Have you been experiencing testicular pain? Most men don’t realize that testicular pain can be caused by pelvic floor dysfunction, nerve irritation in the lower back, or issues with circulation. Unfortunately, testicular pain is often misdiagnosed as prostatitis, and many men are unnecessarily prescribed antibiotics. Oftentimes, antibiotics are not the solution. Instead, pelvic floor physical and occupational therapy can help to eliminate muscular impairments, improve pelvic floor and core coordination, and reduce dysfunction to treat testicular pain.
What are the Causes of Testicular Pain?
There are several potential causes of testicular pain, three of which are related to lumbar pathology, vascular pathology, and pelvic floor pathology.
- Lumbar pathology: The nerves that supply the testicles start in the lower back. If a disc bulges, or arthritis develops, or a lumbar nerve gets irritated, the pain can travel down and feel like it’s in the testicle even though the source is the spine
- Vascular pathology: PProblems with blood flow, like enlarged veins (known as varicoceles), twisting of the blood supply (known as torsion), or congestion in the vessels, can create aching, heaviness, or sharp pain in the testicle
- Pelvic floor pathology: The pelvic floor muscles act like a hammock under the pelvis. If they get tight, weak, or spasm, they can irritate nerves and cause pain that feels like it’s inside the testicle even though the muscles are the source
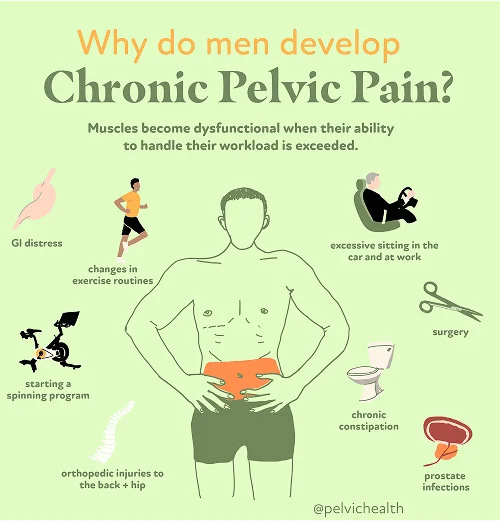
Additional causes of testicular pain can include:
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting
- Chronic constipation and straining
- Jelqing and/or attempts at gential enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
- The majority of men with pelvic pain (including testicular pain), with or without urinary or bowel complaints, have pelvic floor dysfunction
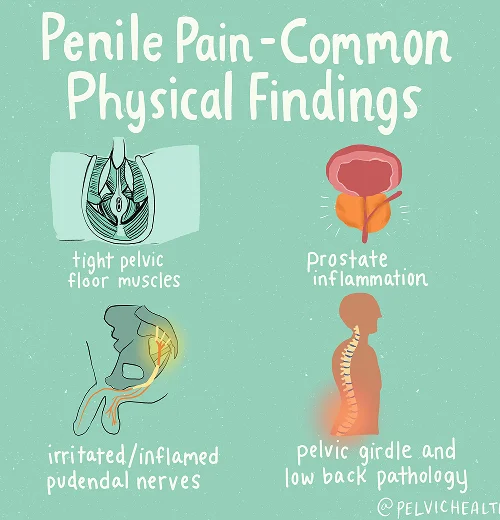

Symptoms of Testicular Pain
- Burning, aching, itching of the testicles
- These symptoms can also occur in the penis, scrotum, perineal, and/or anal area
In addition to testicular pain, many men also experience a combination of the below symptoms:
- Men suffering from pelvic pain often times experience pain caused by sitting, certain types of exercises, and certain types of clothing
- In addition to pelvic pain, men often experience urinary urgency/frequency/hesitancy as well as pain and slower / diminished urinary stream
- With pelvic pain, men may have discomfort in their penis, scrotum, and perinea upon ejaculation
- Some men experience signs of erectile dysfunction, accompanied by reduced ejaculation strength.
