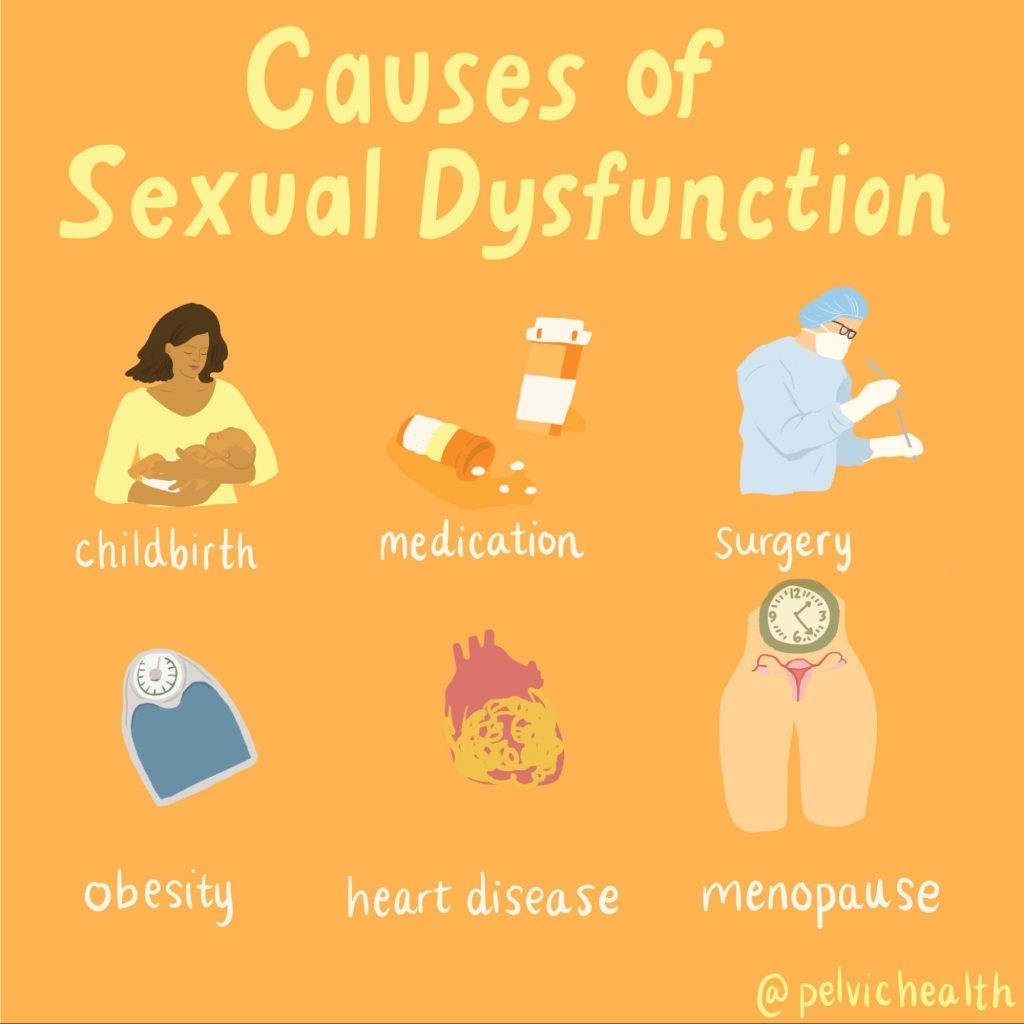
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

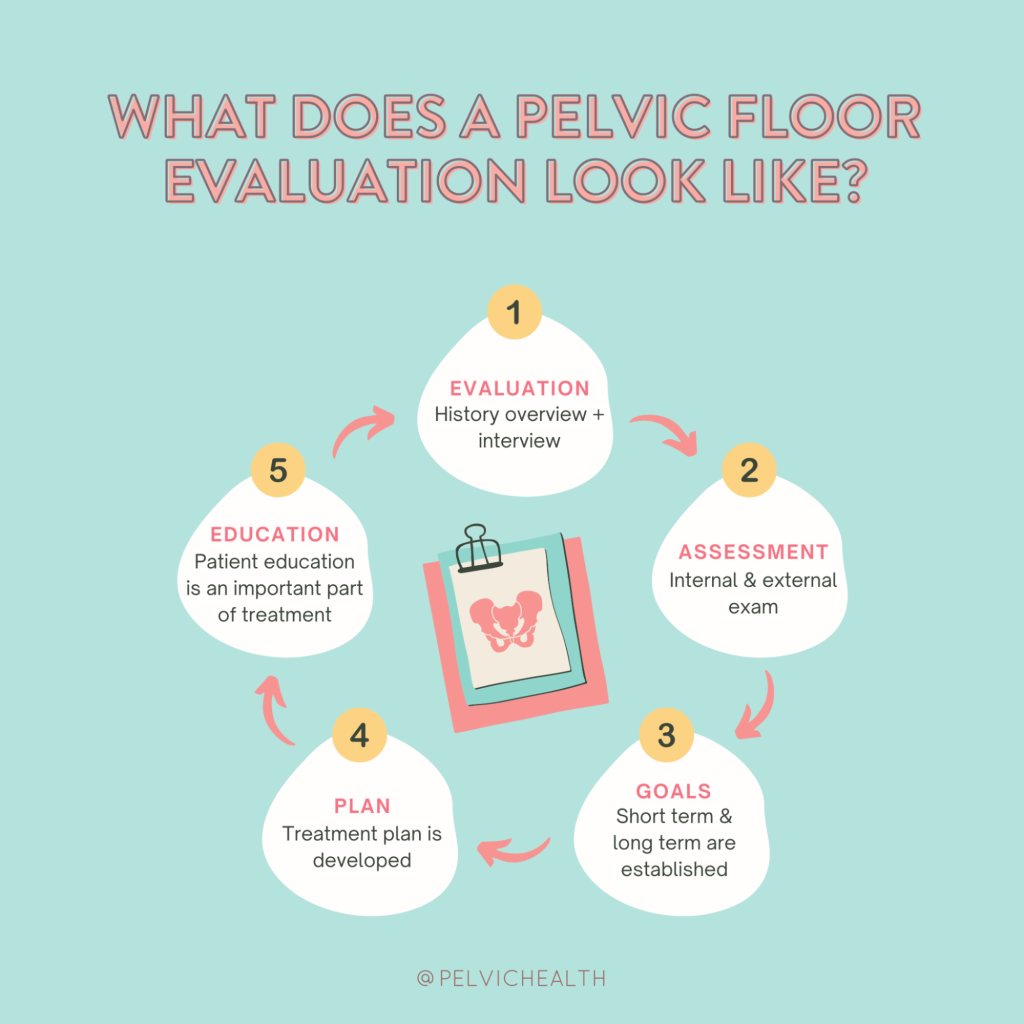
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
The Big “O” – Let’s talk Updates in Care
By Jandra Mueller, DPT, MS, PHRC Encinitas
When people hear the word “orgasm,” most people probably think about ‘pleasure.’ What actually is an orgasm? When it comes to truly understanding this complex physiological and psychological phenomenon—especially in clinical settings—the conversation is much more nuanced. At the 2025 ISSWSH/ISSM Annual Meeting, leading experts in sexual medicine presented new insights into the science of orgasm, updated definitions, and proposed frameworks for diagnosing and managing orgasmic dysfunction. Here’s a breakdown of the key highlights.
Understanding the Orgasm: From Definition to Complexity
The 2016 ISSWSH definition of orgasm was groundbreaking in its time. It described orgasm as
“a variable, transient, peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
Fast forward to 2025, and researchers and clinicians are calling for a more clinically applicable definition—one that supports diagnosis and treatment.
“Orgasm is a feeling of intense pleasure that evolves over three phases: the pre-orgasm phase is generated by repetitive genital and/or non-genital stimulation increasing physiologic arousal and whole body myotonia resulting in awareness of a progressive increase “climb” in excitation; the orgasm phase reaches one or more peaks of excitation that trigger(s) an inhibitory process resulting in relaxation of the myotonia, cessation of the stimulation and de-activation/resolution of the excitation perceived as intensely pleasurable, and ending with satiety and/or contentment; and the post-orgasm phase is the return to the baseline state. Orgasm may be accompanied by concomitant ejaculation.”
