Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

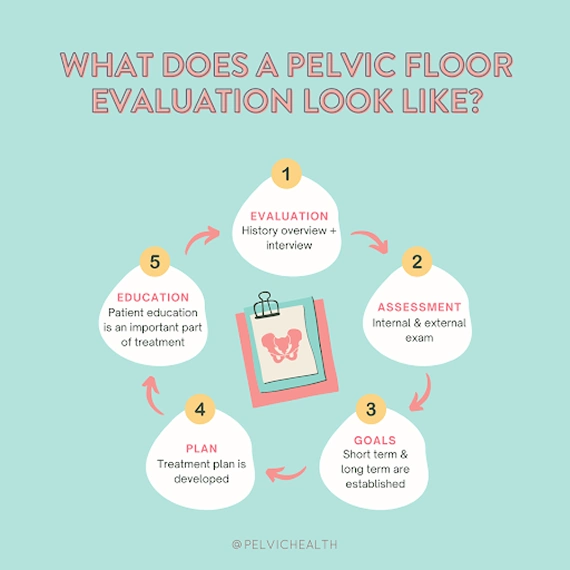
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
The male pelvic floor supports important functions like your core, urination, bowel movements, and sexual performance, but it rarely gets any attention until something feels off. Even then, many cases are misdiagnosed as prostatitis. For many men, symptoms like groin pain, urinary urgency, genital pain, post-ejaculatory pain or trouble with erections come as a surprise—and are often hard to talk about.
This guide focuses on everything you need to know about pelvic floor dysfunction in men and the treatment available.
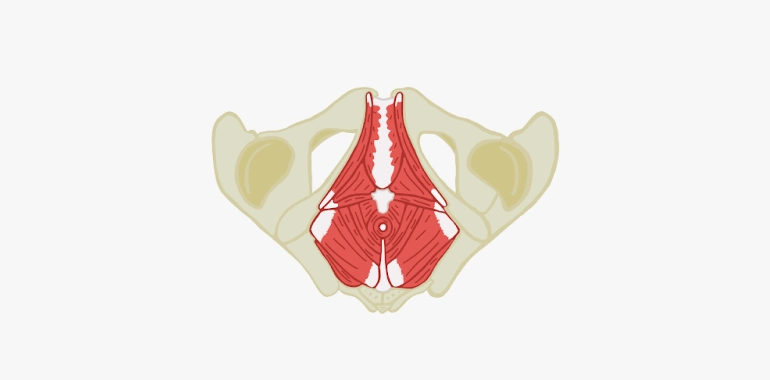
Male Pelvic Floor Anatomy and Physiology
The male pelvic floor is a group of muscles, ligaments, and connective tissue that form a supportive sling at the base of the pelvis. These muscles stretch from the pubic bone to the tailbone and play an important role in bladder and bowel control, sexual function, and core stability. The pelvic floor works together with the deep abdominal and back muscles to support the pelvic organs, including the bladder, rectum, and prostate.
Pelvic floor dysfunction in men happens when these muscles become too tight, too weak, or lose coordination. This can lead to a range of symptoms such as urinary leakage, frequent urination, constipation, erectile dysfunction, or pain in the pelvis, genitals, or rectum. Sometimes the muscles spasm or stay contracted, which can make the symptoms worse over time.
Understanding the anatomy of the pelvic floor helps explain how dysfunction in this area can affect many different parts of daily life.
The pelvic floor muscles are innervated by the pudendal nerve, the levator ani nerve and sacral nerve roots. These muscles are under voluntary and involuntary control and are never fully at rest, making them unique and different from all of our other muscles in our body.
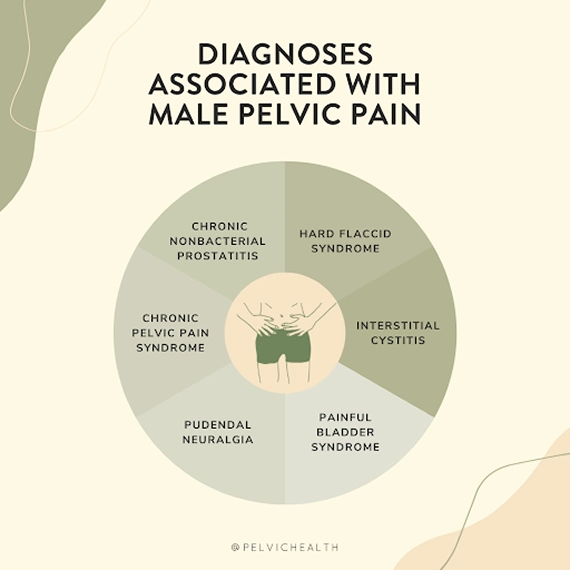
Diagnostic Challenges and Categories
Research shows 10% of men experience pelvic pain at some point in their lives that is caused by pelvic floor dysfunction. However, many of these individuals are misdiagnosed and mistakenly prescribed antibiotics for what they believe is prostatitis, and experts believe the prevalence is actually higher than 10%. However, the majority of men diagnosed with prostatitis do not have prostatitis. Many urologists prescribe men antibiotics without even testing. And if they do test, they tend to still prescribe antibiotics even if the cultures are negative because medical schools do not include training on pelvic floor dysfunction and, therefore, general urologists are often unaware that pelvic floor dysfunction exists.
