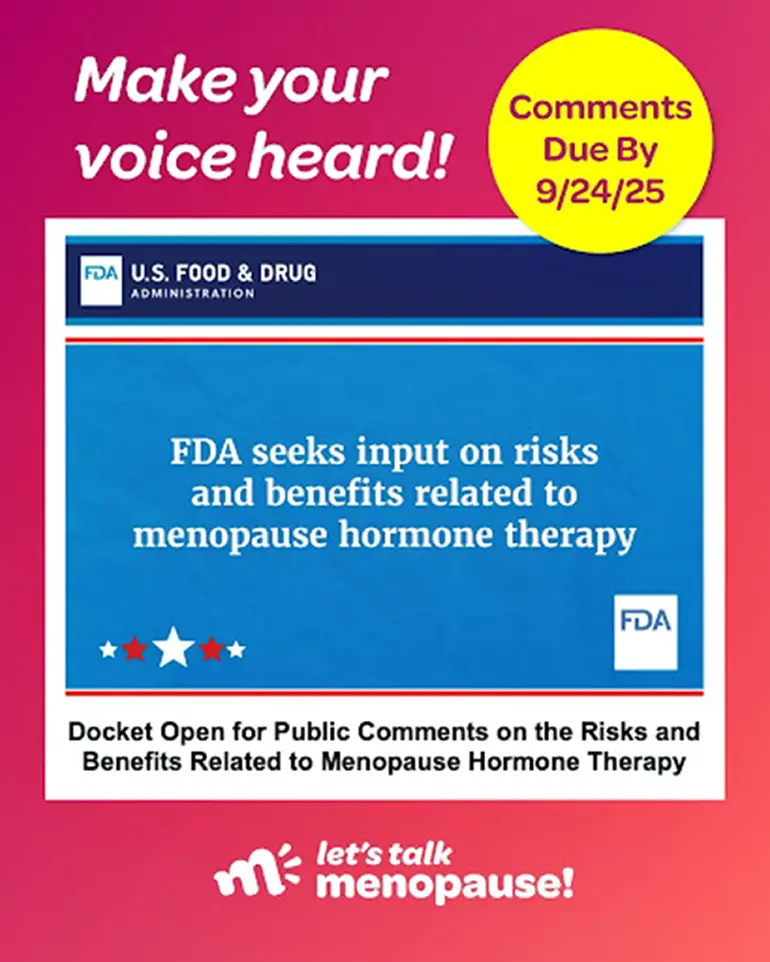
My name is Stephanie Prendergast. I am a pelvic floor physical therapist, co-founder of the Pelvic Health and Rehabilitation Center, past-President of the International Pelvic Pain Society, and faculty for the International Society for the Study of Women’s Sexual Health. Over the course of my career I have cared for thousands of women and educated countless medical providers. I am also in perimenopause myself, and a daughter, niece, and friend to many women who have faced these challenges.
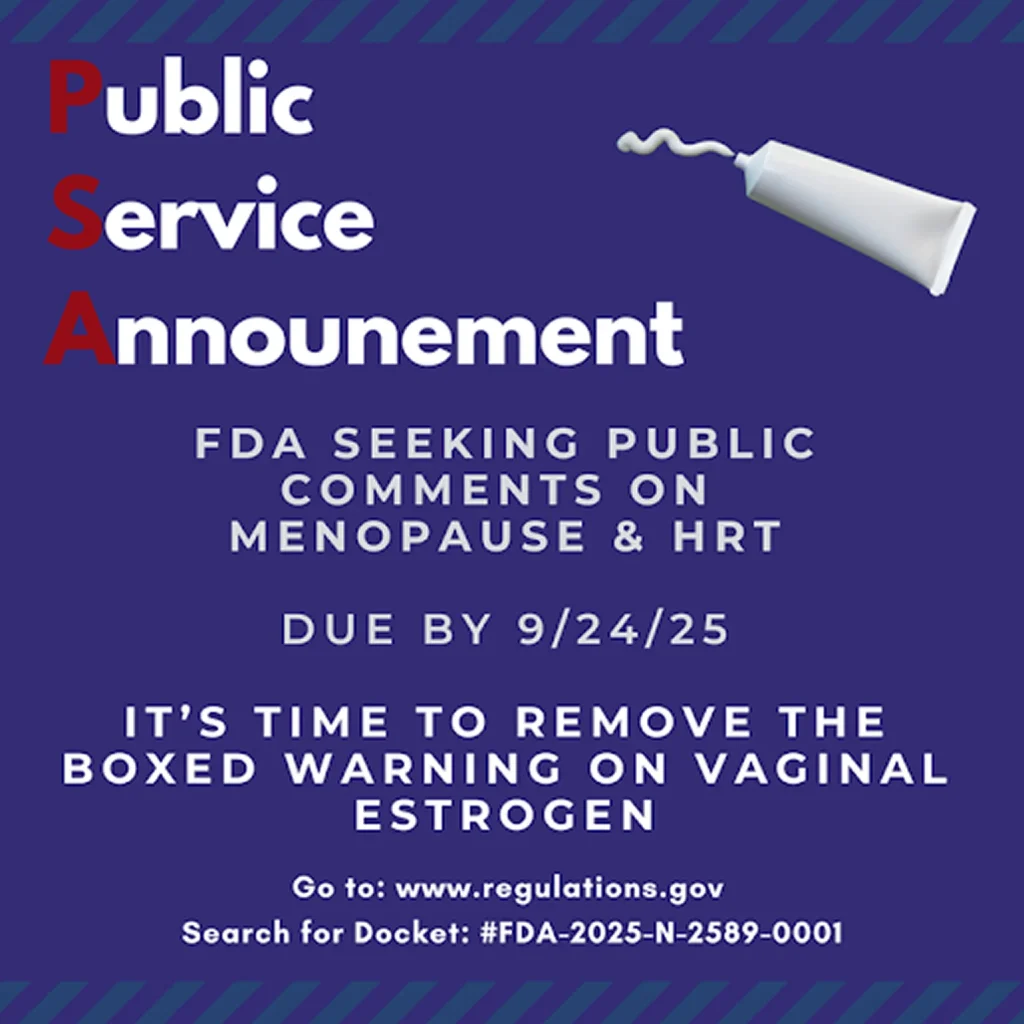
In our clinics, we treat women suffering from vaginal dryness, dyspareunia, bladder irritation, and recurrent urinary and vaginal infections—conditions that frequently overlap with pelvic floor dysfunction. Physical and occupational pelvic health therapists are trained to differentiate musculoskeletal causes from hormonal deficiencies, but our ability to help patients is undermined when safe, effective treatment—vaginal estrogen—is stigmatized by inaccurate labeling.
The current FDA labeling creates fear and confusion. Patients read warnings that contradict decades of clinical evidence, and physicians—many of whom already lack training in menopause care—often tell women that vaginal estrogen causes cancer or other health problems. This is simply not true. Yet the weight of FDA labeling and a physician’s authority outweighs the reassurance of any physical or occupational therapist, no matter how experienced. This labeling is harming women’s health and must be corrected.