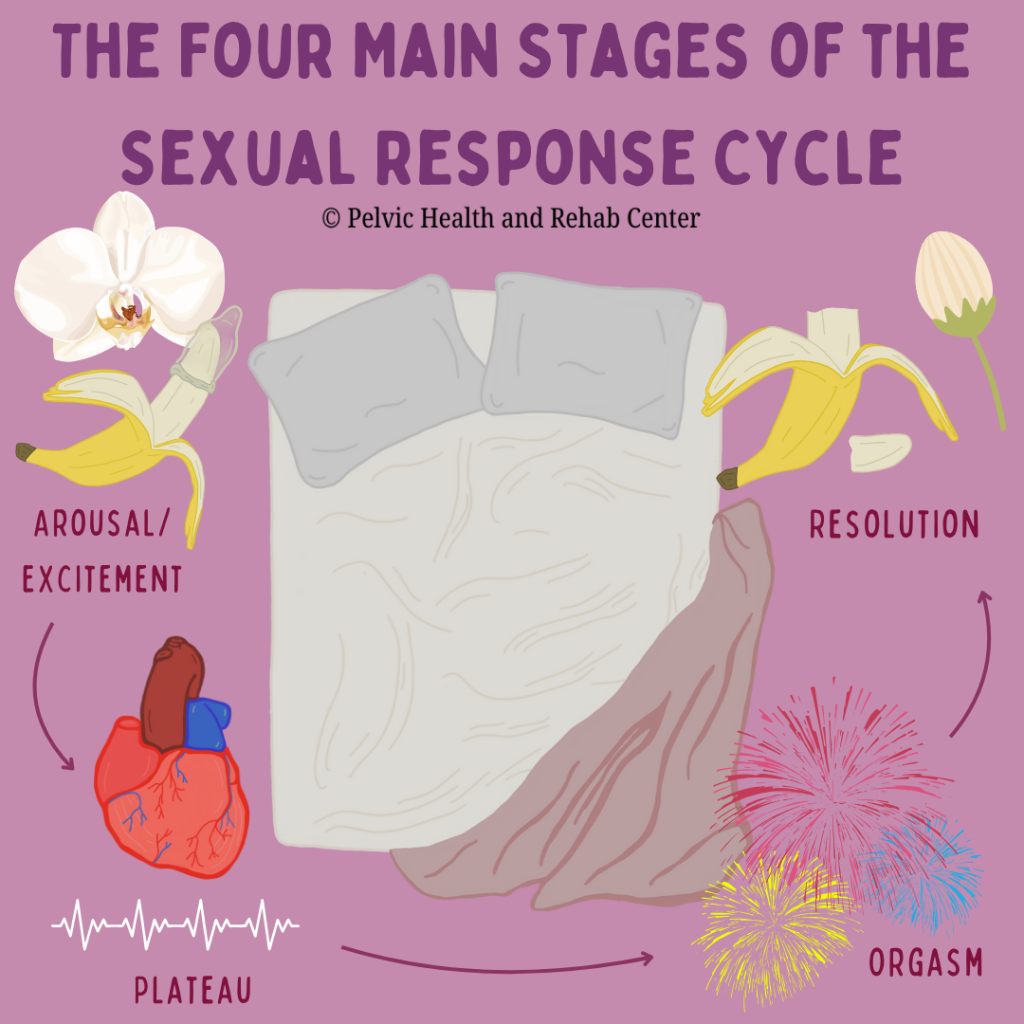
The proposed update defines orgasm as an evolving three-phase experience:
- Pre-Orgasm Phase – Characterized by increasing arousal and whole-body muscle tension (myotonia) from repetitive stimulation.
- Orgasm Phase – A climax of excitation that triggers an inhibitory process, resulting in relaxation, cessation of stimulation, and intense pleasure.
- Post-Orgasm Phase – A return to baseline marked by satiety and contentment.
This new model aligns with clinical observations and offers a more actionable approach to identifying dysfunctions within these phases.
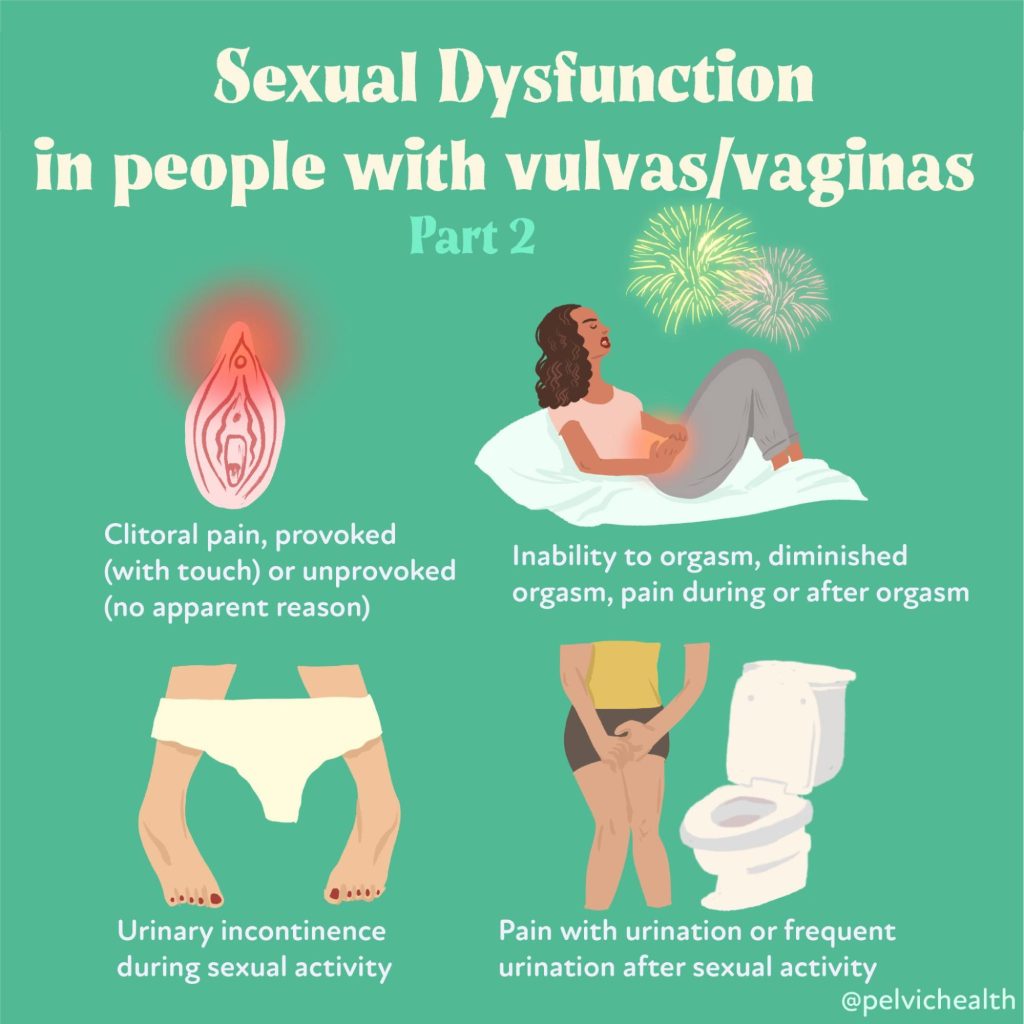
Defining Orgasmic Dysfunction
Female orgasmic disorder (FOD) is defined as
“Persistent or recurrent, distressing compromise of orgasm frequency, intensity, timing, and or pleasure associated with sexual activity for a minimum of 6 months.”
This new definition emphasizes distress and duration as critical qualifiers. It’s not just about whether an orgasm occurs—but whether its absence, delay, or change in quality is causing concern or impacting well-being.
Problem or Dysfunction?
An important point was made that some people do not have distress if a problem is occurring; therefore, there may not be any need to intervene. However, when there is a problem, and there is distress around it, it is defined as a dysfunction; and intervention is warranted.
The “Big O” has four measurable components:
- Frequency – Orgasms occur less often or are entirely absent.
- Intensity – The sensations are dulled or “muted.”
- Timing – The orgasm may be delayed, spontaneous, or prematurely triggered.
