Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
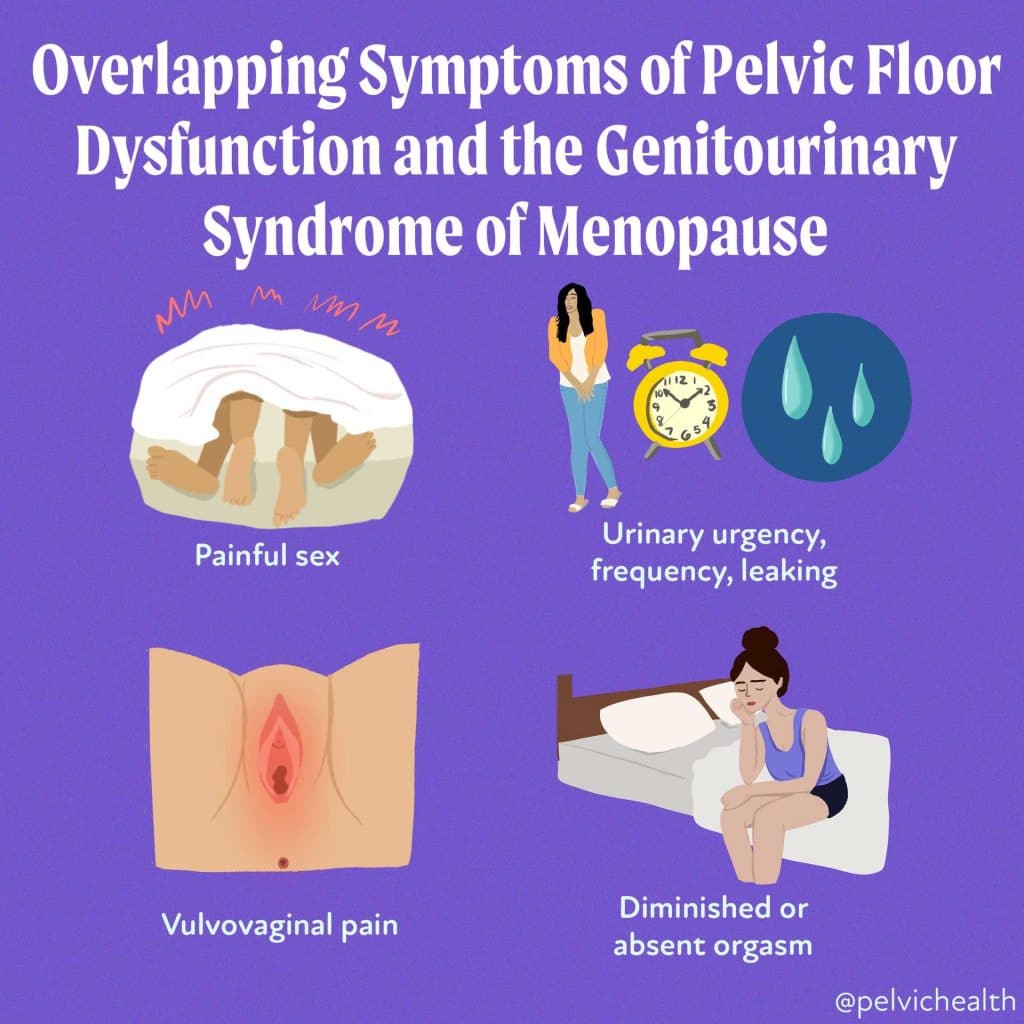
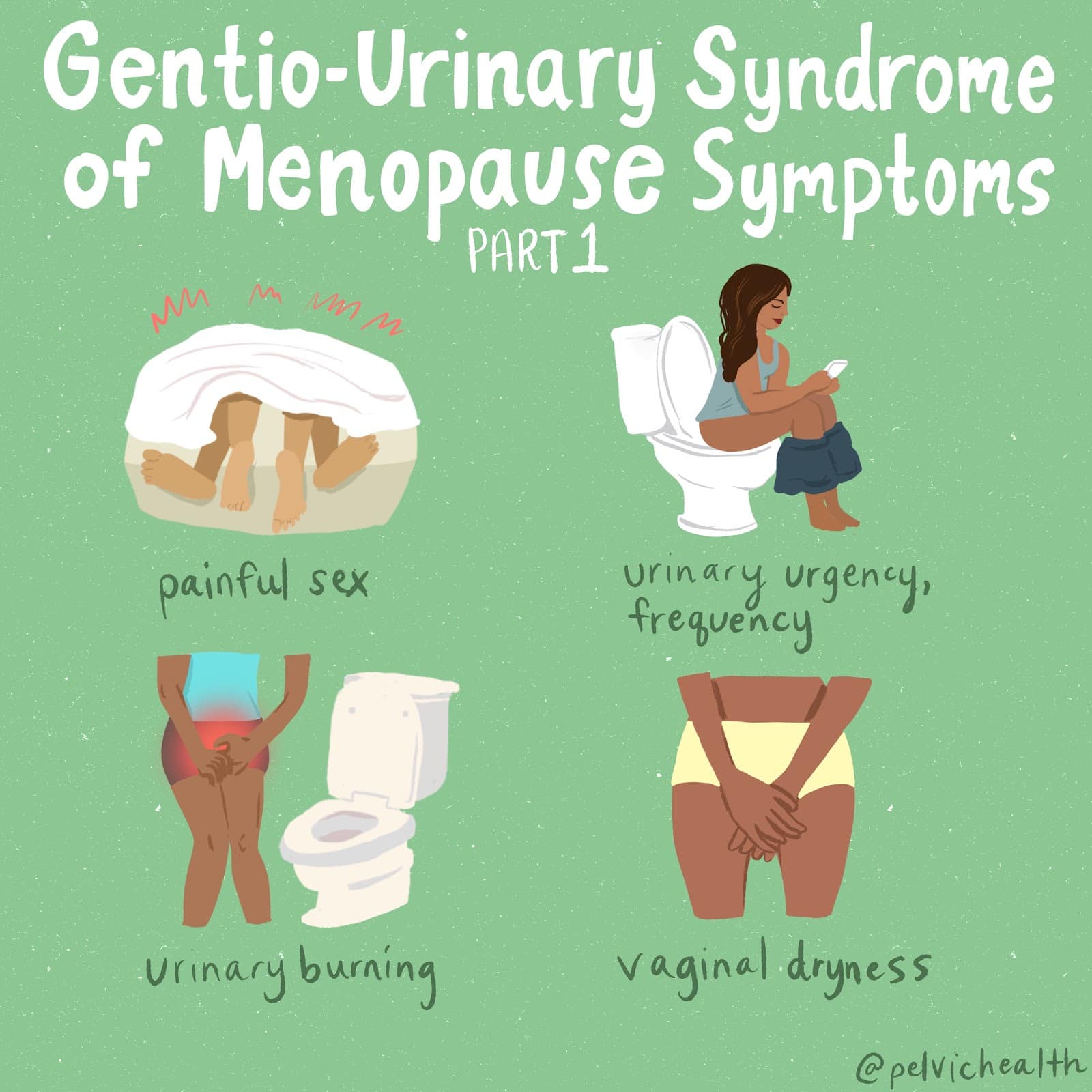
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting
An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.