I also write to you as a daughter. Several years ago, my mother developed severe symptoms that were repeatedly misdiagnosed or worse, undiagnosed all together. It turned out the problem was recurrent urinary tract infections. She was treated with rounds of antibiotics that destroyed her gut, caused weight loss, and left her debilitated. Despite seeing gynecologists, urologists, and primary care physicians, she was never offered hormonal therapy. At age 70, after months of suffering, she finally received vaginal estrogen under my advocacy. Within one month, her symptoms resolved. She has thrived ever since—yet even now, she faces ongoing barriers: physicians unwilling to prescribe it, pharmacies accusing her of “overuse,” and the stress of navigating a system shaped by misinformation. If I had not been able to advocate for her, I fear her decline would have continued.
My mother’s story is not unique. I see these patterns in my patients daily. Safe, effective, low-dose vaginal estrogen restores health and dignity, yet women are denied it because of misleading FDA labeling.
On behalf of my patients, my profession, and my family, I urge the FDA to correct this error. Accurate labeling will empower women, guide providers, and reduce unnecessary suffering. As healthcare providers, we fight many uphill battles for our patients—please make this one easier.
Everyone deserves pelvic comfort, health, and wellbeing. Please do the right thing and change the label.
Respectfully,
Stephanie Prendergast, PT, MPT

Due 9/24/25 11:59pm EDT
Still time to rally!
It’s super easy
Click → “Comment” → Follow the prompts.
