Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Keena Batti
Keena Batti is a Los Angeles Chapter Campaign Leader of Tight Lipped. Stephanie Prendergast is a member of the Tight Lipped Speakers Bureau.
When I was 19, I wanted to start taking birth control. When I visited my gynecologist, he cataloged the many ways birth control would benefit me. He also warned of blood clots, but that was the only side effect I was given in my appointment. I didn’t realize that at 19 years old, I was making a decision to take a medication that would drastically alter my life.
Fast-forward a few years..
All throughout my 20s, I experienced UTIs. When I would seek help from my gynecologist, I was told I was “prone” to them, lectured to pee after sex (which I was), prescribed antibiotics, and sent on my way. None of my doctors ever investigated further.
When I was 28, I had a UTI that wouldn’t go away. I took progressively stronger antibiotics for months until I eventually developed an allergy to amoxicillin. I was in such excruciating pain that going to work was torture. My vulva was burning, stinging and itching. I couldn’t use tampons, wear pants or have sex.
After seeing several unhelpful gynecologists and not knowing where else to go, I eventually found a urologist and sexual medicine specialist who diagnosed me with hormonally mediated Vestibulodynia. He told me that my oral contraceptives had affected the testosterone receptors in my vestibule–an area of tissue at the entrance of the vagina. This hormone deficiency caused my tissues to become thin and damaged, leading to all of my pain symptoms.
He performed a q-tip test–a simple test that used just a q-tip to poke various areas on my vulva and vestibule and see if they hurt. None of my gynecologists had performed this test, and I had certainly never had my vestibule examined. My new urologist showed it to me with a handheld mirror–it was red, raw, inflamed and so clearly the source of my pain. I couldn’t believe my other doctors had missed it.
A few months later..
When I was in physical and occupational therapy, my therapist suspected I might have lichen sclerosus. Lichen sclerosus is a condition that affects the vulvar tissue and can cause irritation, itchiness, small fissures and pain with sex. When I went to my gynecologist to tell her my suspicions, she refused to even let me change into a gown and be examined. She looked at me and said, “You’re too young to have lichen sclerosus.” I sought out a more knowledgeable specialist and was eventually correctly diagnosed via biopsy.
I know now that even pre-pubescent girls can have lichen sclerosus. Her assumption was dated, biased, and frankly, wrong. Because of her lack of knowledge, my former gynecologist put me at risk for clitoral adhesions, labial absorption and vulvar cancer.
A few years later, when dealing with cyclical vaginal infections and UTIs, I struggled to find a doctor who could help. I eventually had to travel to Florida to see a vulvovaginal pain specialist and gynecologist who caught another skin condition–lichen planus. I now travel across the country every two months to have my condition monitored by this specialist, because there’s no one in Los Angeles I trust. While I consider myself highly privileged to be able to afford this care, it’s simply inaccessible to most pelvic pain patients.
Chronic vulvovaginal and pelvic pain is a silent public health crisis.
These conditions impact up to 1 in 4 women, non-binary, and transgender individuals. Most patients’ first stop for help with vulvovaginal pain is their OB/GYN. Yet it’s almost impossible to find an OB/GYN who learned how to diagnose and treat these conditions. One study found that vulvar pain patients go to more than 15 doctor appointments before getting a diagnosis, which has certainly been the case in my own journey to find adequate care.
Gynecologists in the United States do not receive training on the basics of vulvar anatomy, vulvar disorders, and common chronic vulvovaginal pain, like vulvodynia. This education is not included in the national requirements for OB/GYN education or taught at the vast majority of programs, leaving many OB/GYNs poorly equipped to treat patients in pain.
At Tight Lipped, we’re working to change this.
The goal of our current campaign is to ensure that every patient with vulvovaginal or pelvic pain can receive comprehensive and compassionate care. In order to achieve this, we’re advocating for all OB/GYN residency programs to provide training on vulvovaginal and pelvic pain conditions.
Nationally, we’ve made inroads this year at seven teaching hospitals, and we need help raising money to deepen our work. All donations will enable us to expand to additional teaching hospitals, learn advocacy skills so we can be effective in our community organizing work, and create informative materials about this campaign to break the stigma and silence associated with vulvovaginal pain. Click here to donate to our work.
By Cambria Oetken, DPT, PHRC Westlake Village
Here is What You Need To Know!
