By Jandra Mueller, DPT, MS, PHRC Encinitas
March is Endometriosis Awareness Month, AND National Nutrition Month – what a great time to talk about how optimal gut health and nutrition impacts endometriosis. Optimal gut health and nutrition play a crucial role in one’s endometriosis journey because having a healthy gut means improving our mental health, optimizing our immune system, nourishing our bodies AND can have impacts in how this disease progresses. YES, gut health actually plays a role in the pathogenesis of this disease. Endometriosis is known by most as a hormonal and gynecological disease; however, this perspective is slowly shifting and is now being looked at as an inflammatory or immune related disease. This means that we potentially will have new treatments, and maybe new ways of diagnosing this disease, in a more comprehensive way. As of now, excision surgery is the gold standard for both diagnosis and treatment, and will likely still remain a critical part of treating this disease. However, I’m sure many endo sufferers know that surgery alone has not necessarily helped with all the ‘other’ endo symptoms like fatigue, IBS, and chronic pain.
What is endometriosis?
Endometriosis is endometrial-like tissue, found outside of the uterus most commonly in the abdomino-pelvic cavity, that can become problematic. Most commonly, it is known to cause painful periods (dysmenorrhea) and play a role in those suffering from infertility. However, there are many many more symptoms and conditions that are associated with endometriosis and guess what, not all people with endo have painful periods, high estrogen, or suffer from infertility! This is why endometriosis can be so hard to diagnose and treatment can be tricky.
Facts about endo
-
- It is estimated that one in ten women* have endometriosis. However, those that are familiar with endo may say this number is actually low. *I use the term ‘women’ because that is what is published in literature; however, it is understood that those biologically born as female, with female anatomy, may not identify under that term. Those that identify as male, non-binary, transgender, and intersex are absolutely not excluded from this statistic!
- Average delay of diagnosis is seven to ten years.
- Those with a family history have a significantly higher risk for developing endometriosis.
-
- There is no predisposition based on race or socioeconomic status. However, people of color may be underrepresented because of the impact of systemic racism in our society leading to more mis-diagnoses, under or inadequate treatment, and inaccuracies in pain perception resulting in more hysterectomies and inadequate pain reduction interventions.
- Stage of disease is NOT correlated with symptom severity.
In 2017 there was a NEW theory proposed called “The Bacterial Contamination Theory,” which talks about the role of the gut bacteria and overall gut health in the progression of this disease. Until recently, there were many theories proposed which have been found to be somewhat true, but also have been disproven. We believe that depending on the person, all theories may actually have some merit. Mostly, these theories at best tell us why the lesions are there in the first place, but they do not help to understand how this cell progresses into endometrial-like tissue, implants itself and invades into the surrounding tissues, establishes its own nerve and blood vessel supply, or causes clinical symptoms. This new theory is a step in the right direction to help understand this on a deeper level.
The Bacterial Contamination Theory of Development: A New Concept in Endometriosis
To understand this, it is helpful to understand a little bit of background information about the gut. Our gut contains a ton of bacteria, it is estimated that there are more bacteria in our gut than cells we have that make us human. They play vital roles in our health and can be impacted in many ways including our diets, exposure to medications such as antibiotics, stress, and chronic illness to name a few. When these bacteria become out of balance, it is called dysbiosis. This just means that they are no longer balanced, we have some bacteria that may be really high, and some that may be really low. They are all important and play a role in our health, but need to be in balance. In those with endometriosis, it is estimated that 90% have IBS, or at least GI symptoms, the most common being bloating, followed by changes in bowel movements (diarrhea, constipation, or both).
This theory explains that certain bacteria, specifically gram-negative bacteria, can release a toxic called lipopolysaccharide which, in normal circumstances, is not an issue. You have other gut bugs that help to keep this in check. However, when you have less of the good bugs, and a high number of these bacteria, this is when things become problematic. These gram-negative bacteria are more likely to be resistant to antibiotics, so, if you’ve had to take antibiotics for UTIs, colds, sinus infections, or anything else, this impacts the state of your gut health. When this balance is disrupted, and there are high levels of this toxin in the gut, they are able to travel outside the gut and into places in our bodies where they are not supposed to be, and cause problems. This can also be due to intestinal permeability issues or ‘leaky gut’ which is also common in those with endo.