- Pleasure – Orgasm happens without the expected euphoria, a condition termed “orgasmic anhedonia.”
Functional Subtypes of Female Orgasmic Disorder (FOD)
Dr. Irwin Goldstein and Dr. Barry Komisaruk presented clinical illustrations of how female orgasmic disorders can manifest across the orgasmic spectrum. Their research breaks FOD into subtypes based on where in the orgasm cycle dysfunction occurs:
- Failure to Excite (Pre-Orgasm Phase)
– The individual never reaches the threshold for orgasm.
– There’s minimal awareness of myotonia and no sense of climax or satisfaction.
– Often results in frustration and emotional distress. - Failure to Inhibit (Pre-Orgasm Phase)
– Sensitivity increases but becomes aversive, leading to discomfort rather than pleasure.
– Orgasm never occurs, and the arousal climb results in avoidance or distress. - Delayed Orgasm (Across Pre/Orgasm Phases)
– Orgasm may eventually occur, but only after prolonged effort.
– It can be emotionally and physically fatiguing, and the reward may be blunted. - Muted or Premature Orgasm (Minimal Excitation/Inhibition)
– Orgasms occur at low thresholds, often prematurely, with muted pleasure.
– The experience lacks emotional and physical satisfaction. - Orgasmic Anhedonia
– The physiological climax occurs, but no pleasure is felt.
– There is a complete disconnect between bodily release and emotional fulfillment. - Post-Orgasm Illness Syndrome (POIS)
– A rare and poorly understood condition marked by protracted malaise, fatigue, brain fog, and emotional dysregulation following orgasm.
– Symptoms can persist for days to weeks.
Addressing the Root Causes: Questions Every Clinician Should Ask
When assessing a patient with suspected orgasmic dysfunction, the context matters. Providers are encouraged to ask:
- Are orgasms absent, delayed, or reduced in intensity?
- Is there distress—and if so, how severe?
- Is the problem lifelong or acquired? Generalized or situational?
- Are other sexual concerns present (desire, arousal, pain)?
- Is there a partner-specific component?
- Are any medical, medication-related, psychological, or relational factors contributing?
- Is the patient receiving adequate and preferred types of stimulation?
These questions allow providers to differentiate between a clinical dysfunction and a personal or situational problem, helping avoid over-medicalization and ensuring that interventions are person-centered.
Emerging Treatment Strategies (Still Under Debate)
While none of the proposed pharmacologic treatments have reached consensus or FDA approval, several approaches are under investigation. These include medications aimed at:
- Enhancing excitation (e.g., dopaminergic agents)
- Reducing inhibition or anxiety (e.g., SSRIs, anxiolytics)
- Modulating sensory input to improve pleasure perception
- Addressing systemic inflammation and neurological triggers in conditions like POIS
It is critical to note that all proposed treatments are off-label, and decisions should be guided by expert opinion, individualized assessment, and safety considerations.
In addition to possible medications, pelvic floor and mental health therapists play an important role in helping to treat the whole person. A recent systematic review and meta-analysis by Jorge et al. (2024), demonstrated that pelvic floor therapy improved female sexual dysfunction. Our friend and colleague Dr. Erica Marchand reviewed current behavioral treatments for female orgasmic disorders in an article in Sexual Medicine Reviews (2021), highlighting the need for more research and a broader understanding of the various types to provide better treatment strategies.
Why This Matters
Understanding orgasmic function and dysfunction isn’t just about enhancing pleasure—it’s about supporting emotional health, intimacy, and self-esteem. For many individuals, difficulty achieving orgasm carries a deep psychological toll. As sexual health professionals, recognizing the spectrum of orgasmic experiences and dysfunctions can:
- Improve diagnostic accuracy
- Reduce shame and stigma
- Guide evidence-informed interventions
- Encourage open, validating conversations with patients
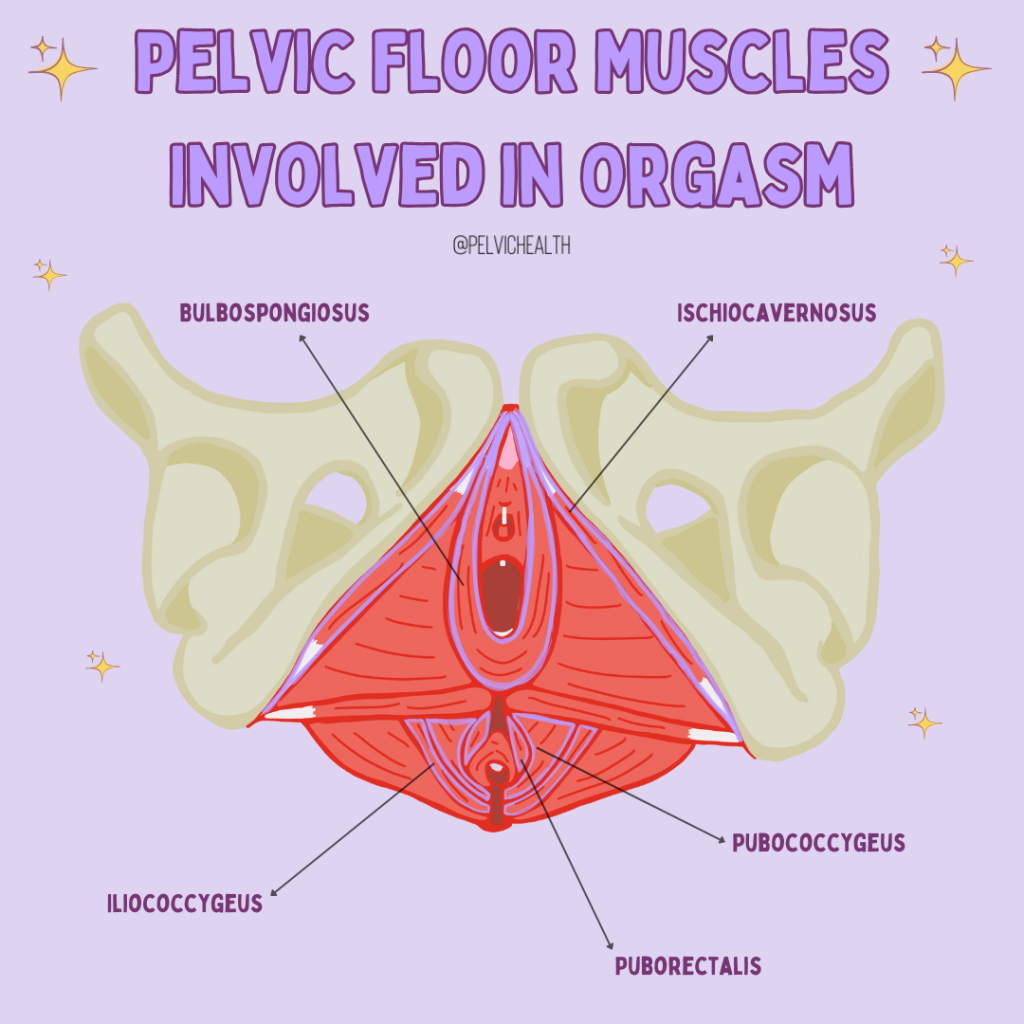
How Does Pelvic Floor Therapy Play a Role?
If you suffer from pelvic pain, or other conditions such as incontinence, sexual activity may not be something you find enjoyable and choose to engage in. Pelvic floor dysfunction and pelvic pain really is the ultimate mood killer. Both physical and occupational therapists who specialize in pelvic floor therapy can help to address the underlying problem, but are also incredible resources for getting you to a team of providers who can help treat the underlying causes.
Research and media articles often suggest a ‘strong’ pelvic floor is important for improving your sexual pleasure. This suggests that performing strengthening exercises (i.e. Kegels) should be done. This is actually not the case for most. Muscles work best at their optimal resting length which is neither too tight or too lax – both situations can result in weakness and difficulty reaching climax. The team at PHRC can help guide you as to what your individual needs are, refer you to other providers when there is more than just a muscle dysfunction, and can provide you with a number of resources so you can get back to having pleasurable sex.
Final Thoughts
The 2025 ISSWSH meeting underscores a fundamental truth: orgasm is more than a moment of pleasure—it’s a dynamic, biopsychosocial process. By shifting toward functional definitions, patient-centered assessment, and inclusive language, sexual health providers can move the conversation from mystery to medicine.