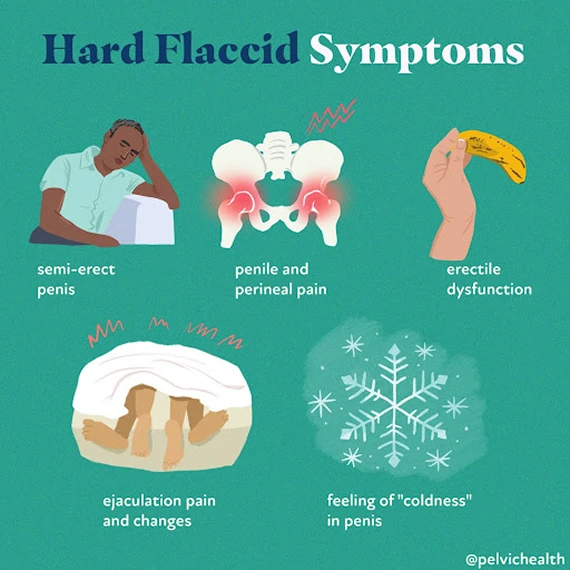
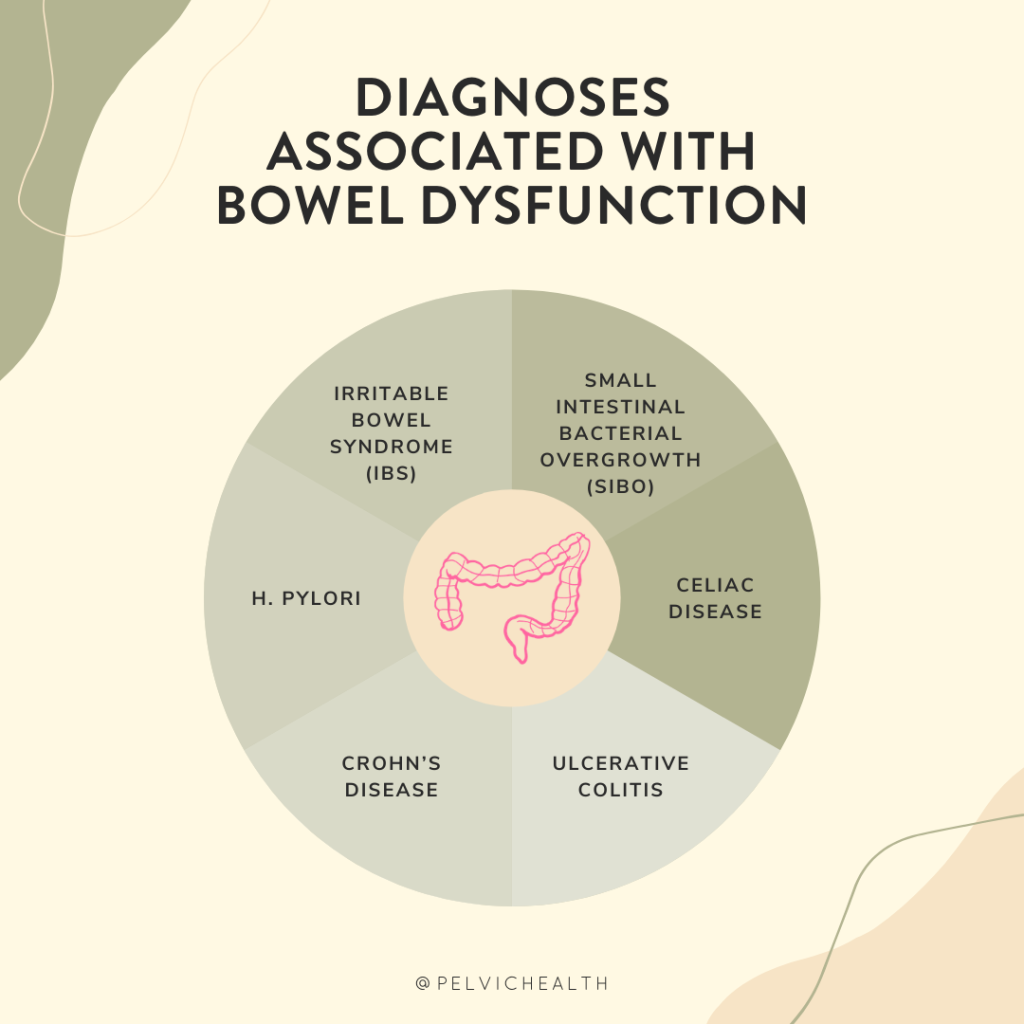
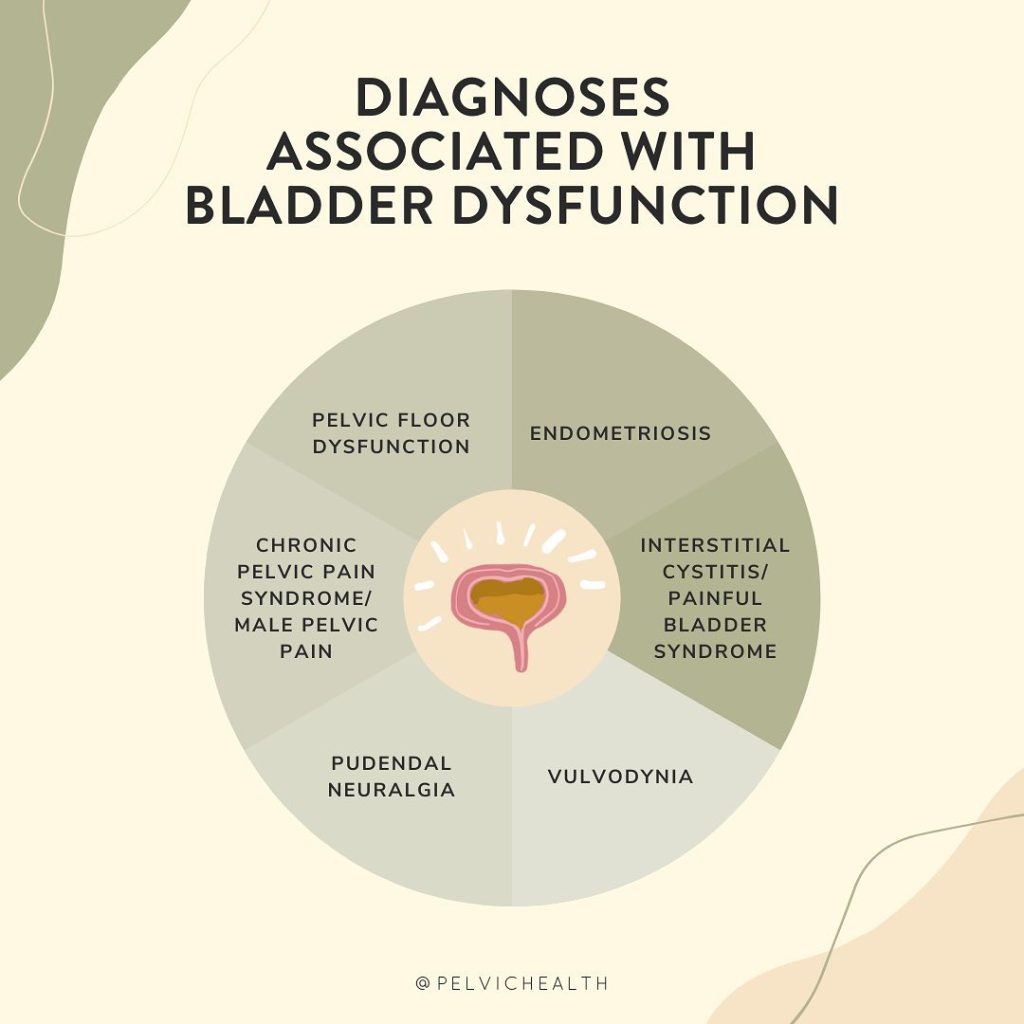
Pelvic pain syndromes such as Chronic Pelvic Pain Syndrome/Male Pelvic Pain, Pudendal Neuralgia, Hard Flaccid Syndrome, and Interstitial Cystitis/Painful Bladder Syndrome are all associated with dysfunction in the pelvic floor, resulting in persistent discomfort and/or urinary, bowel, and sexual dysfunction.
Studies indicate that men with pelvic pain may take up to seven years to receive an accurate diagnosis. This prolonged diagnostic journey is attributed to the fact that the symptoms of male pelvic pain closely resemble those of prostate, bladder, and/or sexually transmitted infections.