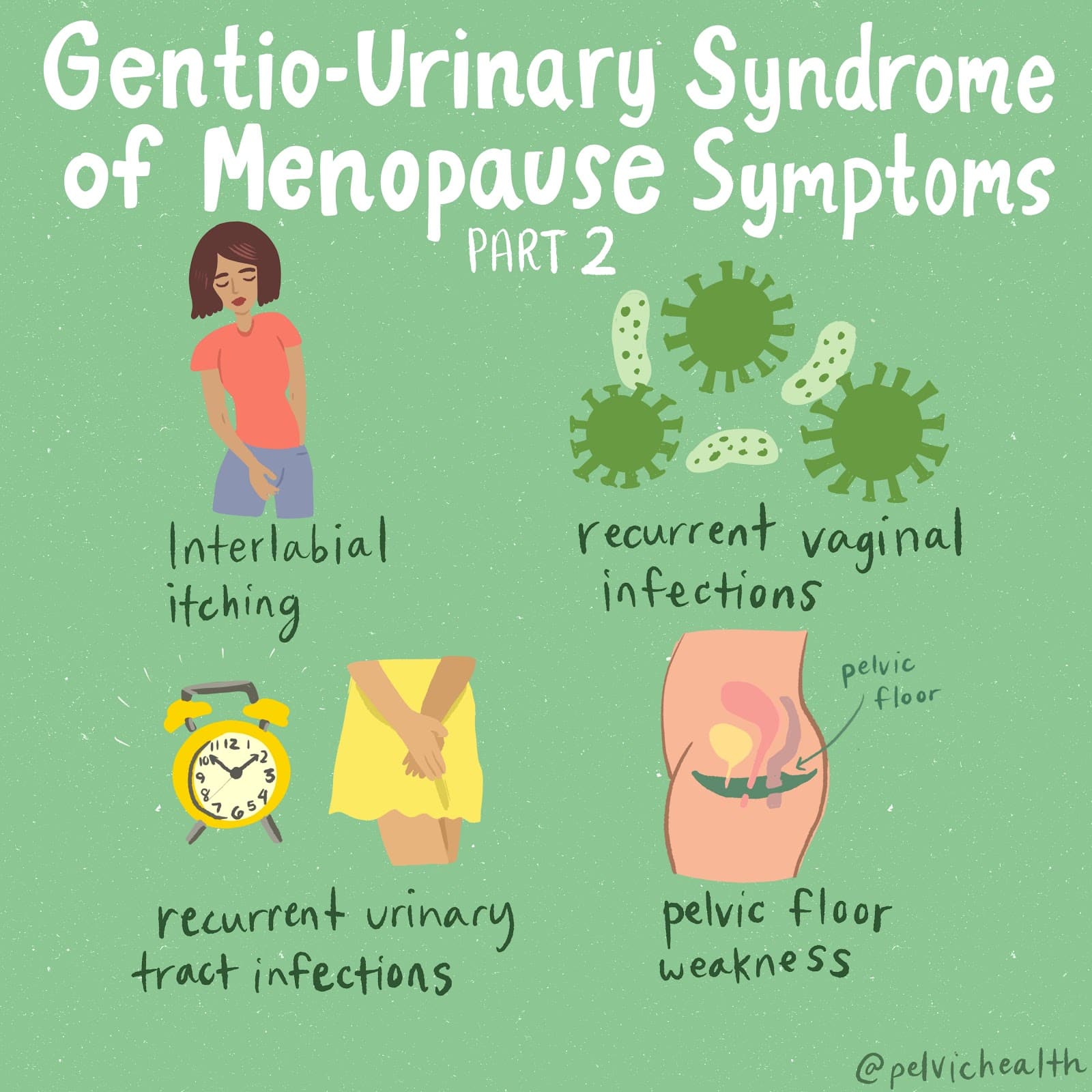
Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Alexa Savitz, DPT, PHRC Pasadena
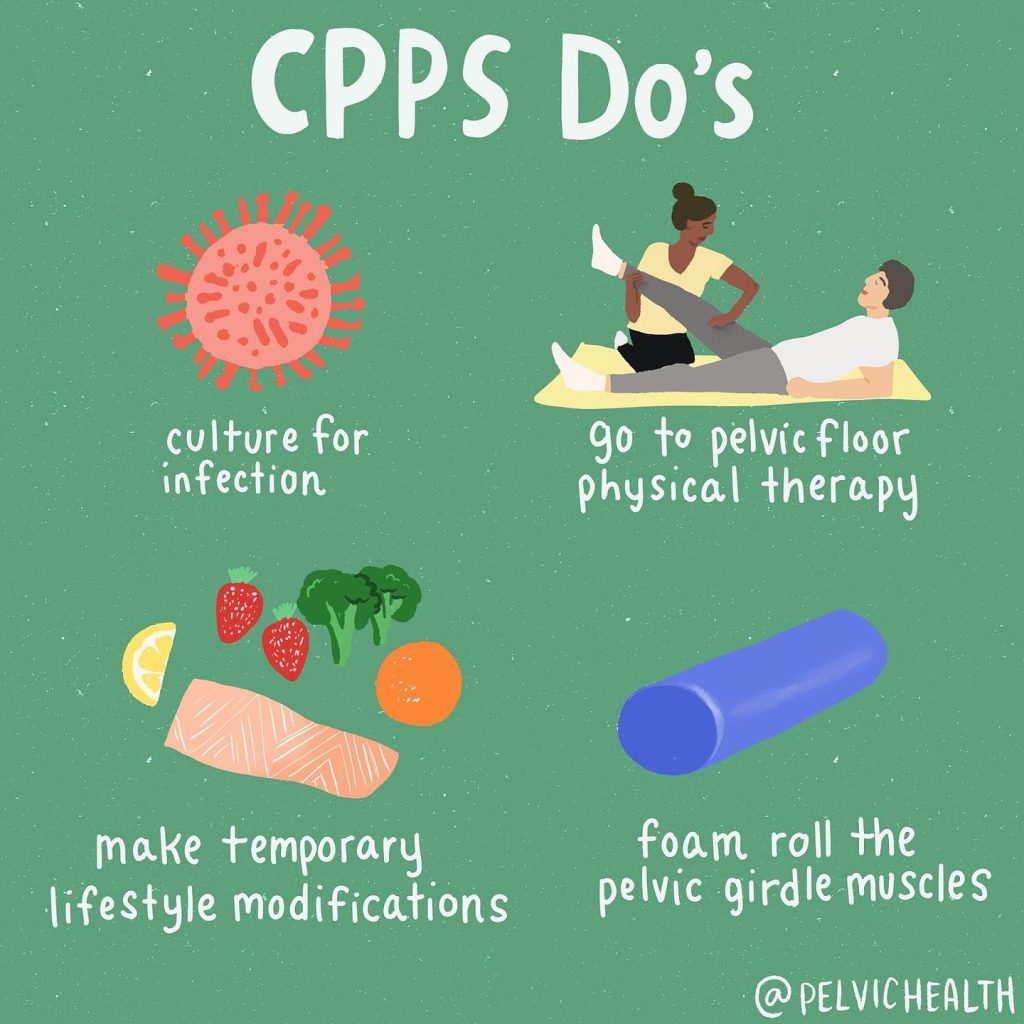
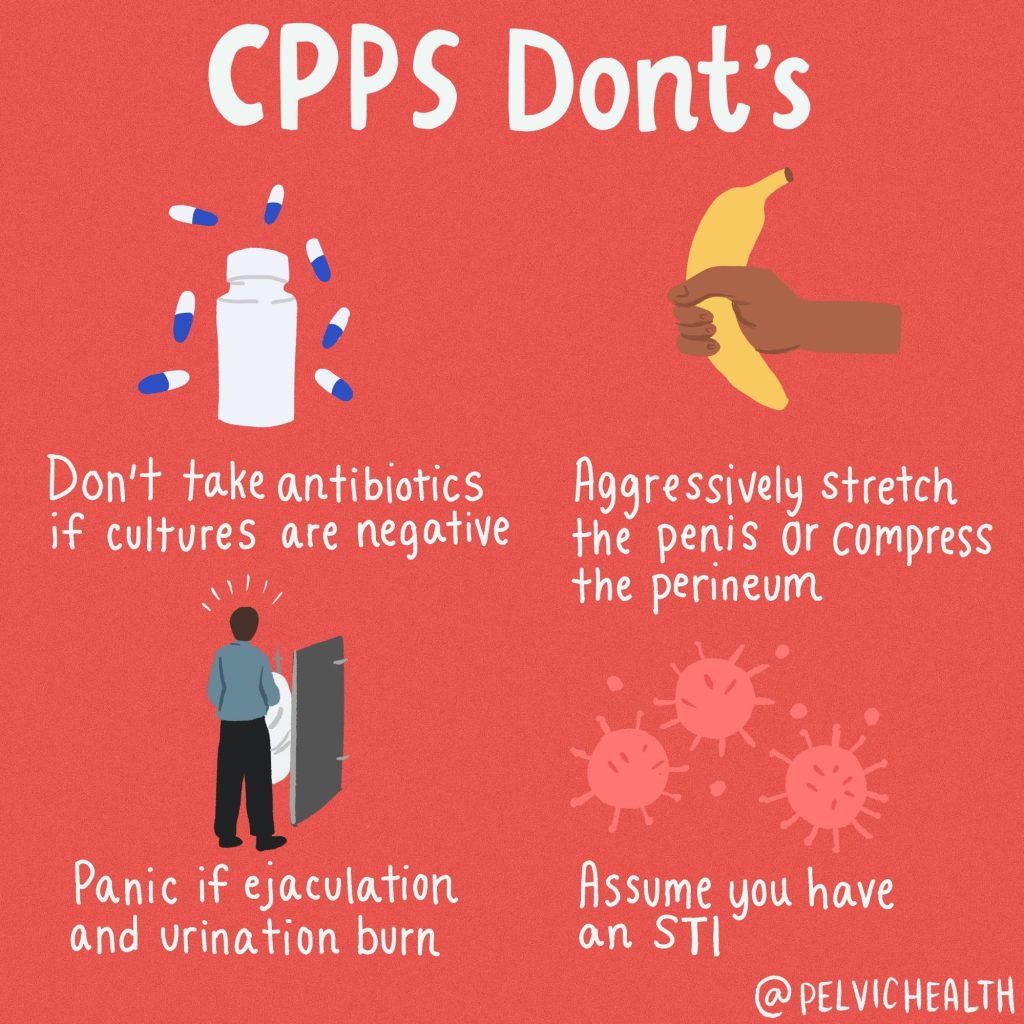
At PHRC we are no strangers to working with male pelvic pain patients. About 50% of our case loads at PHRC can be made up of male pelvic pain diagnoses. Research shows that up to 16% of men suffer from Chronic Pelvic Pain Syndrome (CPPS) at some point in their life. Pelvic floor physical and occupational therapy (PFPT) is an integral part of treating CPPS yet many people do not realize this. Here is a success story and case overview of how PFPT helped a male patient overcome CPPS.