If you or someone you know is struggling with sexual concerns like difficulty reaching orgasm, know that help exists. Pelvic floor therapists, sex therapists, and trained sexual medicine providers can work together to develop an individualized approach—one that respects your body, your needs, and your right to pleasure.
Publications:
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
Ehlers-Danlos Syndrome & Hypermobility Spectrum Disorders: How Pelvic Floor Physical and Occupational Therapy Can Help
By Jandra Mueller, DPT, MS, PHRC Encinitas
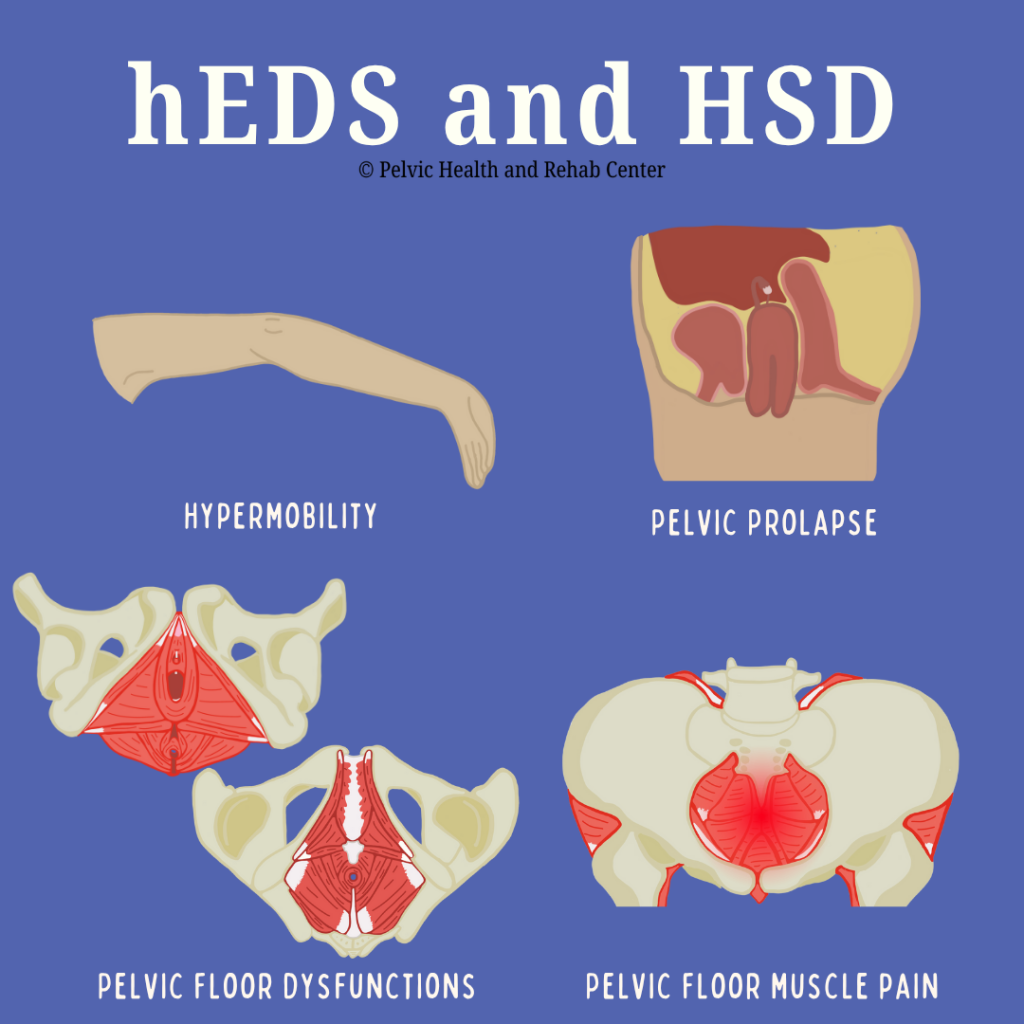
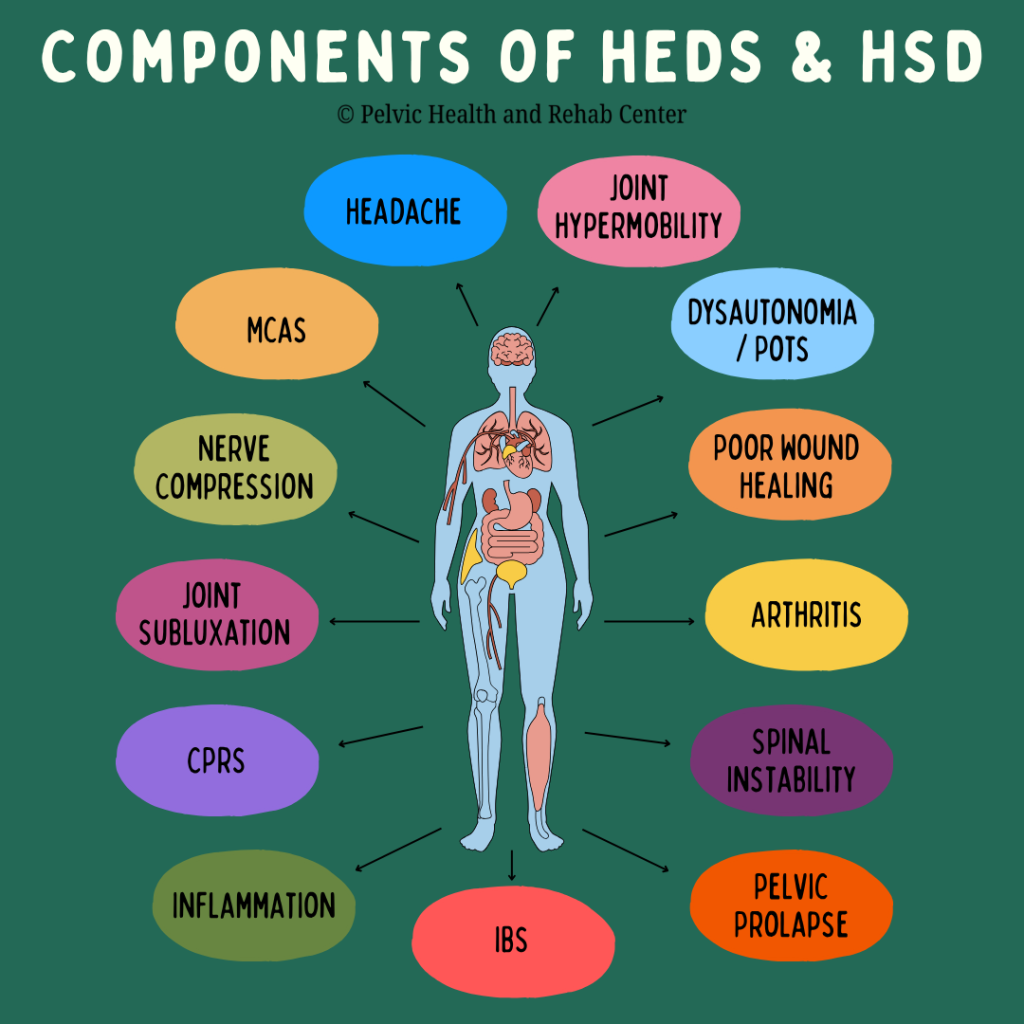
Ehlers-Danlos Syndrome (EDS) is a group of 13 heritable connective tissue disorders. Genetic changes impact our connective tissue, causing joint hypermobility, skin hyperextensibility, and tissue fragility. Though it’s a multisystemic condition, one of the often-overlooked aspects of EDS is its impact on the pelvic floor and sexual health concerns. People with EDS may suffer in silence from pelvic pain, bladder or bowel dysfunction, and sexual health concerns—but pelvic floor therapy offers hope and relief. As awareness of EDS has risen all of us at PHRC have become increasingly involved in helping patients improve their pelvic health despite having a genetic disorder. Let us explain!
What Is Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome (EDS) refers to a group of hereditary connective tissue disorders that result from defects in the body’s ability to produce strong collagen. There are 13 subtypes of EDS, with hypermobile EDS (hEDS) being the most common and also the only one currently without a known genetic marker. The two other more common forms are vascular EDS (vEDS) and classical EDS (cEDS), the other subtypes are extremely rare. People with EDS may appear outwardly healthy, but the systemic nature of this disorder affects multiple bodily systems, making it particularly complex to diagnose and treat.