Adding to the complexity, numerous pelvic floor physical and occupational therapistss are primarily trained to treat women. However, at PHRC, this is not the case. In fact, there are some days where we treat more men than women.
The key to addressing this issue lies in targeted physical and occupational therapy aimed at strengthening the pelvic floor muscles rather than relying on ineffective antibiotics.
Symptoms of Male Pelvic Floor Dysfunction
Pelvic floor dysfunction in men can manifest in a range of symptoms, which generally fall into four categories: urinary, bowel, sexual dysfunction, and pelvic floor/girdle/trunk/lower extremity pain.
- 1. Urinary Symptoms
- Frequent urge to urinate with little output
- Hesitancy or difficulty starting urine stream
- Feeling incomplete bladder emptying after urinating
- Burning or pain during or after urination
- Dribbling urine after finishing urination
- 2. Bowel Symptoms
- Constipation and/or straining during bowel movements
- Incomplete bowel emptying sensation
- Pain before, during, or after bowel movements
- Urgency or frequent need to have a bowel movement
- Need for excessive toilet paper
- Leakage of stool or gas
- 3. Sexual Symptoms
- Pain during or after ejaculation
- Erectile dysfunction or difficulty maintaining an erection
- Testicular pain or aching
- Penile or perineal pain with arousal or sexual activity
- Decreased sensation or numbness during sex
- 4. Pelvic Floor, Girdle, Trunk, and Lower Extremity Pain
- Pain in the perineum or sit bones
- Lower abdominal or groin pain
- Tailbone or coccyx pain when sitting
- Hip, lower back, or sacroiliac joint pain
- Inner thigh or pelvic floor muscle tightness
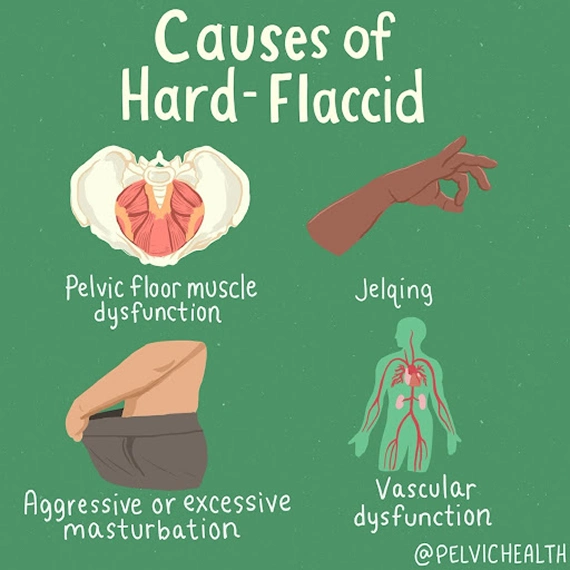
Causes of Male Pelvic Floor Dysfunction
Men can develop pelvic floor dysfunction for many reasons, including the below:
- Surgical trauma (vasectomy, benign prostatic hyperplasia (BPH) interventions, prostatectomy)
- Orthopedic injuries or other traumas (spine, hip, knee, and/or ankle injuries/pathology, accidents)
- Biomechanical or structural dysfunction (hip dysfunction, piriformis syndrome, scoliosis, leg length discrepancy)
- Excessive exercise or changes to exercise routine
- Excessive sitting or sitting changes involving car changes, office changes
- Chronic constipation and straining
- Jelqing and/or attempts at genital enhancement or foreskin regeneration
- In rare cases, bladder, prostate, or sexually transmitted infections after successful resolution of infection
Many men who experience pelvic pain, with or without issues related to urination or digestion, often have pelvic floor dysfunction.
Learn more about Pelvic Floor Dysfunction
Treatment for Male Pelvic Floor Dysfunction
Pelvic floor dysfunction in men is treated through a combination of in-person physical and occupational therapy sessions and a personalized home exercise program. Treatment focuses on addressing muscle tension, weakness, or coordination issues that contribute to symptoms like pelvic pain, urinary problems, and sexual dysfunction. Techniques might include manual therapy, targeted exercises, relaxation strategies, and education on posture and movement patterns, often combined with collaboration from other healthcare providers to support your recovery.
Why PHRC and What To Expect at Your First Appointment
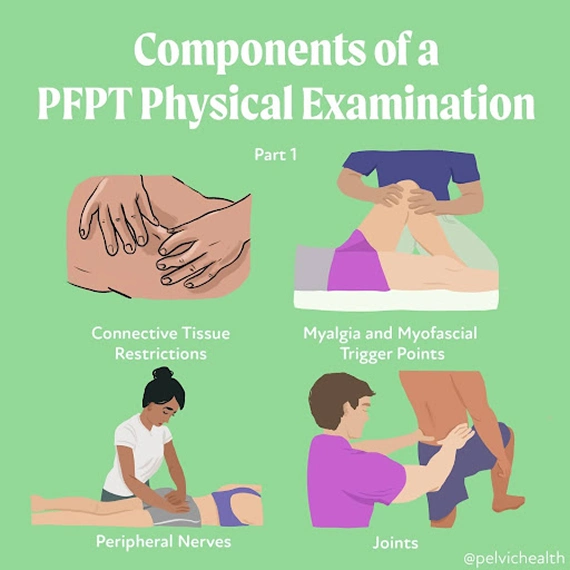
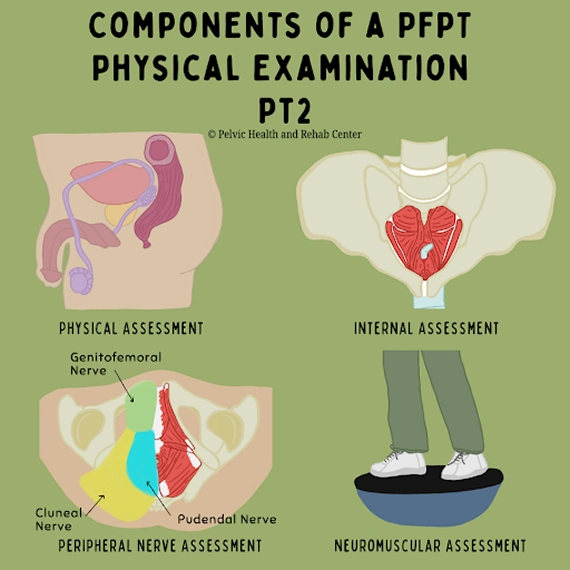
When you arrive for your first appointment at PHRC, the primary goal is to understand your pelvic health concerns in detail. During this initial consultation, your therapist will ask about your medical history, including any past pelvic surgeries, chronic conditions, or injuries that might contribute to symptoms like urinary issues, bowel dysfunction, sexual pain, or lower extremity pain. This conversation helps guide the best approach for your care.
A physical assessment will follow, where your physical and occupational therapists evaluates the muscles, tissues, and nerves in your pelvic region. This exam may include checking for muscle tightness, weakness, or imbalances that could be affecting your pelvic floor function. Your therapist also looks at how well your muscles coordinate during movement, which plays a role in bladder and bowel control, sexual function, and core stability.