When LPS is present (in the gut or outside the gut), they activate our immune system, increase production of different growth factors and inflammatory mediators (called cytokines) further inflammation so that our body can help fight this ‘pathogen.’ It ultimately becomes a positive feedback loop. This toxin and these growth factors have been shown to trigger the change in the cell type and promote the growth and implantation of these cells, and help them to escape clearance from our own immune system. They essentially sneak past our immune system and create a home for themselves in our tissues where they go on to create a blood supply and nerve supply to survive and cause pain, among other issues.
These bacteria are also found in the gential tract and can migrate upwards towards the uterus, and during menstruation, can be refluxed out of the uterus into the abdominopelvic cavity, which may become problematic. If we think about Sampon’s theory of retrograde menstruation, which is the most well known theory to date, although disproved because it has been shown that 90% of women experience retrograde menstruation, yet only 10% have endo, this starts to make more sense. Bacteria is refluxed during menstruation, and those with various genetic factors, high gut inflammation, hormonal imbalances, now have the right environment to allow the immune system to ignore the mess that is going on, and the disease is now present and can become problematic.
The result of high LPS in the abdominopelvic cavity causes something called oxidative stress. Oxidative stress is where there are a lot of free radicals compared to antioxidants in our body, and this can result in changes to our DNA promoting inflammation and disease. It is not a coincidence that the majority of women with endo have GI symptoms, and that this is a huge area that is not being adequately addressed in this population.
Another recent article from 2019 looked at the gut microbiome in those with endometriosis and supported this theory. In those with endo, it was seen that the group of gram-negative bacteria was significantly higher than those without endometriosis, and the group of beneficial bacteria was lower. The overall conclusion was that a dysfunctional immune system, caused by significant gut dysbiosis has some evidence that the microbiome modulates the immune system response leading to endometriosis causing escape from our immune system, and promotes the progression of this disease.
Overall, these new studies and evidence to fill in the gaps of what is currently known is very promising for this community. For years, endometriosis has been thought of as a hormonal or gynecological disease with surgery as the cornerstone of treatment, and hormonal suppression as the ‘best’ treatment to help manage symptoms. With this new perspective, this opens doors for new treatments, that may be superior and actually TREAT this disease instead of just suppressing hormones causing a myriad of other problems. It is well known, even when looking at this new theory, that hormonal balance plays a key role in mediating this disease, but it is only part of the picture.
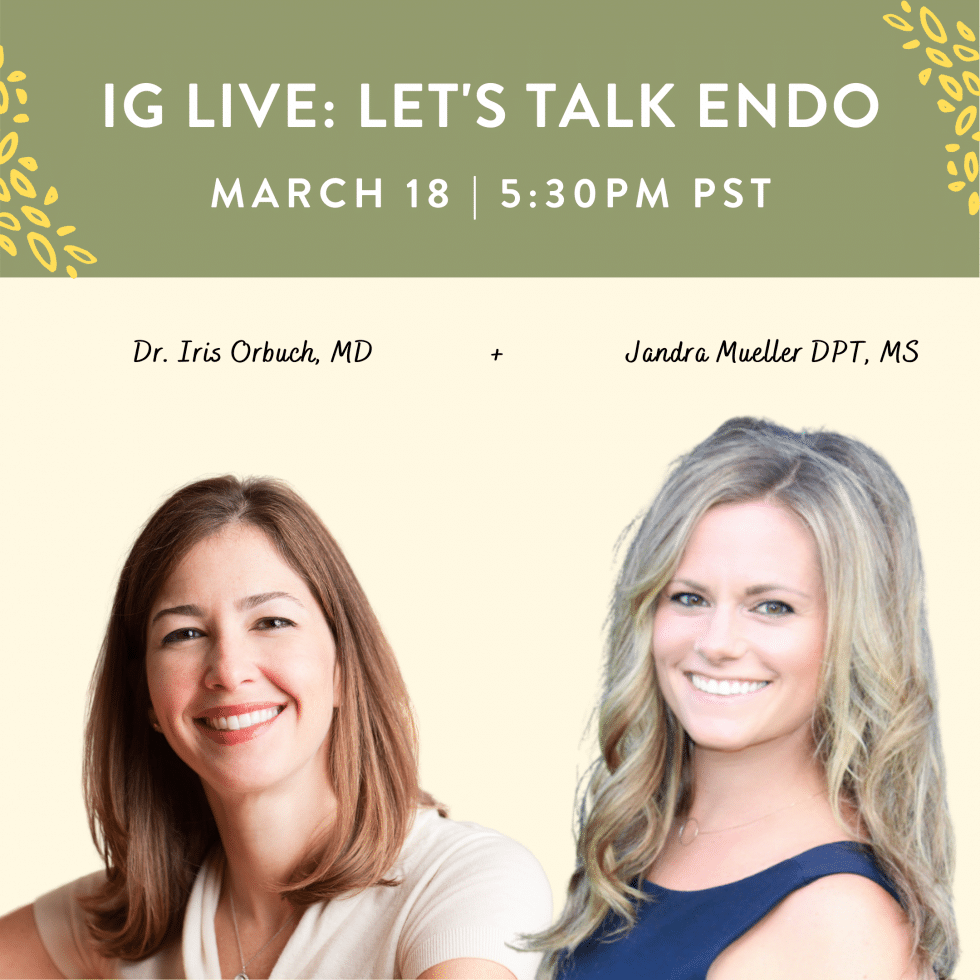