Chris is a 32 year old who was referred to PHRC by a local urologist because of the following symptoms:
- painful urination
- urinary urgency and frequency
- pelvic pain with sitting
- pain with sexual function
He reported he had dealt with these symptoms for 1 year. Chris is a pilot and long trips multiple days per week required him to sit with this discomfort. You could imagine how his symptoms were impacting his quality of life.
He had seen multiple providers, taken antibiotics, and had many tests performed including ultrasounds and CT scans that were all normal. He had begun eliminating bladder irritants including spicy foods and alcohol as he noticed these substances increased his urinary urgency and frequency. He tried eliminating coffee, however this was challenging to exclude from his daily routine and schedule, and he observed that it was associated with his urinary symptoms. Prior to coming to PHRC he started to use a cushion while sitting and had been doing pelvic floor stretches which helped jump start his journey towards healing.
Patient Goals:
Chris’ goals were to improve his pain and symptoms to make work travel more tolerable with less discomfort and to improve his pain associated with sexual function.
Physical Examination Findings
- Gluteal, hip rotator, and rectus abdominis myofascial trigger points
- Reduced hip mobility and gluteal strength
- Obturator internus palpation reproduced the pain he felt with sexual function
- Severe pelvic floor muscle (PFM) tension at the urogenital triangle
- Pain at the perineal body with palpation
- Impaired PFM length-tension relationship contributing to his inability to contract and lengthen the PFMs
Assessment
I suspected due to Chris’ sedentary lifestyle as a pilot that the constant compression on the PFMs were causing tension and a reduction in blood flow to the area resulting in pelvic pain and pelvic floor muscle dysfunction. The PFMs, more specifically the muscles of the urogenital triangle, attach to the perineal body which can cause perineal pain and I suspected his painful sitting. They are also the muscle group responsible for urinary and sexual function. The severe tension found in these muscles I suspected were contributing to his urinary symptoms, painful sitting, and pain associated with sexual function.
Treatment Plan
Chris’ plan included connective tissue and soft tissue mobilization, and myofascial trigger point release of the external pelvic girdle muscles and pelvic floor muscles to address the dysfunction. It also included neuromuscular reeducation to improve flexibility and coordination of the PFMs, and therapeutic exercise with a home exercise program that included strengthening of the pelvic girdle muscles to support the PFM tension.
Outcomes
At 4 weeks he reported less pain with sexual function and he was feeling more normal when sitting prolonged for flights.
At 8 weeks he was having 85% less pain with sexual function. He was staying consistent with his home exercises even while traveling. He reported that his urgency and frequency continued to act up when consuming caffeine. Caffeine is a diuretic and can cause the body to produce more urine. We discussed how he could still have that cup of coffee while staying hydrated to help the urgency and frequency. He progressed with his gluteal and core strengthening exercises to help support his PFM tension.
By 12 weeks of pelvic floor physical and occupational therapy he was able to return to his regular exercise routine. Abdominal exercises in yoga used to flare him up, however he was able to return to yoga and participate in all poses without pain or symptoms. His primary goal that he achieved was that he was able to sit for flights without symptoms and he felt normal. The pain with sexual function had reduced to occasional minimal tightness afterwards. He reported feeling confident he could manage any flare ups in the future because of the tools and exercises that he had learned in PFPT at PHRC.
Conclusion
Pelvic pain can greatly disrupt our daily life, making it challenging to go about our routines, hobbies, and work. With pelvic floor physical and occupational therapy effective relief can be achieved by improving muscle function, reducing tension, and restoring mobility. Through targeted treatment and a personalized plan at PHRC, our male pelvic patients can experience lasting relief, return to the activities they love, ultimately reclaiming their health and well-being.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: Chronic Pelvic Pain treated, irritable bowel syndrome, chronic pain, chronic pelvic pain diagnosed, physical and occupational therapy, pain relief, pelvic organs, treat chronic pelvic pain, painful bladder syndrome, interstitial cystitis, pelvic floor dysfunction, chronic pain syndrome, pelvic exam, persistent pain
By Alexa Savitz, DPT, PHRC Pasadena
Cauda equina syndrome and pudendal neuralgia can present with similar alarming symptoms, which may complicate the diagnostic process. However, prompt and urgent referral is critical when cauda equina syndrome is suspected to prevent the progression of symptoms. In contrast, pudendal neuralgia is not an emergent condition though we acknowledge pudendal neuralgia symptoms can be quite severe and feel like there is an emergency.
Recognizing both the overlapping features and the key differences between these diagnoses is essential for ensuring appropriate treatment and management.
Many health care professionals who are not familiar with pelvic pain syndromes typically think of cauda equina when they hear patient reports of urinary and bowel symptoms, many pelvic floor providers may not think of cauda equina because so many other tissues, nerves and structures create the same symptoms. We hope this post helps both sides recognize what’s what and help people get the care they need!
Cauda Equina
Cauda equina symptoms:
- Bladder dysfunction (retention is most common, leakage)
- Bowel dysfunction
- Saddle numbness (in the area of the perineum, bony pelvis)
- Changes in sexual function/erectile dysfunction
- Acute or chronic low back pain
- Loss of or altered sensation (numbness/tingling) in the buttocks, legs, feet
- Weakness in the lower extremities
According to Hawa et. al, there is no consensus for the exact symptoms, however most commonly sensory loss and bladder dysfunction with retention are the most important factors to consider. Back pain, bladder dysfunction, and weakness can often present under different timelines over days or prolonged development over months.1
Causes:
- Herniated discs
- Lumbar spine stenosis
- Fracture
- Tumor
- Infection
- Cysts
Treatment:
- Surgical decompression to the affected levels of the spine to take pressure off the spinal nerve roots that are impacted.