Once the assessment is complete, your physical and occupational therapists will create a personalized treatment plan based on your specific symptoms. This plan might include exercises to relax or strengthen your pelvic floor muscles, manual therapy to release tension, or other techniques designed to target your needs. For example, if you’re dealing with urinary leakage, your therapist might focus on muscle coordination and bladder retraining. If bowel issues are present, strategies to improve control and relaxation will be part of your care.
Your treatment plan will also include a home exercise program to support your recovery between sessions. These exercises, along with regular appointments, help you regain control of your pelvic floor function and reduce pain or discomfort.
We make sure you feel supported throughout your recovery and coordinate care with any other healthcare providers involved in your treatment.
Find Relief from PHRC
At PHRC, our goal is to provide compassionate and comprehensive care to help you manage and overcome pain from pelvic floor dysfunction. By understanding the underlying causes and providing targeted treatments, our goal is to improve your quality of life and restore your health.
We also recognize the challenges some people might face in accessing in-person care, which is why we offer virtual sessions through telehealth after your initial consultation. These sessions allow for continuity of care and accessibility for those unable to travel to one of our clinics.
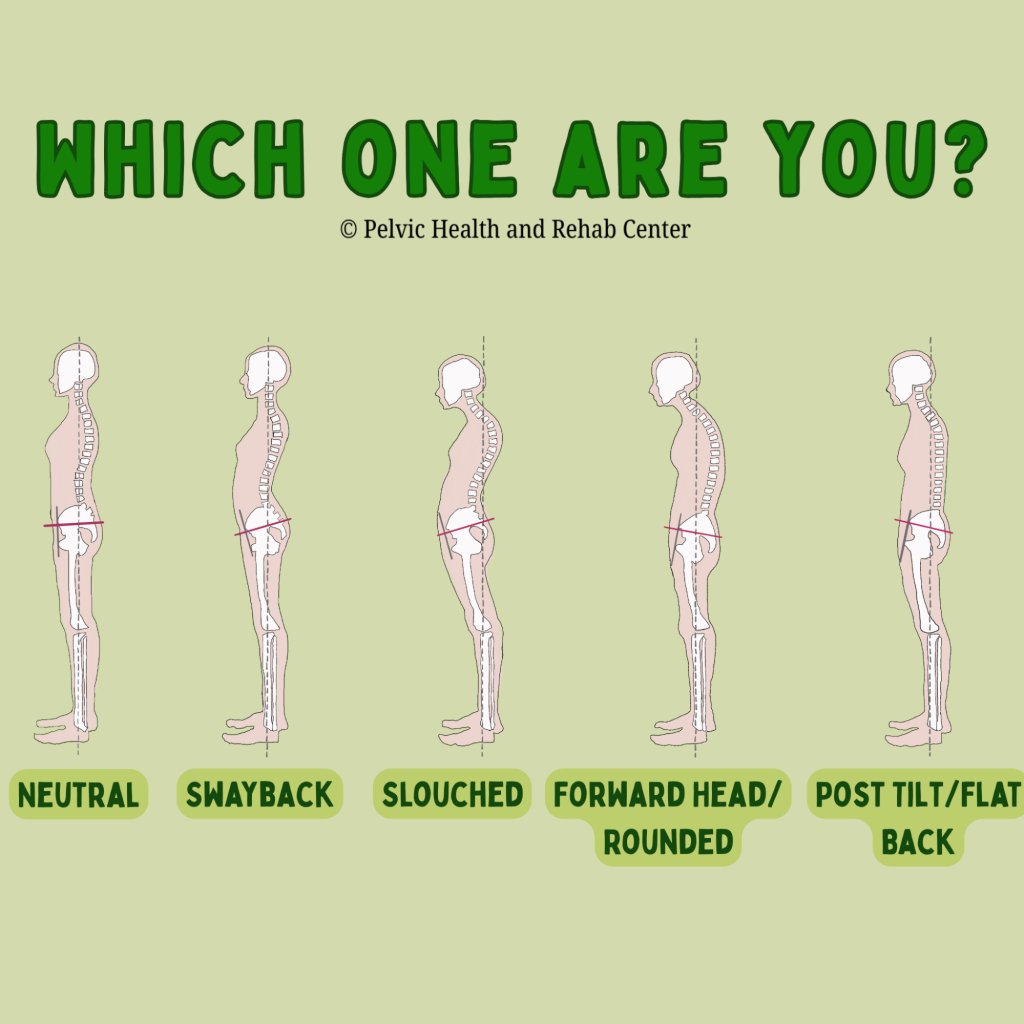
Why Does Our Posture Matter for Our Pelvic Health?
By Jandra Mueller, DPT, MS, PHRC Encinitas
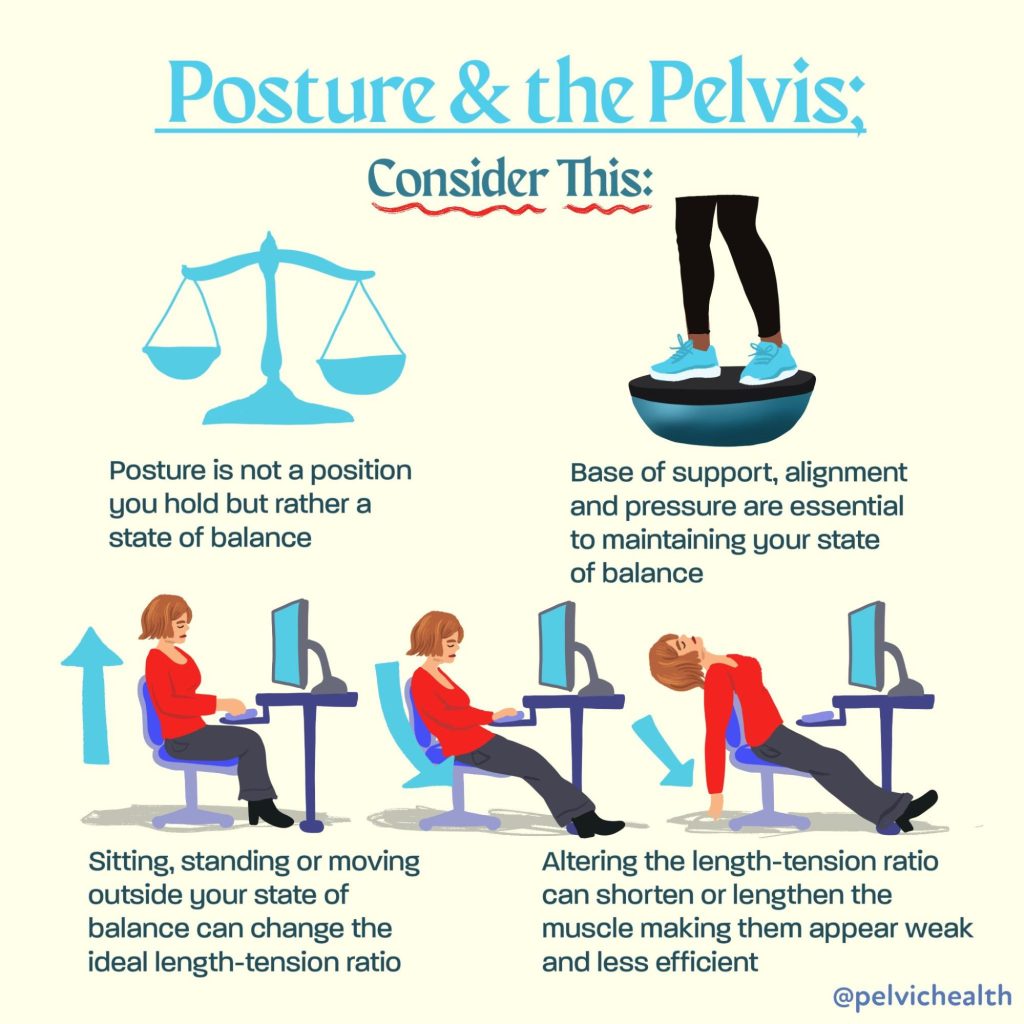
When we think about our posture, we often think “mine can be better” and we picture sitting up straight or avoiding slouching to prevent back or neck pain. Usually these corrections last a few minutes until we find ourselves slumped back over our computer or realizing our back is hurting from standing for so long. Aside from keeping us upright, our posture plays a crucial role in how our pelvic floor functions. In fact, a growing body of research reveals a clear connection between postural alignment and pelvic floor muscle activity, with significant implications for maintaining continence, providing support for our pelvic organs, and our overall core stability.