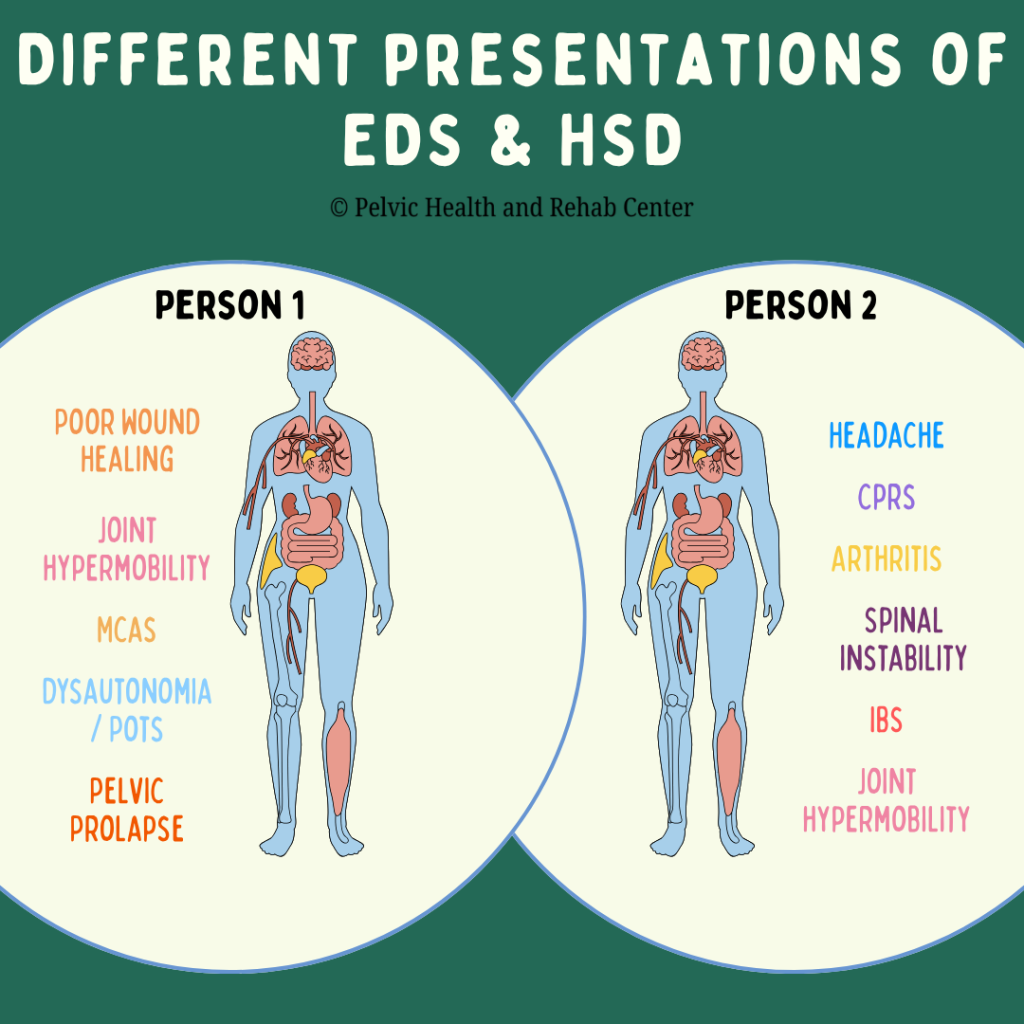
What Are Hypermobility Spectrum Disorders?
Hypermobility spectrum disorders (HSD) refers to joint hypermobility without meeting the criteria for hEDS or another condition. Similar to hEDS, most people experience joint hypermobility and chronic pain and there is a wide variety of symptoms and associated conditions present. It is important to know that HSD can present very differently from one person to the next.
Despite being relatively common (3% of the world’s population or 225 million people), EDS and HSD are often underdiagnosed or misdiagnosed; in part because there is no identified genetic marker present and symptoms can vary greatly. Symptoms can be debilitating and significantly impair quality of life. Early recognition and comprehensive, multidisciplinary management are critical for improving long-term outcomes.
Many regions in our body heavily rely on connective tissue for stability and optimal functioning. Many systems are often impacted by these disorders.
Below are some of the common findings in someone with hEDS or HSD:
- Chronic joint pain and dislocations
- Gastrointestinal issues (e.g., IBS or gastroparesis)
- Bladder dysfunction (urgency, frequency, incontinence)
- Pelvic organ prolapse
- Vulvovaginal pain
- Sexual dysfunction and pelvic pain
A recent article by Ritelli et al. (2024) focused on bridging the diagnostic gap and recognizes a number of other conditions related to hEDS and HSD:
- Chronic Fatigue
- Mast Cell Activation Syndrome (MCAS)
- Dysautonomia/Postural Orthostatic Tachycardia Syndrome (POTS)
- Headaches
- Anxiety
- Neurodivergence
The Overlap Between EDS, HSD and Pelvic Floor Dysfunction
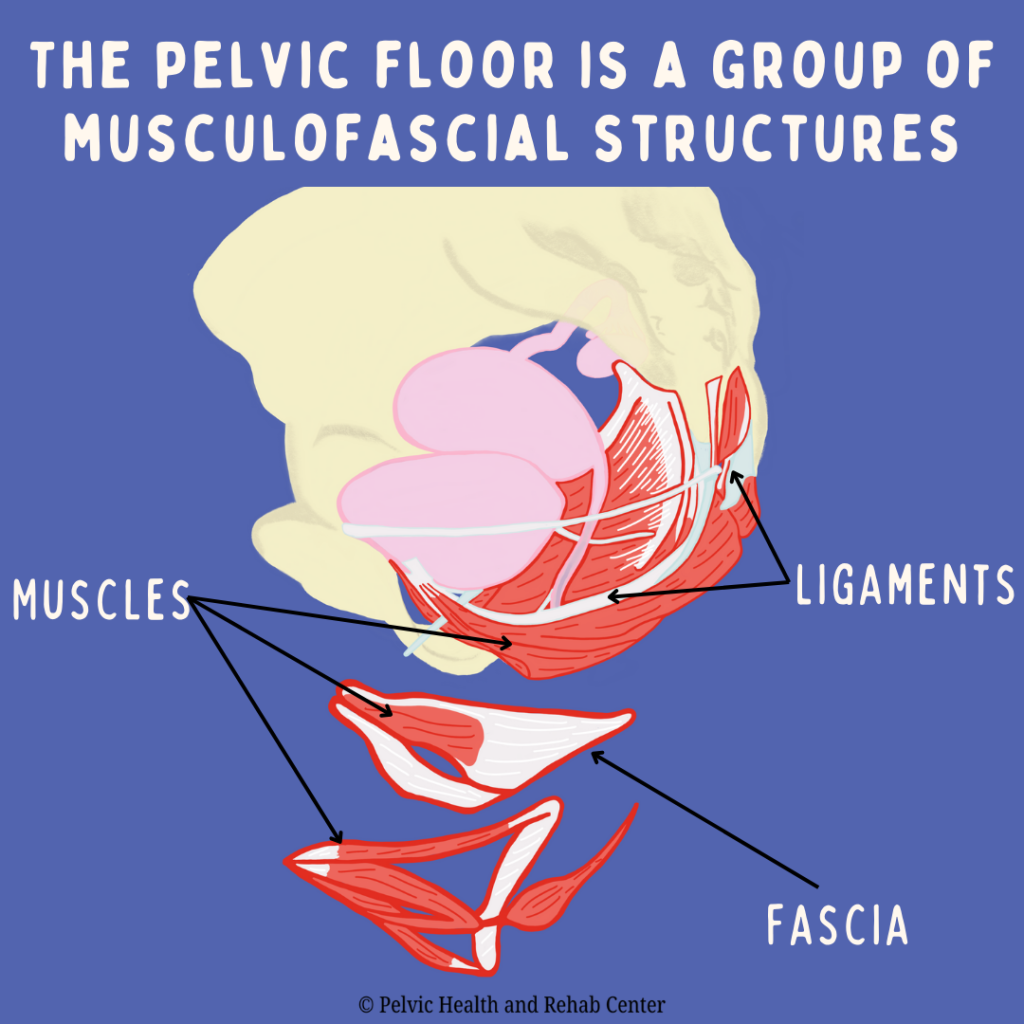
Pelvic floor dysfunction is especially prevalent among people with EDS and HSD due to the connective tissue abnormalities that impair structural support. The pelvic floor is made up of a group of musculofascial structures and plays a vital role in supporting the bladder, bowel, and reproductive organs. In those with EDS and HSD, laxity in these tissues can lead to instability, pain, and dysfunction.