- The timing of surgical intervention has been suggested to be within 48 hours in previous studies. However other research reported no significant correlation between clinical success and timing of surgery. It is recommended that surgical intervention be performed at “the earliest practical opportunity”.1
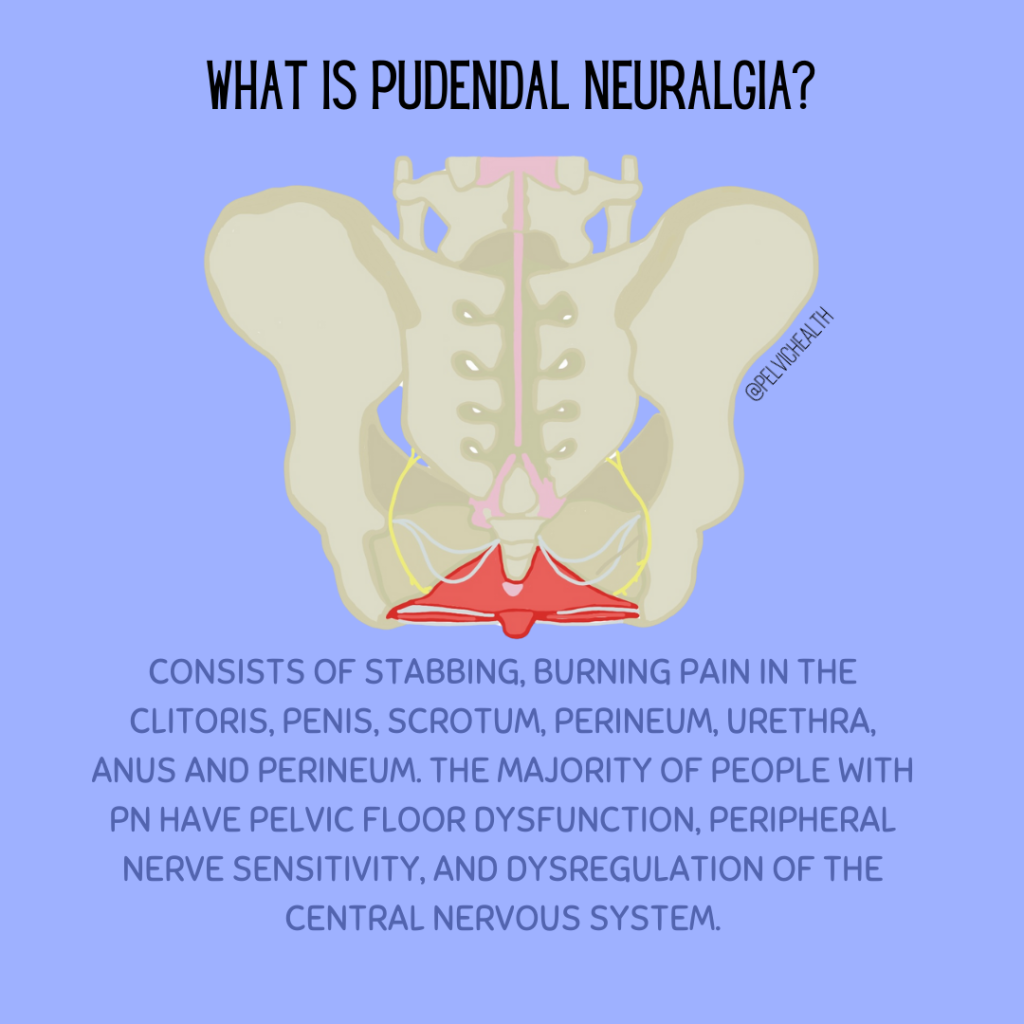
Pudendal Neuralgia
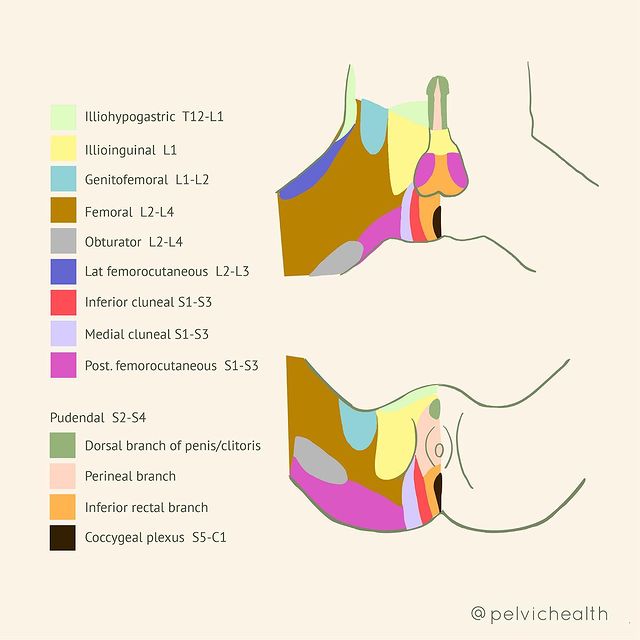
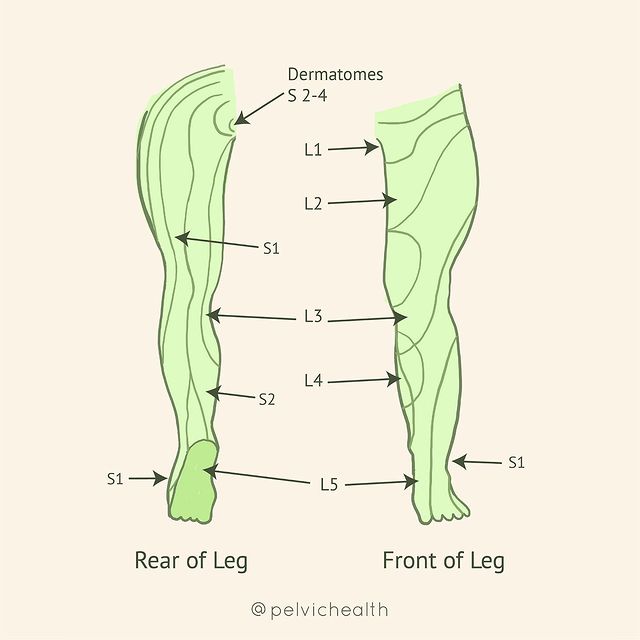
Pudendal Neuralgia is pain in the sensory distribution of the pudendal nerve that is described as tingling, stabbing, shooting in nature. The pudendal nerve originates at sacral nerve roots S2-S4, then divides into 3 branches – inferior rectal, perineal, and dorsal clitoral/penile. The pudendal nerve is a mixed nerve containing sensory, motor and autonomic fibers. It innervates the majority of the pelvic floor muscles, the distal ⅓ of the urethra and rectum, and the sensory distribution includes the genitals, perineum, and anus.