Physical and occupational therapists are great at looking at someone’s posture, and it’s so engrained in our professions that our observations begin immediately and at some point during the course of therapy, we will dive into it. Whether it’s addressing how you are sleeping, holding your baby, lifting boxes, sitting at your desk for work or standing in line at the grocery store – your posture impacts your body and your pelvic health.
So, how exactly does posture affect the pelvic floor? Let’s take a look at the evidence.
Understanding the Postural-Pelvic Floor Connection
The pelvic floor muscles (PFMs) don’t work in isolation. They are part of a complex system involving the diaphragm, abdominal muscles, and spinal stabilizers—all of which are influenced by posture. When our posture is compromised, so is the efficiency and coordination of this core system.
A 2022 study by Kwak et al. titled “Posture Correction Therapy and Pelvic Floor Muscle Function Assessed by sEMG with Intravaginal Electrode and Manometry in Females with Urinary Incontinence” showed that posture correction had a direct impact on pelvic floor function. Specifically, women who received postural correction therapy demonstrated significant improvements in pelvic floor muscle strength and coordination, as measured by both surface EMG and intravaginal manometry.
Additional research performed by physical and occupational therapistss Chehrehrazi & Nourbakhsh published in the Journal of Women’s & Pelvic Health Physical and Occupational Therapy (2024) demonstrated the impact of a specific pelvic corrective exercise on the impact of pelvic floor muscle (PFM) contractions. In this double blinded randomized study, the authors evaluated 30 individuals who demonstrated pelvic asymmetries and randomized them into two groups: pelvic repositioning exercise group and a control group. They found statistically significant improvements in PFM contractions after the pelvic repositioning exercise group, but not in the control group. This study demonstrates that neuromuscular exercises aimed at improving proper joint alignment and positioning impacts the function and strength of the pelvic floor muscles.
Key takeaway:
Posture correction improved pelvic floor contractility and function and contributed to symptom relief in women with urinary incontinence.
How Posture Influences Pelvic Floor Activity
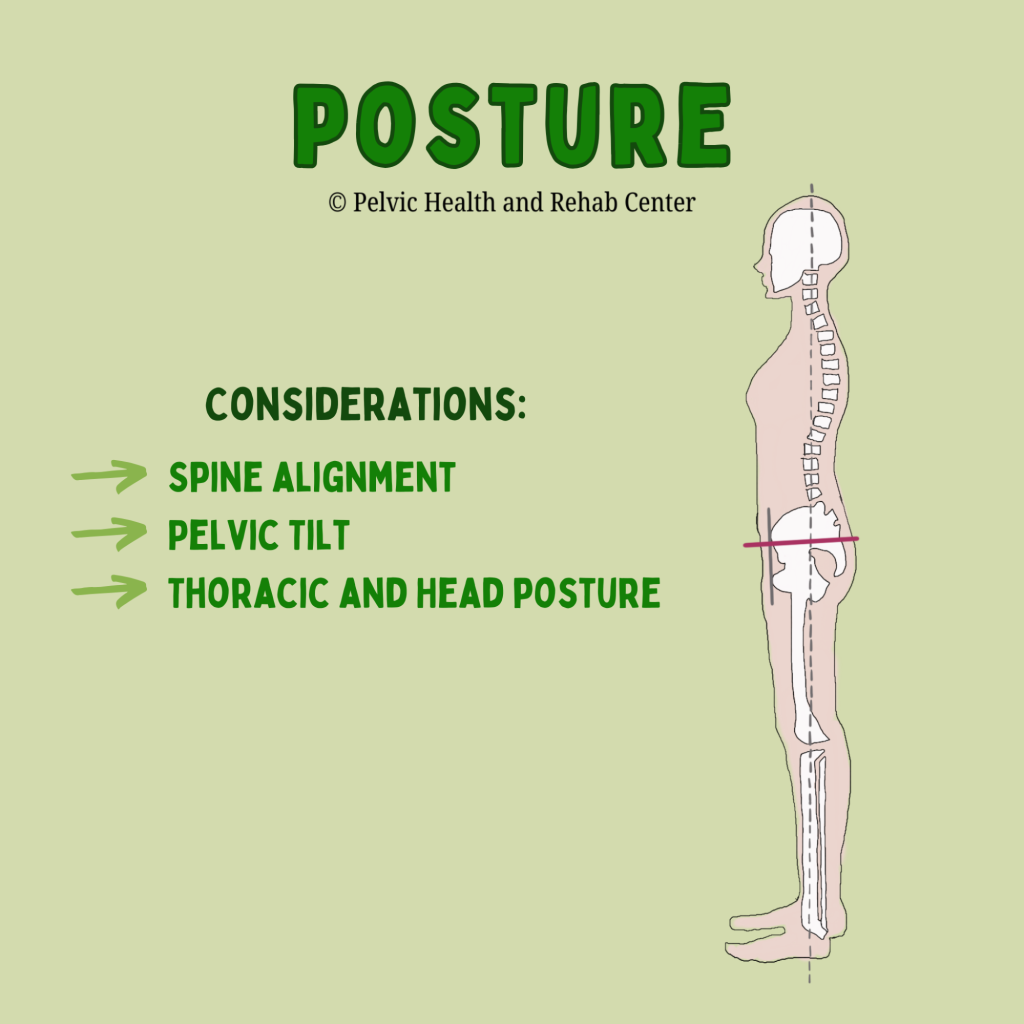
Research reviewed by Capson et al. (2020) in “Are There Any Relations Between Posture and Pelvic Floor Disorders?” highlights several postural factors that influence pelvic floor muscle dynamics furthering our understanding of how the pelvic floor does not work in isolation:
Lumbar spine alignment:
Increased lumbar lordosis (swayback) can increase intra-abdominal pressure, which places more strain on the pelvic floor. Conversely, a flattened lumbar curve may reduce the pelvic floor’s ability to contract effectively.