This year new moms are finally getting the attention they deserve! We are excited to report our trusted sexual medicine experts coined a new term that describes the genitourinary hormonal deficiencies of lactating moms experience.
What is the Genitourinary Syndrome Lactation?
Earlier this year, an article was published proposing the novel term, genitourinary syndrome of lactation (GSL) in hopes to bring awareness to this population as well as the proper management, treatment and diagnosis. GSL describes the collection of genitourinary symptoms experienced by postpartum moms during the lactation period. While postpartum already encompasses significant changes both emotionally and physically, additional care should be provided for those suffering from genitourinary symptoms in order to alleviate burden and optimize wellness during a vulnerable time. The collection of genitourinary symptoms include vaginal dryness, dyspareunia, urinary symptoms and alterations in sexual function which can significantly impact these patients quality of life. This syndrome occurs due to hormonal changes associated with alterations in the genitourinary tract that will be discussed further.
Lactation and the potential impact on the genitourinary tract
Lactation comes with in depth physiological changes creating significant hormone shifts. In the first trimester of pregnancy, estrogen changes areola enlargement and maturation. In the second trimester, there is an increase in progesterone that helps with colostrum production and lobe proliferation. By the 3rd trimester, mature cells form, colostrum is produced by oxytocin in preparation for lactation to occur. Postpartum, there is a drop in progesterone and an increase in prolactin to drive milk supply. This increase in prolactin decreases the ovarian production of two crucial hormones, estrogens and androgens (such as testosterone). To maintain proper lactation, prolactin has to be present which in turn continues to suppress estrogen and androgen release. Lactating women therefore experience a hypoestrogenic and hypoandrogenic state, persisting at times as long as lactation continues. This state is similar to menopause. Estrogen is needed for maintaining vaginal wall thickness and lubrication as well as urethral and vulvar thickness. There are several estrogen receptors in this genitourinary tract including the clitoris and bladder trigone as well. Estrogen is also responsible for maintaining lactobacillus which is needed to maintain a healthy acidic PH to help fight off infections. Androgens also work hand in hand with estrogen to maintain vascularity and healthy vaginal tissue therefore, with the reduction of these, this puts the patient at risk for dyspareunia (pain with intercourse), Vestibulodynia (pain at the vestibule), and can limit sexual desire as a whole.
Vaginal dryness continues to be a primary concern in these individuals that can contribute to discomfort, irritation and pain with sexual intercourse (dyspareunia). Another contributing impact from a lack of estrogen is the ability to recover optimally from vulvovaginal tears or injury. Estrogen promotes growth of crucial cells to help repair tissue. Studies have shown that supplementing with estrogen can improve wound healing synthesis and boost collagen during this repair phase.
Another disrupting symptom that is common postpartum is urinary incontinence. Urinary incontinence is common postpartum and can be emotionally distressing and shameful for patients and society has normalized this as a result of pregnancy. Additional conditions include pelvic organ prolapse and even anal incontinence. There is a connection between SUI and collagen and as we know, collagen is reduced in lactating women due to depletion of estrogen needed for tissue repair and collagen optimization.
Treatment Approaches for Genitourinary Syndrome Lactation (GSL)
Pharmacological Options
Vaginal Estrogen Therapy can be an option for women experiencing vaginal dryness or with complaints of dyspareunia, recurrent UTIs, or vulvar and vaginal changes. While there are limited studies on estrogen therapy in this population, there have been positive subjective reports of improvement at the perineum with no serious adverse events noted. The concern and hesitation with vaginal estrogen use is that it may transfer to breast milk or reduce milk supply. However, even in studies using the highest dose of estrogen possible there were no traces of estradiol detected in breast milk and is unlikely to affect breast milk supply. We know from previous research that low dose vaginal estrogen is considered safe even in women with estrogen receptor positive malignancies (cancer).
DHEA has been indicated for the use for the genitourinary syndrome of menopause and is FDA approved for severe dyspareunia in postmenopausal women. DHEA works to convert to estrogen and testosterone and has limited concern for absorption systemically. DHEA is not currently being used in lactating mothers and there are a lack of studies in its use with this population.
Non pharmacological Options
Functional Microablative CO2 laser is being studied for vulvovaginal atrophy and some researchers have found improvements in dyspareunia, pain at vaginal orifice and dryness.