Common Symptoms:
- Bowel dysfunction (Constipation, pain in the anus or anywhere is in the sensory distribution before, during or after bowel movements)
- Bladder dysfunction (Urinary urgency/frequency, pain, urination triggering symptoms elsewhere in the sensory distribution)
- Pain in the sit bones or ischial tuberosities
- Pain with orgasm
- Pain in the vulva, penis, perineum, clitoris
The pudendal nerve also has autonomic fibers which make this nerve unique in its presentation causing symptoms including:
- increase in heart rate
- decrease in the mobility of the large intestines
- constriction of blood vessels
- pupil dilation
- perspiration
- increased blood pressure
- goosebumps
- sweating, agitation, and anxiety
Causes:
- Prolonged sitting
- Activities such as cycling, horseback riding, weightlifting
- Childbirth
- Trauma/Falls
- Radiation to the pelvis
Treatment:
- Physical and Occupational Therapy
- Botox
- Nerve blocks
- Medications (ie. Lyrica, Cymbalta) with proper therapeutic dose and length of time for effectiveness.
- Lifestyle modifications
Please check out our pudendal neuralgia resource guide for more information!
How can we differentiate between the two?
Consider:
- Mechanism of injury: how did the symptoms begin?
- Imaging. If you suspect cauda equina may be the cause of symptoms, urgent referral for imaging is recommended.
- Pain location
- Unilateral or bilateral symptoms present
- Lower extremity sensory loss and motor weakness is more indicative of cauda equina or spinal pathology.
- Note: the pudendal nerve can also cause distal lower extremity numbness/tingling along the S2 dermatome. However, motor weakness in the lower extremity is not a symptom of PN.
As you can see, there are a few overlapping symptoms of cauda equina and PN, however their treatments take a much different approach. This highlights the importance of conducting a thorough subjective history, examination, and a prompt referral if needed, for your patient presenting with any of these signs and symptoms.
References:
Hawa A, Denasty A, Elmobdy K, Mesfin A. The Most Impactful Articles on Cauda Equina Syndrome. Cureus, 2023 Apr 24;15(4):e38069. doi: 10.7759/cureus.38069
Prendergast, S. How do I know if I have Pudendal Neuralgia or Pudendal Entrapment. 2013 Nov 14. Pelvic Health and Rehabilitation Center Blog. https://pelvicpainrehab.com/blog/how-do-i-know-if-i-have-pudendalneuralgia-or-pudendalnerveentrapment/.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: nerve pain, pain relief, chronic pelvic pain, severe pain, pudendal nerve pain, bladder and bowel, pain management
By Cambria Oetken, PT, DPT
The lost art of breathing…
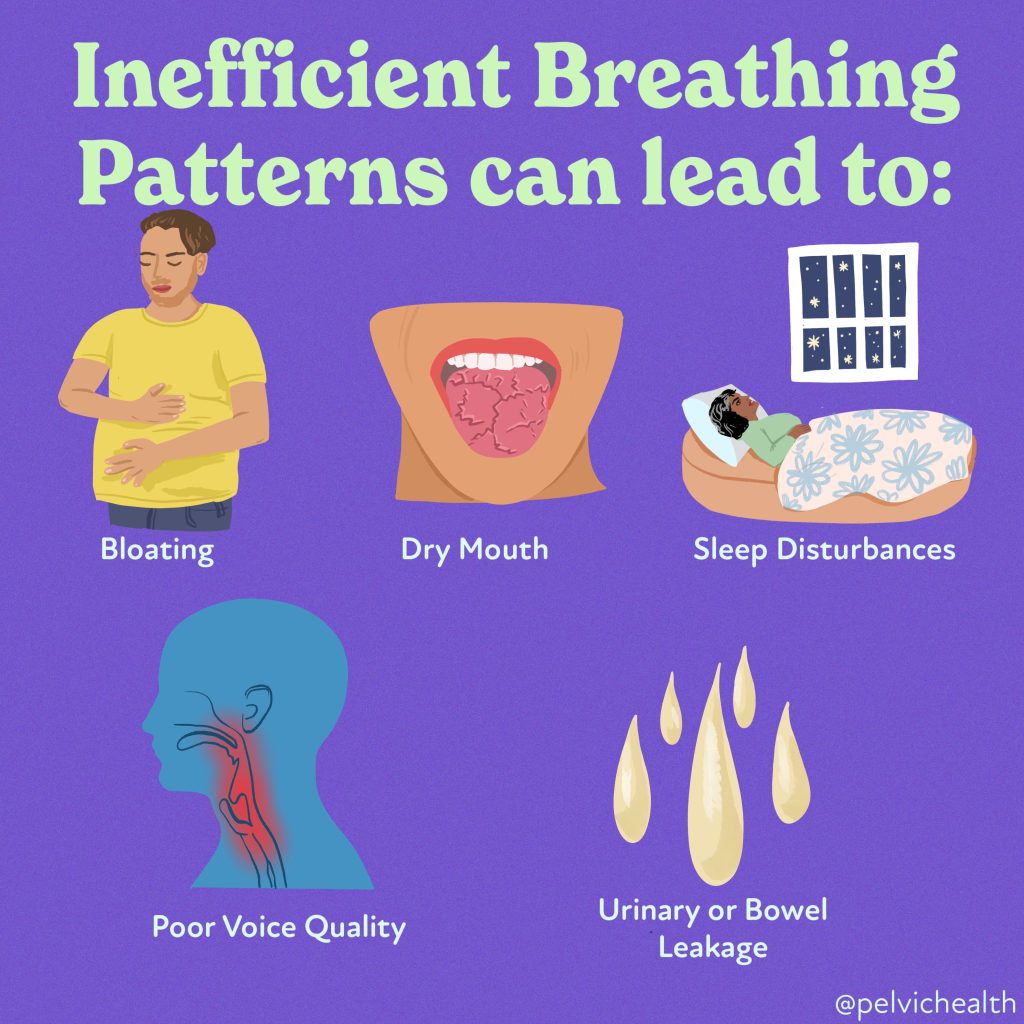
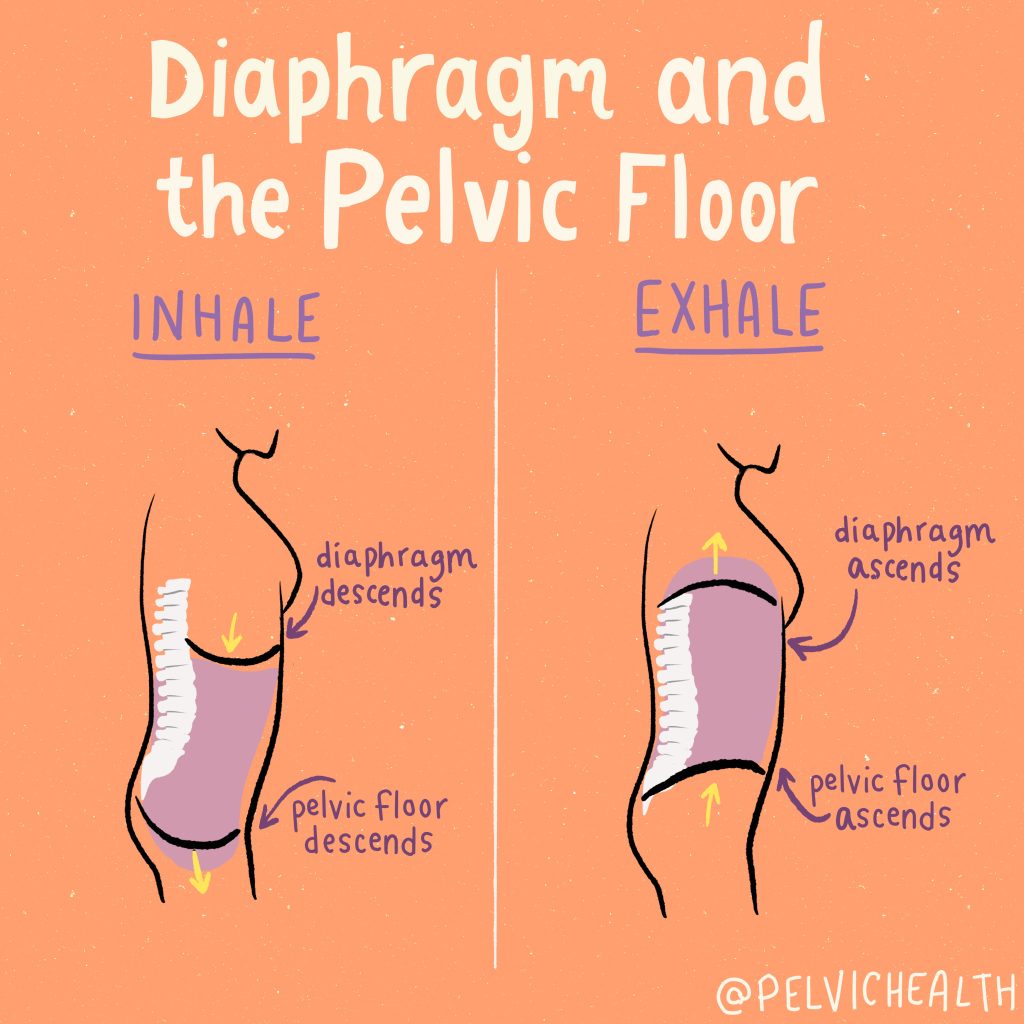