- Men may endure gastrointestinal distress, bloating, and/or constipation
- Symptoms of GI distress can be aggravated by actions like ejaculation or exercise, or unprovoked and spontaneous
- Men may experience these symptoms intermittently or constantly
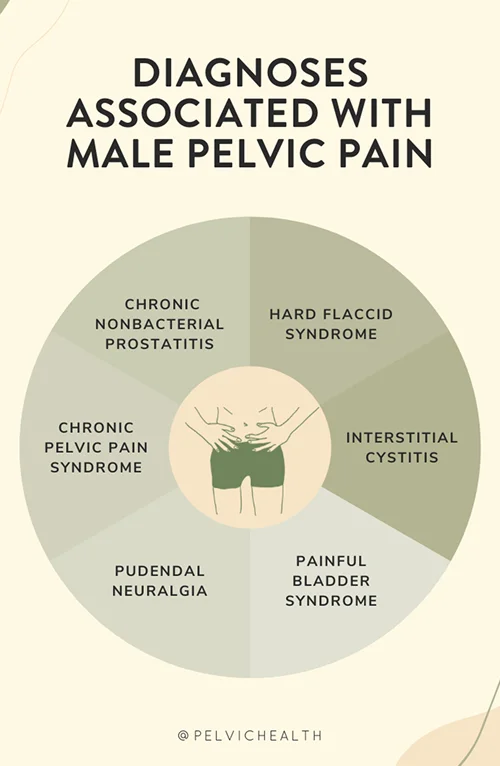
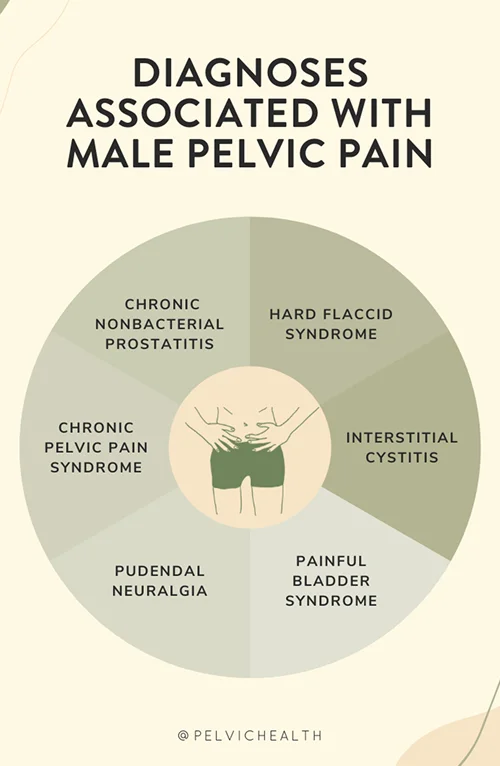
Associated Diagnoses
Lumbar, vascular, and pelvic floor pathologies can all connect to recognized diagnoses of testicular and pelvic pain. Lumbar pathology may appear as lumbar radiculopathy or referred pain from disc injury and arthritis in the lower back. Vascular pathology includes conditions such as varicocele, testicular torsion, or pelvic venous congestion, where altered blood flow creates pain signals. Pelvic floor pathology is most closely tied to Chronic Pelvic Pain Syndrome (CPPS), pudendal neuralgia, hard flaccid syndrome, and painful bladder syndrome. In many cases, pelvic floor dysfunction acts as the underlying link, either driving the pain directly or amplifying symptoms from other systems.
Diagnostic Challenges
Men who experience testicular pain are often misdiagnosed with prostatitis and prescribed antibiotics, even in the absence of infection. Research consistently shows that more than 90% of men with pelvic or genitourinary pain symptoms do not have a bacterial prostate infection.
Instead, they typically fall into the National Institutes of Health categories IIIa and IIIb, grouped under Chronic Pelvic Pain Syndrome (CPPS). Lumbar and vascular contributors can further complicate diagnosis, as they can mimic the presentation of pelvic floor dysfunction. This overlap frequently leads to delays in identifying the true source of pain and in receiving effective treatment.
The National Institute of Health Classification of prostatitis syndromes are:
- Category I: Acute bacterial prostatitis which is associated with severe prostatitis symptoms, systemic infection and acute bacterial urinary tract infection.
- Category II: Chronic bacterial prostatitis which is caused by chronic bacterial infection of the prostate with or without prostatitis symptoms and usually with recurrent urinary tract infections caused by the same bacterial strain
- Category IIIa: Inflammatory chronic pelvic pain syndrome (white blood cells in semen and/or expressed prostatic secretions and/or third midstream bladder specimen)
- Category IIIb: Noninflammatory chronic pelvic pain syndrome (no white blood cells in semen and/or expressed prostatic secretions)
- Category IV: Asymptomatic inflammatory prostatitis which is categorized by prostate inflammation in the absence of genitourinary tract symptoms
The National Institute of Health Classification of prostatitis syndromes are:
- Category I: Acute bacterial prostatitis which is associated with severe prostatitis symptoms, systemic infection and acute bacterial urinary tract infection.