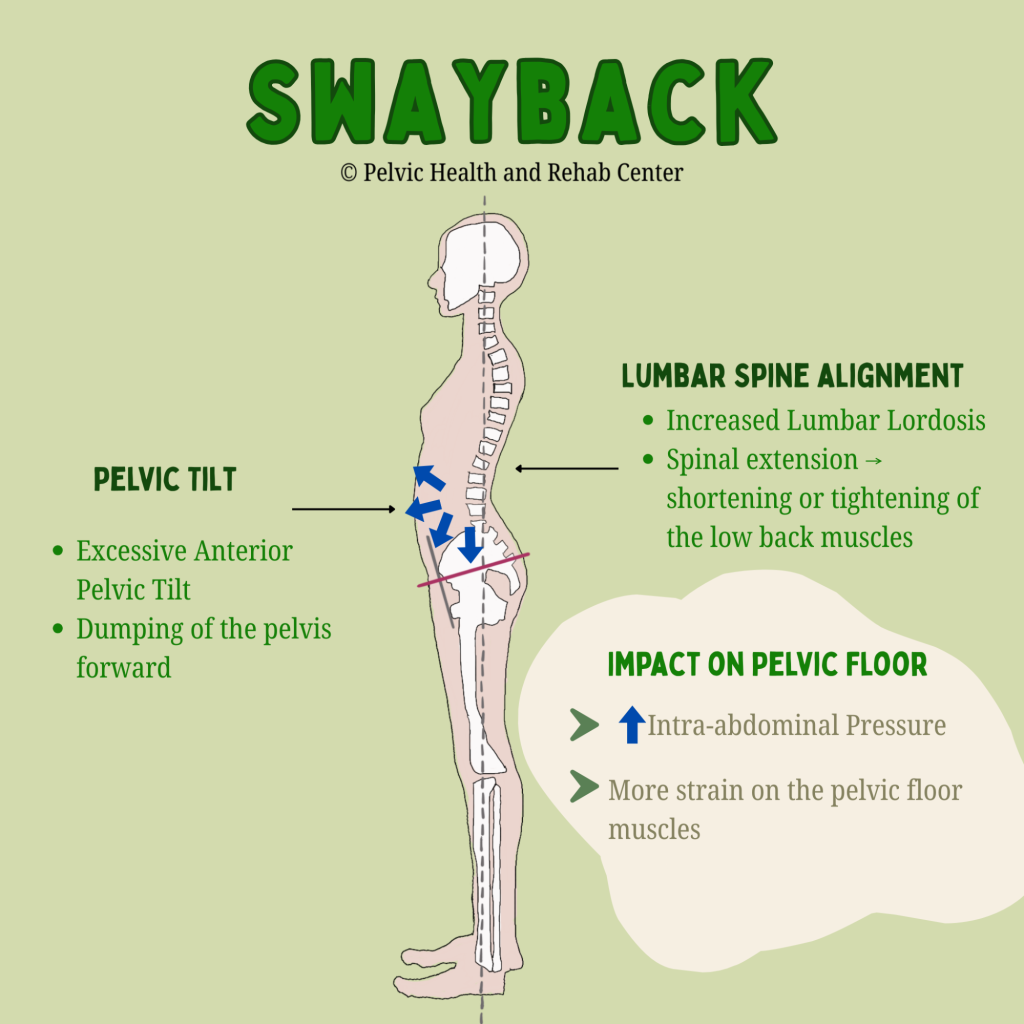
An anterior pelvic tilt often goes hand-in-hand with a swayback posture and contributes to poor core engagement and increased downward pressure on the pelvic organs. A posterior pelvic tilt, such as with a flattened lumbar spine, may reduce optimal positioning of the pelvic floor for contraction and relaxation.
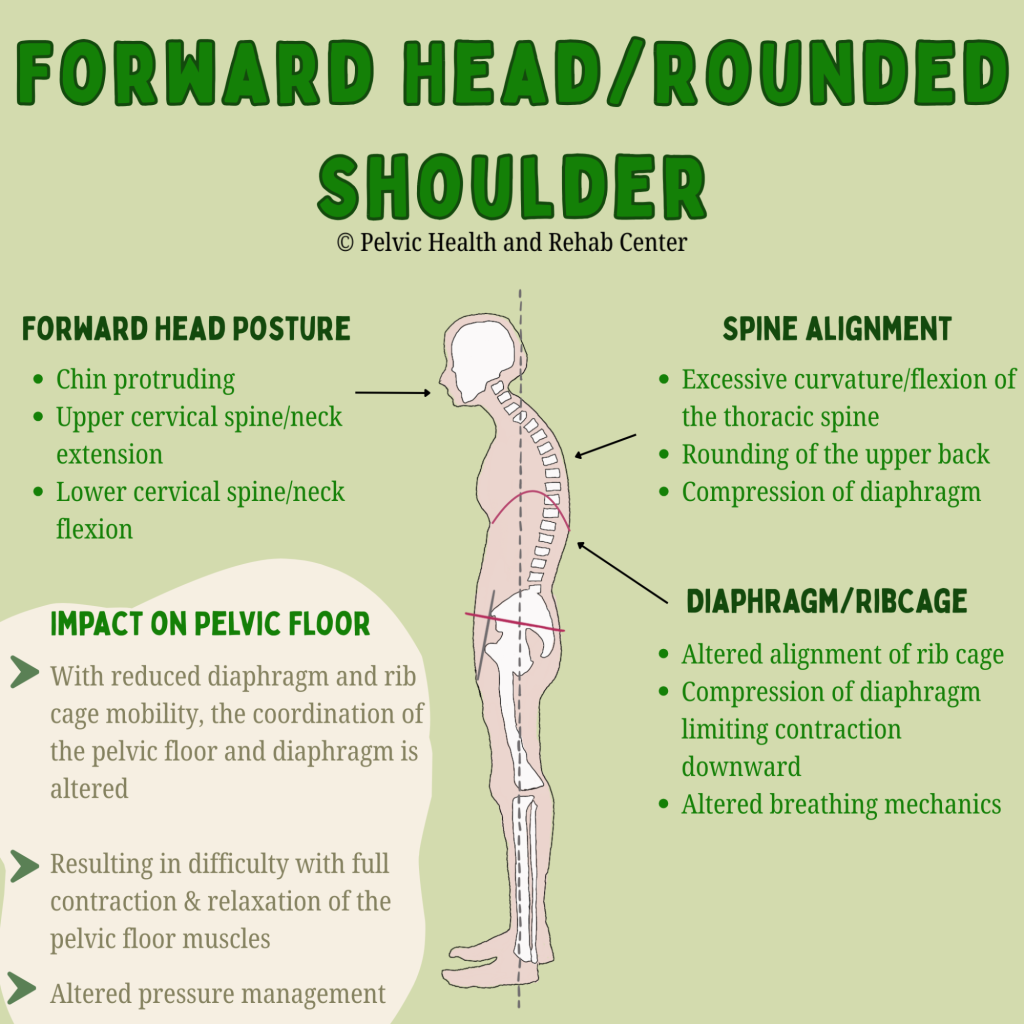
Thoracic and head posture:
Forward head posture and thoracic kyphosis (rounded upper back) can disrupt the alignment of the rib cage and pelvis, altering breathing mechanics and decreasing the coordination between the diaphragm and pelvic floor.