Many people with EDS and HSD are disregarded or gaslit by medical providers and are left to feel their symptoms are “in their head” or unrelated; despite presenting with a clear pattern of multisystem dysfunction. Symptoms like urinary frequency, urgency, constipation, and pelvic organ prolapse can begin early and worsen over time. It is important that pelvic floor therapists should be familiar with multisystem dysfunctions, especially if their patients are not responding in the way that would be expected. When scheduling to see a pelvic floor therapist, it is helpful for patients to make their therapist aware of all symptoms or conditions, even if they think they are not related; and therapists should ask any pertinent questions when they see multisystem dysfunction so that they can modify or create a plan of care to avoid inappropriate exercise prescriptions or misinterpretation of pain responses during treatment.
Diagnosis of hEDS and HSD
Since hEDS does not have a genetic marker, healthcare providers can use the checklist “Diagnostic Criteria for Hypermobile Ehlers-Danlos Syndrome (hEDS)” from The International Consortium on Ehlers-Danlos Syndromes & Related Disorders and The Ehlers-Danlos Society. The clinical diagnosis of hEDS needs the simultaneous presence of all criteria, 1 and 2 and 3.
The various criteria are divided into three categories. The first category is looking at generalized joint hypermobility using the Beighton Scale. The second category is a set of criteria further divided into categories A, B, and C in which two of the following features must be present. The third category is a list of prerequisites all of which must be met.
Those with HSD may not present much differently than someone with hEDS, but they do not meet hEDS criteria and their symptoms cannot be explained by another disorder.
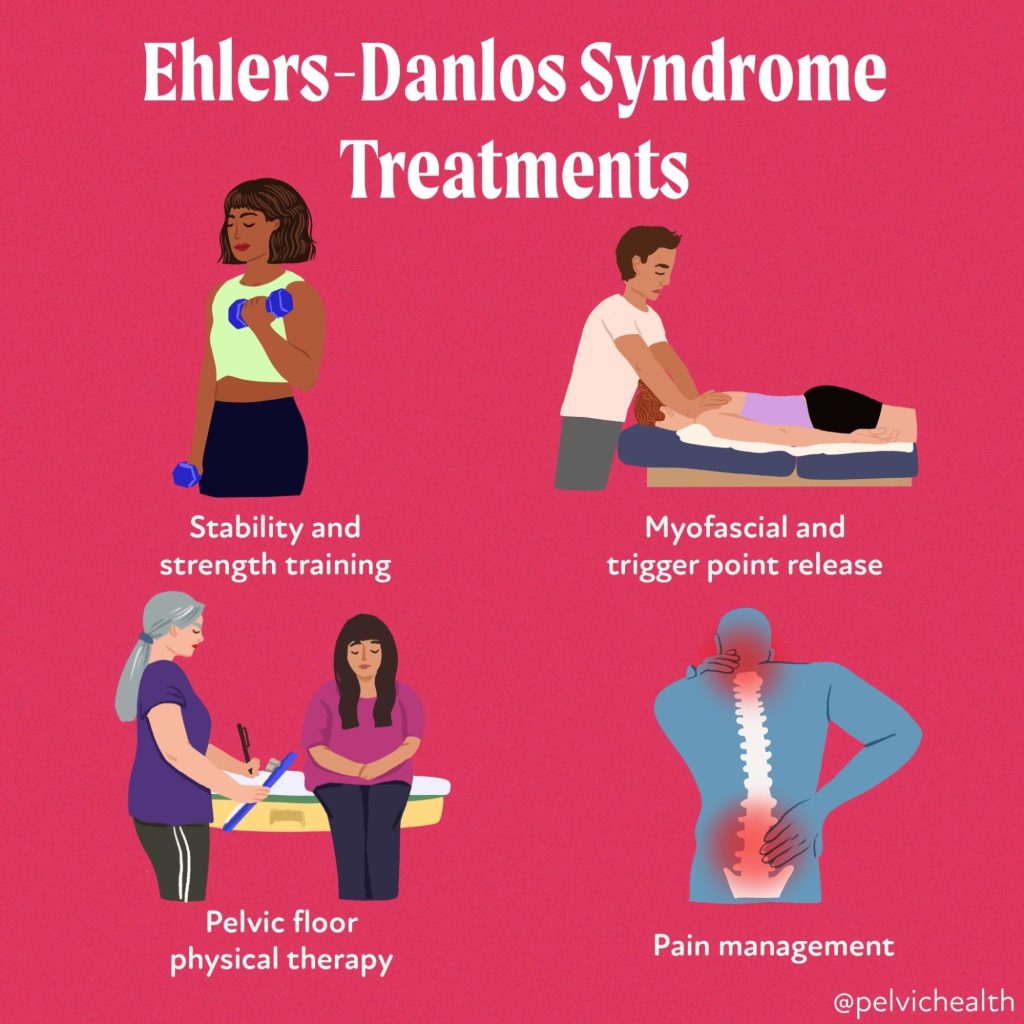
How PHRC and Pelvic Floor Therapy Can Help with hEDS and HSD
Pelvic floor therapy is more than just exercise, it’s hands-on, expert care for the muscles, nerves, and tissues of the pelvic region. While individuals suffering from hEDS and HSD absolutely need to strengthen, hands-on work is often necessary. Determining when and how we use these tools is very important for those with hEDS and HSD. At PHRC, we’re trained to understand how all of the various pieces of the puzzle (symptoms) are connected and interact to cause pain, dysfunction, and disruption in your life.
Pelvic floor therapy for patients with hEDS and HSD requires a highly nuanced and individualized approach. Our evaluations include a comprehensive assessment that considers the patient’s full medical history, comorbidities, trauma background, and current functional status. Our evaluations and follow-up sessions are one-on-one with your therapist, allowing adequate time to focus on the various problems you are experiencing.
Our work focuses on:
- Manual therapy directed towards restrictions in the fascial and muscular system impacting the pelvic floor along with proper strengthening and stabilization techniques
- Addressing posture and movement patterns that may be worsening symptoms
- Progressive strengthening and stabilization exercises
- Gradual functional retraining
- Teaching you how to manage flares and avoid triggers
- Education, tools, and resources that can help you in your day to day tasks to avoid fatigue and flare-ups
- Collaborating with your other healthcare providers (like pelvic pain specialists, allergists, or endometriosis surgeons)
Our therapists recognize that many people suffering with hEDS and HSD have experienced significant invalidation and gaslighting. Our team recognizes and uses a trauma based approach ensuring you feel safe and supported. Another aspect PHRC prides itself on is our collaborative approach with a team of providers, coordinating care with various specialists to help our patients reduce this load as it can be extremely burdensome, but can greatly enhance therapy outcomes.
Conclusion
Living with EDS can be exhausting, frustrating, and isolating. For many patients, it takes years to receive a diagnosis, during which time symptoms often progress and impact multiple areas of life, including relationships, self-image, and daily functioning.
It’s important for both patients and providers to understand that healing is not linear. There will be ups and downs, flare-ups, and good days. The key is consistency, education, and compassionate support.
Support groups, patient advocacy organizations, and mental health counseling can all play a role in sustaining patients emotionally as they navigate the chronic nature of EDS. Pelvic floor therapists can act not only as clinicians but as advocates and allies in their patients’ health journeys.
If you’re living with Ehlers-Danlos Syndrome and struggling with pelvic symptoms, know that help is available. Pelvic floor therapy is a compassionate, personalized, and effective path to better pelvic health—and a better quality of life.