I recently read the book Breath: The New Science of a Lost Art, written by author James Nestor who explores the power of breath, its impact on our health, and the ways in which we’ve lost touch with the ancient practices that can unlock optimal wellbeing. Breathing is a powerful tool that has a massive relationship and impact on each of our body systems in unique ways. While breathing has an affect on our overall health, one area where improper breathing has a huge impact is on our pelvic floor. You may have read our blog on ways to relax your pelvic floor and read how our diaphragm and pelvic floor mirror each other on each inhale and exhale. Because of this process, our breathing has a major impact on the function of our pelvic floor, the ability of it to relax and contract and the ability to decrease pain. More on this below so keep reading.
However, the most fascinating of breathing of all is how it has changed and developed over thousands of years to a point where we are now the worst breathers of all time. In James Nestor’s book he discusses how our modern lifestyle has drastically changed the way we breathe, leading to a host of health issues—especially bad breath, poor sleep, and even anxiety. Humans’ facial structures have evolved due to changes in diet and lifestyle over thousands of years likely due to increased processed and soft foods which is a huge change from our ancestors. Our ancestors had broader, stronger jaws, larger airways, and better dental health because they ate tougher, uncooked foods that required more chewing. In result, our jaws and teeth have become smaller, our nasal passages have narrowed, and our faces have changed shape. This has led to issues like misaligned teeth, sleep apnea, and poor breathing habits.
James emphasizes breathing through the nose and breathing slower to name a few of the strategies to obtain numerous benefits. He ties all of this together by suggesting that our current “bad” breathing habits are a direct result of how our faces have changed and how we’ve become disconnected from the ancient practices of proper breathing.
The Diaphragm and Its Role In Pelvic Health
If you’ve ever been to a pelvic floor therapist, you might have encountered diaphragmatic breathing, also known as “belly breathing.” While this is a great place to start, true diaphragmatic breathing involves more than just the belly expanding—it’s a 360-degree movement that requires the entire rib cage to expand in all directions. Diaphragmatic breathing is a great start and can be extremely beneficial just practicing on your own time. The diaphragm is not only the muscle we use to inhale but also plays a crucial role in our posture and core stability.
Anatomy Lesson
The diaphragm is a dome-shaped muscle that attaches to the lumbar vertebrae and lower ribs. For optimal breathing, your rib cage should expand not just forward, but backward into the spine and outward to the sides.. This is something that takes a lot of practice and can be helpful to walk through with your therapist or breath work teacher.