By Stephanie Prendergast, MPT, PHRC Pasadena
Pain science education (PSE)—sometimes called pain neuroscience education—aims to help people understand what pain is, how it’s produced by the nervous system, and why it can persist even after tissues have healed. In chronic pelvic pain, where biological, psychological, and social factors often intertwine, that reconceptualization can be powerful: it can lower fear, boost self-efficacy, and open the door to graded movement, pelvic floor relaxation, and other active strategies. But how strong is the evidence specifically for pelvic pain?
What PSE is (and isn’t)
PSE is not a pep talk and it’s not a substitute for medical work-up. It’s structured learning about pain biology that targets threat appraisal, catastrophic thinking, and protective behaviors (like over-guarding the pelvic floor). A recent international e-Delphi study distilled 92 clinician-endorsed learning points for pelvic pain into 13 core concepts—e.g., “pelvic pain involves changes in the nervous system,” “pain ≠ damage,” “many factors (sleep, stress, hormones, pelvic floor tone) can amplify pain,” and “pelvic pain can change and improve.” It also highlights pelvic-specific themes such as cross-organ sensitization and why flares don’t necessarily mean disease is worsening. These clinician-derived concepts provide a concrete curriculum to guide care and future trials. Frontiers
Do guidelines recommend education for pelvic pain?
Yes. A systematic review of 17 international clinical practice guidelines for benign gynecologic and urologic conditions associated with persistent pelvic pain found that two-thirds explicitly recommend patient education, though they vary on what to teach and how to deliver it (e.g., written materials, support groups). The authors also noted guideline quality was mixed and called for better, tailored education interventions. PubMed
For men with chronic pelvic pain/chronic prostatitis, the 2025 American Urological Association guideline similarly emphasizes a biopsychosocial approach that includes patient education and psychological therapies such as CBT, alongside pelvic floor therapy and other modalities. American Urological Association
What’s the direct evidence for PSE in pelvic pain?
Although the pelvic-specific PSE literature is still maturing, early data are encouraging:
- Knowledge changes after a single seminar. In a pre–post study of women with chronic pelvic pain, a 90-minute neuroscience-based seminar significantly improved scores on the Neurophysiology of Pain Questionnaire and deepened conceptual understanding. Knowledge isn’t a clinical endpoint, but it’s a key mechanism target for PSE. Sydney Pelvic Clinic
- Randomized trial in genito-pelvic pain/penetration disorder (GPPPD). A three-arm RCT tested four weekly educational workshops (covering pelvic anatomy, pain neuroscience, and sexuality) delivered face-to-face or online versus waitlist. Both active formats improved pain intensity, pain-related outcomes (e.g., catastrophizing), and sexual function—benefits that did not depend on socioeconomic status. While the package included anatomy and sexuality content alongside PSE, it’s a rare randomized signal that an education-centric program can improve clinically meaningful outcomes in pelvic pain. SpringerLink
- Biopsychosocial programs where PSE is a core component. A 2025 systematic review of 14 RCTs in women with chronic pelvic pain found CBT and ACT-based approaches, mindfulness, and physiotherapy-based programs reduced pain and improved emotional outcomes. Across intervention types, two elements kept showing up as important: pain science education and structured exposure/engagement with valued activity. This points to PSE as a common “active ingredient” in effective multimodal care. PMC
Taken together, these findings suggest PSE helps patients reconceptualize their pain and, when paired with active strategies, can contribute to reductions in pain and distress in pelvic pain populations. The evidence base is still smaller than in back or neck pain, but it’s growing.
What about the much larger (non-pelvic) PSE literature?