If you’ve been diagnosed or suspect you have hEDS or HSD and have been struggling with pelvic pain, painful sex, or other pelvic floor dysfunction, don’t give up. We understand and we can help. At the Pelvic Health and Rehabilitation Center, we offer both in-person physical and occupational therapy in the Bay Area, Southern California, and New England, as well as virtual consults. If you are struggling with finding help, please reach out or visit our website for more information.
To read more about EDS and HSD, diagnosis, treatments and related information, this article from the NIH gives a good overview.
Resources:
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
Emerging Perspectives on Chronic Pelvic Pain and Sexual Health
By Jandra Mueller, DPT, MS, PHRC Encinitas
Last fall (2024), I attended a mast cell conference where my colleague Alyssa Yee, MD and I were invited to speak about the topic of pelvic pain conditions and the role of mast cells; specifically on the topic of endometriosis and neuroproliferative vestibulodynia (NPV) – a specific type of vestibulodynia characterized by excessive nerve endings and mast cells. Over the last few years, sexual medicine and pelvic health providers have been hard at work researching the involvement mast cells play in some of these more difficult, and very painful conditions causing debilitating pelvic pain and sexual dysfunction.
If you’re one of the many individuals dealing with chronic pelvic pain, painful periods, or discomfort with intimacy, you’re not alone—and you’re not imagining it. These symptoms are common, but they’re often misunderstood, misdiagnosed, or minimized. New research and clinical observations are shedding light on an overlooked contributor to this pain: mast cells.
In this blog, we’ll explore what mast cells are, how they relate to conditions like endometriosis and vestibulodynia, and why understanding their role could be the key to better diagnosis and treatment for many people, and ultimately, better treatment options.
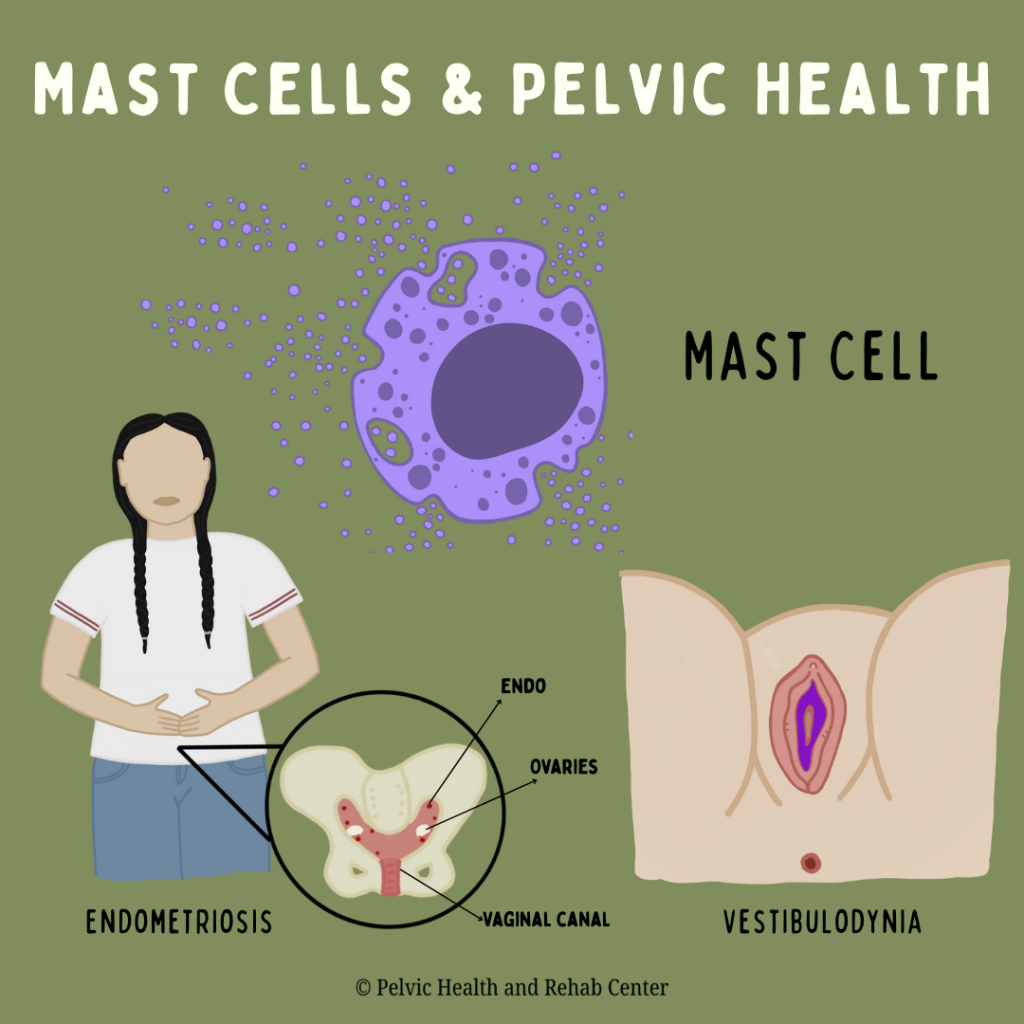
What Are Mast Cells?
Mast cells are part of your immune system. Mast cells are commonly found in tissues that have exposure to the outside environment like the respiratory system, the gut, the genitourinary tract, our skin, and our connective tissue. When a substance comes into contact with a mast cell, the mast cell may be triggered and release a variety of substances like histamine, leukotrienes, and tryptase (and many, many more) in response to these triggers. Most people associate them with allergies, but recent findings show that mast cells can also play a role in chronic inflammation, pain, and even tissue remodeling.
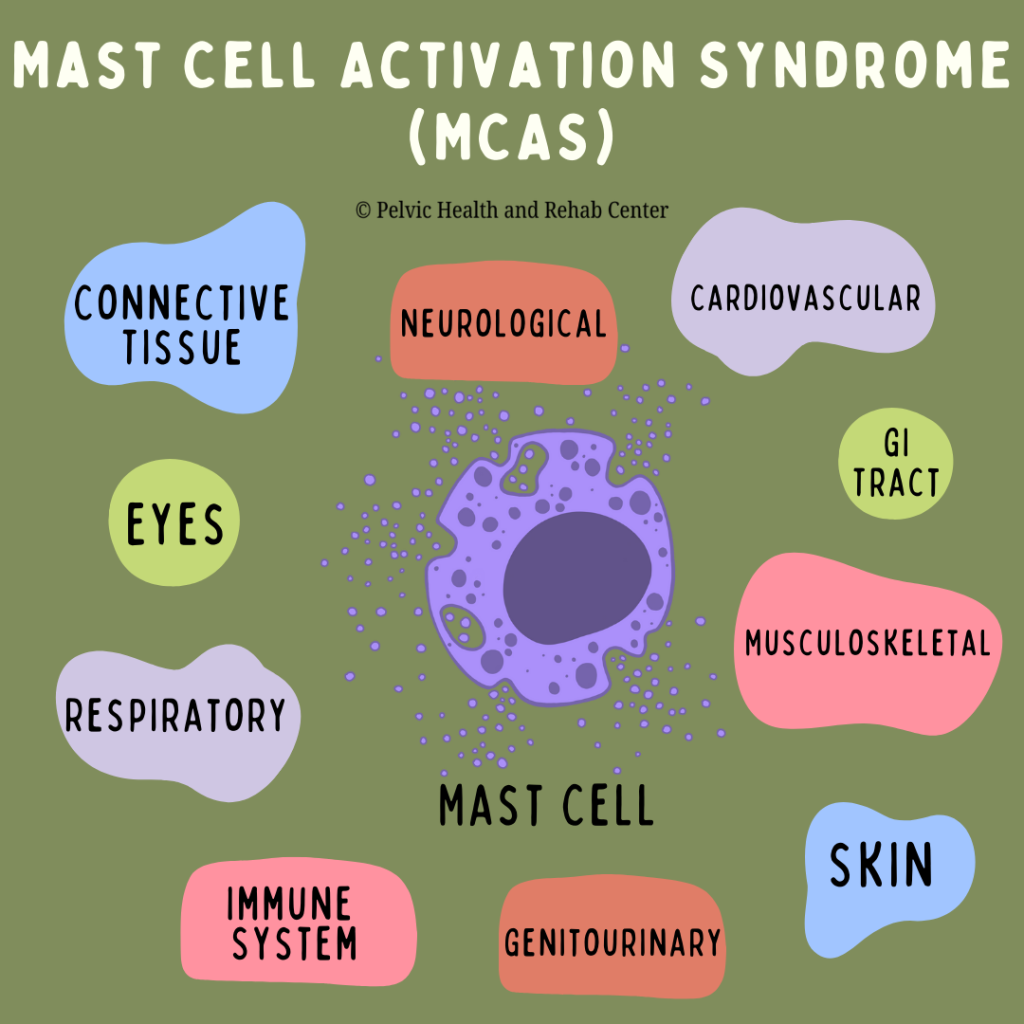
What is Mast Cell Activation Syndrome?