The diaphragm does more than help you breathe—it plays a critical role in stabilizing your trunk, supporting your posture, and regulating intra-abdominal pressure. Because of its connections to core muscles like the transverse abdominis and the hip flexors, a weak core or imbalanced muscles can cause the diaphragm to overcompensate, leading to issues like pelvic floor dysfunction, low back pain, hip tightness, diastasis recti and pelvic organ prolapse. You may now realize how complex and interconnected this muscle is, therefore, if one of these interconnected muscles fail to show up, our diaphragm must work harder to provide the postural support required.
Maybe, just maybe we can breathe our way to a more optimal pelvic floor, a stronger core, reduce low back pain, improve prolapse and diastasis recti…the list goes on.
If you are facing some of the above issues, it may be time to simplify and hone in on your breath.
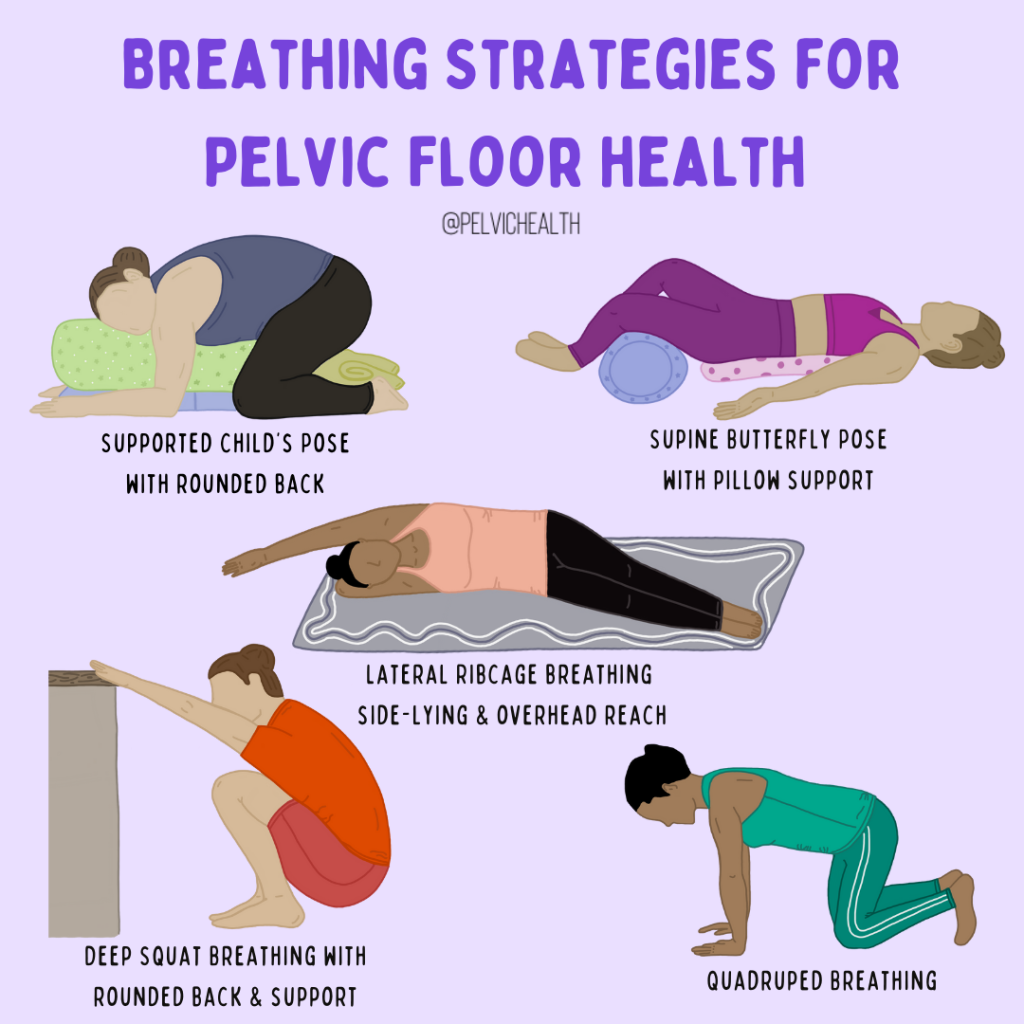
Breathing Strategies
A great place to start integrating improved breathing is practicing in multiple different positions to where you can emphasize expansion into different areas.
Positions
- Supported child’s pose – back rounded
- Lateral rib cage breathing in sidelying, arm reaching overhead
- Supine butterfly pose with pillow supports, potentially pillow under upper back
- Quadruped breathing (on hands and knees)
- Deep squat breathing – rounded forward holding onto countertop
In these above positions, focus on breathing into the area that is being opened up or stretched. Think about breathing into areas that feel potentially restricted or tight and see if you can send your inhale to those regions.
Breathing Patterns
- Nose Breathing
Breathe in and out through your nose. This helps regulate pressure in the pelvic floor and encourages slower, more controlled breathing. - 1:2 Ratio Breathing
Inhale through your nose for a count of 4 seconds, then exhale slowly through your mouth for 8 seconds. This helps activate the parasympathetic nervous system and encourages relaxation. - 5.5 Breathing
Inspired by Nestor’s book, Breath, this technique involves breathing at a rate of 5.5 liters of air per minute. This is roughly a 5.5-second inhale and 5.5-second exhale. Try practicing this for a couple of minutes each day to see how it feels. (Note: This does not have to be a perfect 5.5 seconds, it can be close to achieve the same results)
Final Thoughts: Simplifying Your Breath
Breathing may seem like a simple, automatic function, but the way we breathe can have a profound impact on our pelvic health. By focusing on deep, diaphragmatic breathing, we can improve core stability, reduce pelvic pain, and even help with issues like prolapse and diastasis recti. So, take a moment each day to practice these techniques and see how your breath can transform your body from the inside out.
Our Own How-To YourTube Resources to Optimize Your Breath and Pelvic Floor
Part 1: Diaphragmatic Breathing
Part 6: Alternate Nostril Breathing
Ready to breathe your way to better pelvic health?
Start practicing these strategies today, and consider booking a session with a pelvic floor therapist or breathwork coach to refine your technique and address any specific issues.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!