Working with endometriosis experts is a key to getting an adequate diagnosis and proper treatment for this disease. I have the pleasure of speaking with Iris Kerin Orbuch, MD on this topic and answering all of your questions this month on our IG live.
Dr. Iris Kerin Orbuch is the Director of the Advanced Gynecologic Laparoscopy Center in Los Angeles and author of Beating Endo How to Reclaim Your Life From Endometriosis.

A preview of the book via audio sample is available from HarperCollins Publishers.
She sees the value in addressing endometriosis, an inflammatory disease, via eastern and western approaches. The cornerstone of endometriosis treatment is surgical excision of endometriosis, though she understands the importance of incorporating integrative medicine and combining eastern & western medicine approaches in helping her patients heal and getting them on the road to recovery. She understands that endometriosis is a major reason women experience pain, though she strives to assess for all additional co-existing generators of pain in order to help women live pain free productive lives.
Her training, under the guidance of Dr. C.Y. Liu and Dr. Harry Reich — both pioneers in the field of advanced laparoscopic surgery — allows Dr. Orbuch to be one of a handful of physicians across the country trained to perform advanced minimally invasive procedures. Dr. Orbuch provides both compassionate and individualized care while performing advanced laparoscopic techniques at St. John’s Hospital in Santa Monica, California. Dr. Orbuch is board certified in OB/GYN.
Dr. Orbuch offers Gentle, Compassionate Care and a Personal Touch. When you visit her office, you won’t find a rushed, impersonal environment. Instead, Dr. Orbuch and her staff are committed to providing personal, compassionate services to each and every client. Dr. Orbuch is devoted to helping women live a productive and pain-free life.
If you missed it, you can watch the entire IG live on our Instagram!
For additional resources, Lj Powerhouse and Jandra Mueller, DPT, MS hosted an endo live answering many common questions. For more information and resources on endometriosis read our Pelvic Pain Explained: Endometriosis blog.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual physical therapy appointments too!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical therapists committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical therapists, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical therapist who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
PHRC is also offering individualized movement sessions, hosted by Karah Charette, DPT. Karah is a pelvic floor physical therapist at the Berkeley and San Francisco locations. She is certified in classical mat and reformer Pilates, as well as a registered 200 hour Ashtanga Vinyasa yoga teacher. There are 30 min and 60 min sessions options where you can: (1) Consult on what type of Pilates or yoga class would be appropriate to participate in (2) Review ways to modify poses to fit your individual needs and (3) Create a synthesis of your home exercise program into a movement flow. To schedule a 1-on-1 appointment call us at (510) 922-9836
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Like us on Facebook,
Subscribe to our YouTube Channel,
and follow us on Twitter, Instagram, Tik Tok and Pinterest!