Mast cell activation syndrome is a condition where mast cells become over reactive and inappropriately release too many of their mediators (often inflammatory) and typically involve a wide range of symptoms and typically involve multiple body systems. This syndrome was defined and distinguished from a more rare condition, mastocytosis (increased number of mast cells) and allergic reactions.
Mast Cells and the Body Systems They Affect
A very thorough article by Dr. Lawrence Afrin and colleagues (2020) reviewed the diagnosis of MCAS, and we’ve summarized various symptoms specific to each body system below. Mast cell activation syndrome (MCAS) can affect nearly every organ system in the body. Chronic activation of mast cells results in a wide range of symptoms, making the condition hard to identify. Here are some of the key systems impacted:
- Skin: Flushing, itching, rashes, dermatographism (skin writing), and hives.
- Eyes: Irritated or often dry eyes, episodic difficulty focusing, lid tremors/tic
- Gastrointestinal: Nausea, abdominal pain, bloating, reflux, constipation, or diarrhea.
- Genitourinary: Bladder pain, urinary frequency, interstitial cystitis, vaginal pain (vulvodynia), and menstrual irregularities.
- Neurological: Headaches, dizziness, nerve pain, brain fog, memory issues, and sensory hypersensitivities.
- Cardiovascular: Heart palpitations, blood pressure swings, and lightheadedness or fainting.
- Respiratory: Shortness of breath, wheezing, cough, and sinus congestion.
- Musculoskeletal/Connective tissue: Muscle and joint pain, hypermobility (especially in conditions like Ehlers-Danlos Syndrome).
- Endocrine and Immune: Hormonal imbalances, thyroid dysfunction, and increased susceptibility to allergies and infections, hypersensitivity reactions, impaired healing
Understanding this broad impact helps explain why so many patients experience a long diagnostic journey—MCAS often mimics or overlaps with many other disorders.
Mast Cells, MCAS, and Pelvic Pain
Many people with chronic pelvic pain have conditions such as endometriosis, irritable bowel syndrome (IBS), vulvodynia, or painful sex (dyspareunia). While each of these conditions has its own unique features, what they often have in common is inflammation (and pelvic floor dysfunction!)—and for some people, mast cells may be a key factor in driving this inflammation.
A few years ago, Dr. Paul Yong, a sexual medicine OBGYN and researcher, presented a novel concept: Neuroproliferative Dyspareunia. Based on his research, he compared endometriosis and neuroproliferative vestibulodynia, demonstrating similarities in demographics, inflammatory factors, and the role of mast cells. In addition to the work of Dr. Irwin Goldstein and colleagues in NPV pathology over the last few years, along with many of us seeing individuals presenting with both endometriosis and NPV, further research to support Dr. Yong’s theory has begun; looking at both the pathology of the endometriosis lesions and vestibule in individuals with both conditions.
Let’s break it down with two key conditions where mast cells are now being studied more closely: endometriosis and vestibulodynia.
Endometriosis and Mast Cells
Endometriosis is a condition where tissue similar to the lining of the uterus grows on tissues and organs throughout the abdominopelvic cavity as well as distant sites throughout the body. These lesions have many different appearances, are often innervated, and respond to hormones which lead to inflammation, scarring, and pain.
A study by McCallion et al. (2022) demonstrates that endometriosis lesions can actually attract mast cells. These mast cells then release inflammatory substances that contribute to the pain and worsen the disease. In fact, mast cells and estrogen appear to work together, creating an environment that supports ongoing inflammation and nerve growth—both major sources of pain.
This means treatments that only target hormones (like birth control) might miss a key piece of the puzzle. Addressing immune and inflammatory responses, including mast cell activity, could offer new relief.
Vestibulodynia and Mast Cells
Vestibulodynia is simply defined as pain at the entrance of the vagina, often described as burning, stinging, or sharp discomfort, especially with touch, tampon use, or intercourse. Many people are told “nothing is wrong” or are misdiagnosed for years.
There are several causes and associated factors related to vestibulodynia, often related to a reduction in hormones from the use of birth control pills or certain stages of life such as menopause and breastfeeding. Another type is neuroproliferative vestibulodynia, either lifelong or acquired, that does not necessarily involve hormones. Neuroproliferative vestibulodynia is characterized by:
- Higher nerve density in the vulvar tissue (more nerves = more pain signals).
- Increased mast cells in the tissue, contributing to both inflammation and nerve growth.
This is not psychological—it’s a real biological process that can be seen under a microscope.
Why It Matters: A New Way to Look at Old Problems
Traditionally, pelvic pain has been explained through hysteria, psychological blocks, trauma, hormones or mechanical issues. Patients were often told to ‘it’s all in your head’ or to just manage their pain with birth control, surgery, or even a hysterectomy. While there may be a role for some of these interventions in certain cases, they don’t address the underlying immune system activity—like the involvement of mast cells.
By understanding that mast cells are active in both endometriosis and vestibulodynia, along with a wide range of symptoms in patients with chronic pelvic pain, our hope is that more research results in more understanding and more treatment options.
Chronic pelvic pain is rarely caused by a single issue. It often involves the immune system, neuromuscular system, hormones, and emotional well-being. That’s why the best care usually includes a team approach and persistence.
How PHRC and Pelvic Floor Physical and Occupational Therapy Can Help with Mast Cell-Mediated Pelvic Pain
If you’ve been dealing with ongoing pelvic pain, painful sex, bladder discomfort, or vulvar burning, and haven’t gotten clear answers, you’re not alone. At the Pelvic Health and Rehabilitation Center (PHRC), we specialize in helping people with complex pelvic pain.
Pelvic floor physical and occupational therapy (PFPT) is more than just exercise, it’s hands-on, expert care for the muscles, nerves, and tissues of the pelvic region. At PHRC, we’re trained to understand how all of these pieces are connected and interact to cause pain and disrupt your life. Conditions that are mediated or impacted by mast cells aren’t new to us, but our understanding of the condition is constantly evolving.
Our work focuses on:
- Manual therapy directed towards restrictions in the fascial and muscular system impacting the pelvic floor
- Calming down overactive nerves and reducing pain signals
- Improving blood flow and tissue healing
- Teaching you how to manage flares and avoid triggers
- Addressing posture and movement patterns that may be worsening symptoms
- Collaborating with your other healthcare providers (like pelvic pain specialists, allergists, or endometriosis surgeons)
Our evaluations and follow-up sessions are an hour long, one-on-one with an actual physical and occupational therapists – no aides or assistants, and very comprehensive.
Our therapists are very familiar with the very complex cases and diagnoses, not only are we trained to help address the myofascial implications, we can help screen for, and direct you, to the various professionals that can help with medical management.
Even if your condition hasn’t been formally diagnosed, we can help you start feeling better through targeted pelvic floor therapy and whole-body strategies; we will also help to facilitate the appropriate referrals and can provide helpful resources. We understand that seeing provider after provider is overwhelming and exhausting. We work with an extensive network of specialists and can help you navigate this journey, get a proper diagnosis, and an effective treatment plan.
If you’ve been struggling with pelvic pain, painful sex, or unrelenting vulvar discomfort and haven’t found relief, don’t give up. There is growing awareness and research into mast cell-mediated pain, and perhaps mast cells will be a key factor in managing some of these more complex conditions. We understand and we can help. At the Pelvic Health and Rehabilitation Center, we offer both in-person physical and occupational therapy in the Bay Area, Southern California, and New England, as well as virtual consults. If you are struggling with finding help, please reach out or visit our website for more information.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: immune cells, mast cell mediators, blood vessels, mature mast cells, other immune cells,