Vaginal Lubricants and Moisturizers
Lubricants and moisturizers can be helpful in this population as vaginal dryness tends to be one of the most common concerns that can also impact sexual functioning. This option could be a first step approach that is conservative and easily accessible. Moisturizers and lubricants with hyaluronic acid (HA) have been shown to significantly improve these symptoms and even quality of life just after 12 weeks of use. Additional studies have shown HA use with estriol cream to have an even greater impact when combined. Some of our favorite moisturizers and lubricants can be found below.
Pelvic Floor Physical and Occupational Therapy and Occupational Therapy
This is crucial in optimizing both peripartum and postpartum challenges involving the genitourinary tract. Through exercises, manual therapy, education on proper postures especially with breastfeeding, body mechanics, improving pelvic floor motor control and strength, enhancing sexual wellbeing and overall optimizing postpartum recovery. Therapy can also help to reduce severe perineal tearing through instruction on perineal massage and positional options during delivery to further reduce recovery time postpartum. Pelvic floor therapy has been shown to decrease the risk of urinary incontinence in late pregnancy and postpartum and women were less likely to report pelvic organ prolapse and with a reduction in unsatisfactory sexual function. Pelvic floor therapy should be considered standard care during and after pregnancy to optimize function, well being and prevent potential genitourinary symptoms.
Conclusion
In conclusion, GSL hopes to be recognized as a diagnosis to help bring support and optimal treatment to these lactating individuals in order to optimize their well being both emotionally and physically during a critical period. Should you be an expecting mom, reaching out to your physical or occupational pelvic floor therapist is a great start to begin preparing for progression of pregnancy, delivery and postpartum and can help guide you through an evolving time. Therapists can also work closely with your provider in managing GSL. If you live near one of our 11 locations, please give us a call, we are happy to help!
Reference:
Perelmuter S, Burns R, Shearer K, Grant R, Soogoor A, Jun S, Meurer JA, Krapf J, Rubin R. Genitourinary syndrome of lactation: a new perspective on postpartum and lactation-related genitourinary symptoms. Sex Med Rev. 2024 Jun 26;12(3):279-287. doi: 10.1093/sxmrev/qeae034. PMID: 38757214.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: genitourinary system, urinary tract, breastfeeding, birth, infants, support, breastfed, health
By Cambria Oetken, DPT, PHRC Westlake Village
The Clitoris. We Found it!
There is conflicting evidence as to when the clitoris was exactly discovered and studied. It is thought to date back to 400 BC when Hippocrates described the clitoris as a protrusion which functioned to protect the vagina. There was a later time when anatomists denied its existence altogether. With religious and cultural influences, the clitoris was either disregarded or demonized and in the middle ages, it was even known as “the devil’s teat.” A procedure called a cliteroidectomy (removal of the clitoris) was even a commonly utilized medical practice to treat “hysteria.” With a confusing and lack of understanding about its history, it was only until recently in 2005 that O’Connell, Sanjeevan, and Hutson published in The Journal of Urology recognition of this organ of female sexual pleasure as a three dimensional organ through cross sectional imaging. We now know that the clitoris is more than what is seen on the surface composed of the internal paired clitoral bulbs, corporal bodies, and crura which is composed of erectile tissue. It was not until 2022 however that it was determined the clitoris is composed of 10,000+ nerve fibers which has been discussed as more than a human penis contains. Sounds pretty sensitive and important right??
Stop Ignoring the Clitoris
Historically, and currently, there is a lack of research in regards to the clitoris while the penis has been a counterpoint of research for centuries. Within this new era, the clitoris is becoming more recognized, understood and appreciated for its complexity and sensitivity as well as its importance in female sexual wellness. Luckily, there are prominent medical providers who are bringing more attention to this organ and to women’s sexual wellness as a whole. In a recent New York Times article, written by Rachel E. Gross, she interviews Dr. Rachel Rubin, a urologist and sexual medicine expert, who has been a pioneer in driving attention to women’s sexual health. Dr. Rubin is breaking down barriers around the context of the vulva and the clitoris being “private and shameful” parts thus further empowering the lives of women worldwide. In this article, Dr. Rubin states how the clitoris is “completely ignored by pretty much everyone,” and that “there is no medical community that has taken ownership in the research, in the management, and in the diagnosis of vulva-related conditions.”
F
The article recognizes how there is little to no education about the clitoris in medical school and how women’s health and sexual health as a whole is not a focus for women at all. In fact, in many surgeries such as pelvic mesh surgeries, urethral surgeries even minimally invasive hip surgeries put this organ, its several nerve endings and supporting pelvic nerves at severe risk however is not protected by providers due to its historical lack of relevance, understanding and underlying anatomy.