In short, poor posture can disrupt the natural synergy between the diaphragm, abdominal wall, and pelvic floor, making it harder for these muscles to work together efficiently. Conversely, improving your posture can have immediate effects on muscle function.
Posture and Pelvic Floor Dysfunction: What the Research Shows
Several studies cited in Capson et al.’s review found that individuals with pelvic organ prolapse or urinary incontinence often exhibited altered postural patterns, including exaggerated lumbar curves and pelvic tilting. While not all studies show a direct causal relationship, the evidence supports a strong association between poor posture and increased pelvic floor dysfunction risk.
One standout study included in the review used MRI imaging to assess postural effects on pelvic organs and showed that altered alignment of the spine and pelvis led to measurable changes in pelvic organ position—a likely contributing factor to prolapse and urinary leakage.
Many patients seeking pelvic floor therapy ask “how did this happen?” Many times there is not an event or injury that immediately started their symptoms, more often than not it was a gradual build up and then a triggering event and our job is to help identify the various impairments and provide a treatment plan, which includes identifying factors that ultimately contributed to one’s symptoms in the first place.
Can Improving Posture Help Pelvic Floor Dysfunction?
As therapists, the answer is a no brainer – absolutely! Research also suggests that improving one’s posture can help improve pelvic floor dysfunction. The 2022 Kwak study is particularly compelling. After just eight weeks of posture correction therapy—including targeted stretching and strengthening exercises—participants experienced:
- Improved alignment in spinal and pelvic posture
- Increased pelvic floor muscle strength and endurance
- Decreased urinary leakage
These findings suggest that postural correction can be an effective and non-invasive component of pelvic floor rehabilitation, especially for individuals with incontinence or organ prolapse.
Why Posture Shouldn’t Be Overlooked
While many individuals dealing with pelvic floor dysfunction benefit from manual therapy techniques, pelvic floor tools, and exercises directed at the pelvic floor muscles, in the bigger picture, we have to also look at the whole system to better understand what factors are contributing to and keeping these muscles dysfunctional. Therefore, providers who are treating pelvic floor disorders, assessing posture should be a fundamental part of any evaluation and treatment plan. It’s not just about aesthetics or spinal health—it’s about optimizing the interconnectedness of the neuromusculoskeletal and visceral systems.
Key clinical considerations:
- Evaluate standing and sitting posture, including spinal curves and pelvic alignment.
- Ask about specific postures that are problematic or your patient is needing to achieve throughout their day.
- Incorporate postural retraining, core stabilization, and breathing techniques into treatment.
- Educate patients on the impact of alignment on pelvic floor health/pelvic pain
Bottom Line: Alignment Matters
The relationship between posture and pelvic floor function is clear: good (posture) alignment sets the stage for efficient pelvic floor engagement, while inadequate posture can contribute to dysfunction. I often use the phrase “joint alignment dictates muscle position and function.” Whether you’re recovering from childbirth, managing incontinence, experiencing pelvic organ prolapse, or just sense your pelvic floor is too tight or too weak, integrating postural corrections into care can offer significant benefits and may be the missing puzzle piece to your ongoing symptoms.
Our bodies are built to move and stabilize in coordinated patterns—and posture is a key factor in how our various body systems all function together.
Want to learn more about your posture and simple corrections, check out these videos that walk you through assessing and teach you some simple tricks to try!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic floor muscles, neutral posture, pelvic floor exercises, pelvic floor weakness, pelvic floor muscles form, weak pelvic floor muscles, hypertonic pelvic floor, pelvic health physiotherapist, dynamic posture, correct posture, bad posture, muscle tension
By Elizabeth Akincilar, MSPT, PHRC Lexington
At the Pelvic Health and Rehabilitation Center, we talk about the pelvis all day long. But today, instead of focusing on how it works, let’s explore something just as interesting—where our body part names actually come from!
If you’ve ever wondered why we call certain body parts what we do, you’re not alone. The names of our anatomy often come from Latin and Greek roots, and sometimes those origins are surprising, hilarious, or even a little strange. Let’s take a deep dive into the etymology of some of the most important (and often overlooked) parts of the body, focusing on the pelvic region.
Get ready for a linguistic journey through the origins of words like vulva, penis, uterus, anus, and more. Trust us—it’s going to be fun!
Vulva & Vagina: A Case of Confusion
Many people use vagina and vulva interchangeably, but they actually refer to different parts of the anatomy.
The word vulva comes from the Latin term meaning “womb covering” or “wrapper.” It’s an accurate description, considering the vulva includes all the external genitalia—the labia, clitoris, and vestibule.
Meanwhile, vagina comes from the Latin word meaning “sheath” or “scabbard”—yes, like the thing that holds a sword. The ancient Romans weren’t known for their subtlety. This name makes sense anatomically, as the vagina is a muscular canal, but it also gives insight into historical perspectives on anatomy. Language often reflects cultural viewpoints, and the idea of the vagina as a sheath suggests a male-centered way of understanding the body.
If nothing else, this should encourage everyone to use these words correctly: the vulva is the external structure, and the vagina is the internal canal.
If you’re experiencing vulvar or vaginal pain, learn how pelvic therapy may be able to help!
Pudendal Nerve: The Nerve of It!
The pudendal nerve is an important structure that provides sensation to the pelvic floor, genitalia, and surrounding areas. But did you know its name has roots in shame?
The word pudendal comes from the Latin pudendus, which means “that which must be ashamed of.” Yikes. This tells us a lot about how early anatomists—and society—felt about genitalia.
Thankfully, modern medicine has moved far beyond this outdated perspective, and pelvic health specialists like us are here to remind you that there is nothing shameful about your body!
If you think you may have pudendal neuralgia, learn how PHRC may be able to help you!
Penis & Scrotum: Simple but Effective
The word penis comes from Latin, where it literally means “tail.” Straightforward, right? In some ancient texts, it was also used to mean “organ” or “limb.”
As for scrotum, the word likely comes from the Latin scortum, which means “leather pouch” or “hide.” That’s a fairly accurate description—though maybe not the most flattering one!