Zooming out helps calibrate expectations. An umbrella review across chronic musculoskeletal pain concluded that PSE added to active treatments (most often exercise) tends to yield greater improvements—especially for psychosocial targets like catastrophizing and kinesiophobia—than the same treatments without PSE. By contrast, PSE alone shows inconsistent effects on pain and disability. The message is clear: use PSE as a catalyst within a broader active plan, not as a standalone. Frontiers
What patients say they need from PSE
A 2024 qualitative study asked women with “improved” pelvic pain what PSE ideas mattered most. Four themes stood out: (1) a sensitized nervous system can become overprotective (validation), (2) pain doesn’t always mean damage (reassurance and reduced fear), (3) thoughts, feelings, and attention can amplify pain (self-management levers), and (4) pain can change, slowly (hope plus a realistic time course). These patient-voiced concepts align well with the clinician-derived curriculum above and reinforce the need for tailored, stigma-reducing language. PubMed
Practical takeaways for clinicians and patients
- Tailor the content. Start with core concepts (pain ≠ damage; sensitization; many contributors) and add pelvic-specific pieces: pelvic floor guarding and down-training, cross-organ sensitization (e.g., bladder–bowel–pelvic floor “crosstalk”), hormonal influences (adolescence, perimenopause), and how flares can be managed without panic. The new pelvic pain PSE curriculum is a helpful scaffold. Frontiers
- Pair PSE with active strategies. Use education to lower threat and increase confidence, then lock in gains with graded movement, pelvic floor relaxation training, sexual pain pacing strategies, sleep/stress skills, and goal-oriented exposure to valued activities. This mirrors what effective RCT programs actually do. PMC
- Mind the psychosocials. Catastrophizing, fear-avoidance, and low self-efficacy are common in pelvic pain and are responsive targets for PSE and CBT-style skills. Major guidelines recommend integrating behavioral therapies and patient education into care plans. PubMedAmerican Urological Association
- Delivery can be flexible. Group workshops (with partner inclusion), one-to-one sessions, printed/online materials, and telehealth can all work. The GPPPD RCT suggests online and face-to-face education can be similarly effective when content and structure are sound. SpringerLink
Where the evidence is still thin
We still need larger, high-quality pelvic-specific RCTs that isolate the contribution of PSE, report core outcomes, and test dose, timing, and delivery (individual vs group; in-person vs digital). Encouragingly, researchers have now defined what to teach; the next step is rigorous trials testing how best to teach it and for whom. Meanwhile, multimodal programs that include PSE remain the most evidence-aligned option. FrontiersPMC
References
American Urological Association. (2025). Male chronic pelvic pain guideline. https://www.auanet.org/guidelines-and-quality/guidelines/male-chronic-pelvic-pain-guideline American Urological Association
James, A., Thompson, J., Neumann, P., & Briffa, K. (2019). Change in pain knowledge after a neuroscience education seminar for women with chronic pelvic pain. Australian and New Zealand Continence Journal, 25(2), 39–44. (PDF). Sydney Pelvic Clinic
Johnson, S., Bradshaw, A., Bresnahan, R., Evans, E., Herron, K., & Hapangama, D. K. (2025). Biopsychosocial approaches for the management of female chronic pelvic pain: A systematic review. BJOG, 132(3), 266–277. https://doi.org/10.1111/1471-0528.17987 (Open Access). PMC
Mardon, A. K., Leake, H. B., Szeto, K., Moseley, G. L., & Chalmers, K. J. (2024). Recommendations for patient education in the management of persistent pelvic pain: A systematic review of clinical practice guidelines. Pain, 165(6), 1207–1216. https://doi.org/10.1097/j.pain.0000000000003137 PubMed
Mardon, A. K., Leake, H. B., Wilson, M. V., Karran, E. L., Parker, R., Malani, R., Moseley, G. L., & Chalmers, K. J. (2025). Pain science education concepts for pelvic pain: An e-Delphi of expert clinicians. Frontiers in Pain Research, 6, 1498996. https://doi.org/10.3389/fpain.2025.1498996 (Open Access). Frontiers
Mardon, A. K., Chalmers, K. J., Heathcote, L. C., et al. (2024). “I wish I knew then what I know now”—Pain science education concepts important for female persistent pelvic pain: A reflexive thematic analysis. Pain, 165(9), 1990–2001. https://doi.org/10.1097/j.pain.0000000000003205 PubMed
Cuenca-Martínez, F., et al. (2023). Pain neuroscience education in patients with chronic musculoskeletal pain: An umbrella review. Frontiers in Neuroscience, 17, 1272068. https://doi.org/10.3389/fnins.2023.1272068 (Open Access). Frontiers
Lopez-Brull, A., Pérez-Domínguez, B., Cantón-Vitoria, L., Plaza-Carrasco, M., & Nahon, I. (2023). Association levels between results from a therapeutic educational program on women suffering from genito-pelvic pain/penetration disorder and their socioeconomic status. Sexuality Research and Social Policy, 20, 1180–1187. https://doi.org/10.1007/s13178-023-00790-7 (Open Access; includes RCT methods and outcomes). SpringerLink
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!