Women’s lives can be severely impacted by damage to this important structure just as a male would be should there be damage to their counterpart. We now know that sexual wellness is a major part of health both mentally, emotionally and physically and thus should be treated with such importance as any other organ in the body.
Now for a quick anatomy lesson…
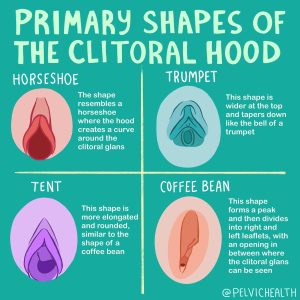
The clitoris is composed of more than just what we see as a knob on the external surface. What you see externally is the conveniently placed glans towards the top of the vulva with the clitoral hood draping over it. Think of this as the “tip of the ice berg” because beneath the surface are the much larger paired clitoral bulbs, corporal bodies, and crura, which are all composed of erectile tissue (as pictured below). Similarly these same structures can be identified in the male counterpart of the penis.
Men who are uncircumcised retract their foreskin to clean underneath. All people with a clitoris should carefully do the same, let us explain!
View this post on Instagram
Caring for and finding your clitoris
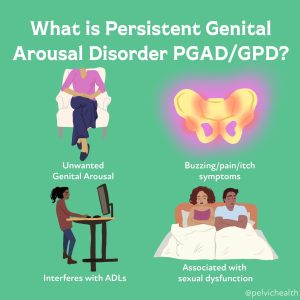
If you are having symptoms at the clitoris, such as pain, decreased arousal, decreased orgasm, absent orgasm, or additional arousal conditions such as persistent genital arousal disorder(PGAD)/genito-pelvic dysesthesia (GPD) it is important to share these concerns with your provider.
At Home Self-Exams
However, performing a self exam at home and becoming familiar with your anatomy can be a great start. Regular self exams can be helpful by using a mirror or by palpating the structures. Oftentimes there can be clitoral hood adhesions, vulvar dermatological concerns, smegma and keratin pearls around the clitoris that could be problematic. To examine your vulvar tissue, begin by laying back with a mirror in order to see the tissues appropriately. Begin by finding the clitoral hood or clitoris at the top of the vulva closest to your pubic bone. You can retract the clitoral hood with two fingers to expose the glans of the clitoris. The clitoral hood should move fairly easily and fully expose the clitoral head. If the clitoral hood does not move optimally or does not expose the glans there could be limited mobility or adhesions present. Also be aware of any smegma or discharge under the hood that could be building up.
A helpful strategy to potentially help with clitoral hood mobility and reduce buildup of discharge is by retracting the clitoral hood in the shower and letting warm water run over the area. Ensure you are avoiding harsh soaps or additional washes to this area to avoid irritation of the tissue. Again, it is always important to speak with your provider or a sexual medicine expert to address these issues.
Multiple pathologies such as pelvic floor dysfunction, pudendal neuralgia, PGAD, and vulvar dermatoses can lead to changes in sexual pleasure and can cause pain. Stay tuned to our blog for more in depth articles, if you have questions we are here to help and please reach out to us!
References
Half the World Has a Clitoris. Why Don’t Doctors Study It?
Human Clitoris Has Over 10,000 Nerve Fibers | Oregon Health & Science University (ohsu.edu). SexualDiversity.org
Maria Uloko, Paige Isabey, Blair Peters. How many nerve fibers innervate the human clitoris? A histomorphometric evaluation of the dorsal nerve of the clitoris, abstract was presented by Blair Peters, on Oct. 27, 2022, at the 23rd annual joint scientific meeting of Sexual Medicine Society of North America and International Society for Sexual Medicine.
Uloko M, Isabey EP, Peters BR. How many nerve fibers innervate the human glans clitoris: a histomorphometric evaluation of the dorsal nerve of the clitoris. J Sex Med. 2023 Feb 27;20(3):247-252. doi: 10.1093/jsxmed/qdac027. PMID: 36763957
Resources
Clitoral Pain: Unmasking Common Culprits
Clitoral Pain: Causes and Treatment
Why Your Clitoris Is In Pain [Youtube Video]
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: clitoral stimulation, clitoral hood, labia minora, glans clitoris, sexual arousal, nerve endings, female genital anatomy, female sexual function, female sexual response