Learn more about penile and scrotal pain here.
Please note, medical experts do not recommend or condone testicular tanning.
Anus, Rectum, & Colon: A Trip Down the Digestive Tract
The anus gets its name from the Latin word for “ring,” which makes perfect sense given its circular structure.
Meanwhile, the rectum means “straight” in Latin, which is a little misleading. While the rectum is somewhat straighter than the colon, the entire digestive tract has plenty of curves. Ancient anatomists may have been working with incomplete information when they named this part of the body!
The colon comes from the Greek kolon, which simply refers to a portion of the intestine. Unlike some of the other words on this list, this one doesn’t come with an amusing or controversial history—it’s just a straightforward name for a key digestive structure.
If you’re struggling with bowel dysfunction, PHRC can help!
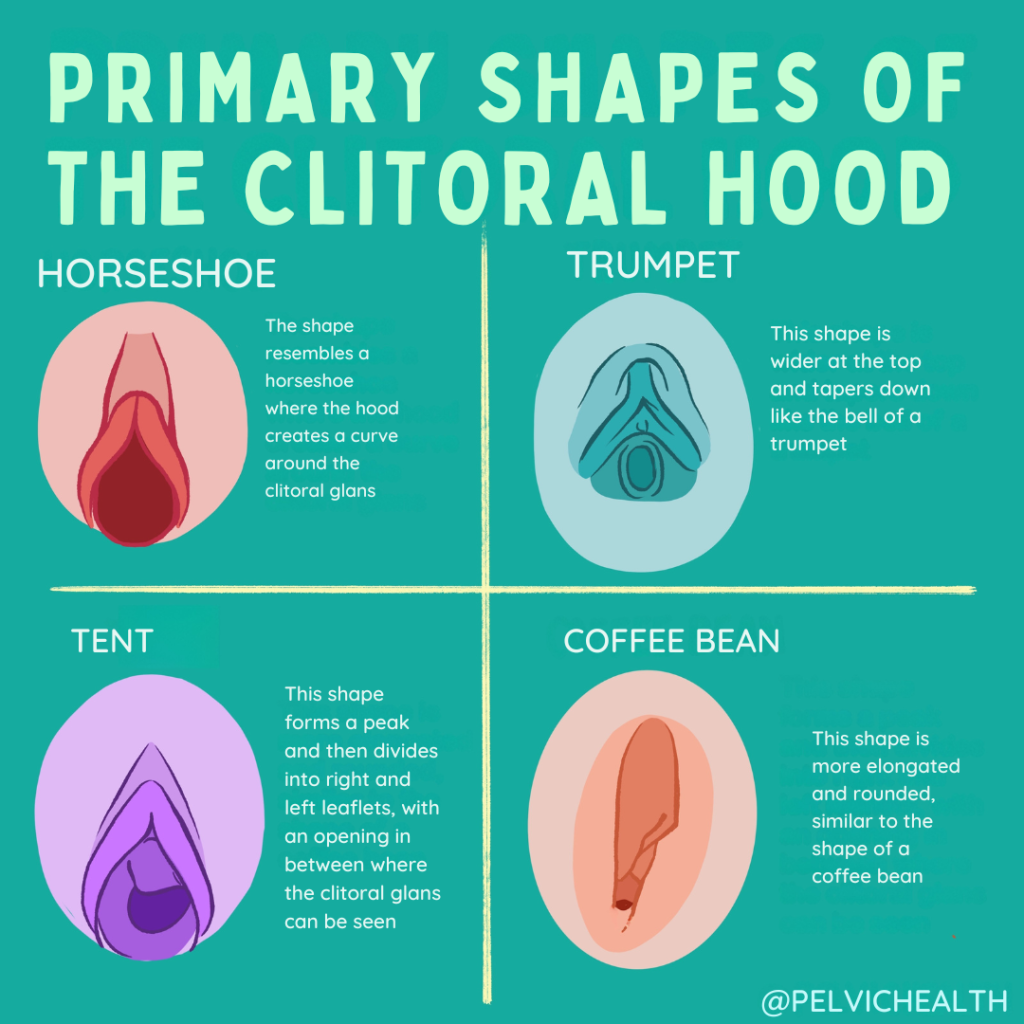
Clitoris & Labia: Unlocking the Mystery
The clitoris has one of the more interesting etymologies on this list. It comes from the Greek kleitoris, which possibly means “little hill” or “key.” Some scholars think the term may have been metaphorical—after all, the clitoris could be seen as the “key” to unlocking pleasure.
The clitoris is thankfully getting more media attention in the scientific community and the media!
Learn more about the clitoris here.
Meanwhile, labia is a Latin word that means “lips,” which is a simple yet accurate description of the structures that form the outer and inner folds of the vulva.
Interestingly, the clitoris was largely ignored in anatomical texts for centuries, despite being first described by ancient Greek physicians. Many early medical texts omitted it entirely, reflecting a broader societal tendency to overlook female pleasure and sexuality. Today, we know the clitoris is a complex organ with a vast network of internal structures, showing just how much early anatomists underestimated it!
Uterus & Ovary: Where Life Begins
The word uterus comes from Latin and simply means “womb” or “belly.” It’s one of the more straightforward anatomical terms, used in many variations throughout history.
The word ovary, on the other hand, is directly linked to the Latin word ovum, meaning “egg.” This makes perfect sense, as the ovaries are responsible for producing and releasing eggs during the reproductive cycle.
Perineum: The Sacred Space
The perineum is the area between the genitals and the anus, and its name has an interesting backstory. It comes from the Greek perinaion, which means “around the temple.”
Why did the Greeks think of this part of the body as a temple? Some historians believe it was considered a sacred or protected area, possibly due to its role in childbirth and sexual function. Others think it may have been a poetic way of describing its location between two important parts of the body. Either way, the name gives this often-overlooked region an air of mystery and reverence.
Bladder: The Body’s Balloon
The word bladder comes from the Old English blaedre, meaning “a blister, bag, or pouch.” This is one of the oldest words on our list, dating back to early Germanic languages.
The bladder’s job is to store urine before it leaves the body, and its name perfectly describes its function. It’s essentially a flexible, expandable pouch that fills up and empties out as needed.
Experiencing bladder dysfunction? PHRC may be able to help!
Language Shapes How We See Our Bodies
The words we use for our bodies aren’t just labels—they reflect history, culture, and even outdated beliefs. Some terms, like pudendal, remind us of the shame once associated with these body parts, while others, like clitoris, hint at ancient knowledge that was later ignored.
As pelvic health specialists, we love helping people understand their bodies and feel empowered in their own skin. Whether you’re dealing with discomfort, pain, or just have questions, we’re here to help—no shame, no embarrassment, just expert care.
So next time you hear one of these words, you’ll know exactly where it comes from—and maybe even impress your friends with a fun etymology fact or two!
If you have questions about your pelvic health, reach out to PHRC. We’re always happy to talk about the amazing human body—no matter what part of it you’re curious about!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!