- Category II: Chronic bacterial prostatitis which is caused by chronic bacterial infection of the prostate with or without prostatitis symptoms and usually with recurrent urinary tract infections caused by the same bacterial strain
- Category IIIa: Inflammatory chronic pelvic pain syndrome (white blood cells in semen and/or expressed prostatic secretions and/or third midstream bladder specimen)
- Category IIIb: Noninflammatory chronic pelvic pain syndrome (no white blood cells in semen and/or expressed prostatic secretions)
- Category IV: Asymptomatic inflammatory prostatitis which is categorized by prostate inflammation in the absence of genitourinary tract symptoms
Treatment for Testicular Pain
Depending on the cause of your symptoms (whether it’s tight/overactive pelvic floor muscles, nerve irritation, or blood flow issues), your treatment can include:
- Pelvic floor physical and occupational therapy for pelvic floor dysfunction: Helps release the tight muscles, retrain coordination, and calm any nerve irritation in the pelvis
- Spine and back treatment: Physical and occupational therapy, posture work, and sometimes injections if nerve irritation in the lumbar spine is the source of the testicular pain
- Vascular-related treatment: Pelvic floor physical and occupational therapy can reduce muscle guarding, improve circulation through posture and breathing techniques, and reduce pressure on congested veins
- Addressing biomechanical issues: Physical and occupational therapy and exercises to improve hip function, mobility, and body mechanics when structural problems contribut
- Lifestyle adjustments: Managing constipation, limiting prolonged sitting, and gradually returning to exercise to reduce pelvic strain
How We Can Help You with Testicular Pain
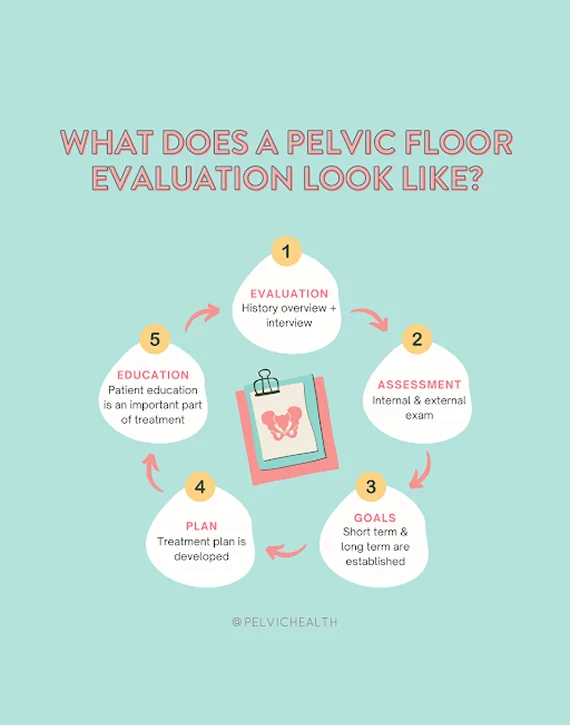
Men experiencing testicular pain can benefit from an evaluation with a pelvic floor physical and occupational therapist specializing in pelvic pain. During your evaluation at PHRC, the pelvic floor physical and occupational therapist reviews your history and symptoms with you, what you have been diagnosed with in the past, the treatments you have undergone and how effective or not effective these treatments have been.
We understand what you have been going through and that most men are very frustrated by the time they see us.
During your physical examination the pelvic floor physical and occupational therapist examines muscles, tissues, joints, nerves, and your movement patterns. Once your pelvic floor physical and occupational therapist completes the examination they review your findings with you. The physical and occupational therapist creates an assessment which explains how you developed pain and creates short and long-term goals for your treatment plan.
How We Can Help You with Testicular Pain
Men experiencing testicular pain can benefit from an evaluation with a pelvic floor physical and occupational therapist specializing in pelvic pain. During your evaluation at PHRC, the pelvic floor physical and occupational therapist reviews your history and symptoms with you, what you have been diagnosed with in the past, the treatments you have undergone and how effective or not effective these treatments have been.
We understand what you have been going through and that most men are very frustrated by the time they see us.
During your physical examination the pelvic floor physical and occupational therapist examines muscles, tissues, joints, nerves, and your movement patterns. Once your pelvic floor physical and occupational therapist completes the examination they review your findings with you. The physical and occupational therapist creates an assessment which explains how you developed pain and creates short and long-term goals for your treatment plan.
Typically, the frequency of pelvic floor physical and occupational therapy treatment is one to two times per week for roughly 12 weeks. You are given a home exercise program to complement your in-person sessions, and your pelvic floor physical and occupational therapist will help to coordinate your recovery with the other members of your treatment team. We are here to help you recover and finally get relief from your symptoms.
