Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Diaphragmatic breathing aka deep belly breathing – how is that an exercise? Many of my patients are surprised when I prescribe and emphasize diaphragmatic breathing in their home exercise programs. Historically, they have associated physical and occupational therapy and/or exercise with strengthening, stretching or the need to get the heart rate up. However, with the pelvic floor muscles, especially for patients with pelvic pain or dysfunctional urinary/bowel conditions, this exercise that may appear relatively low level can do great things for relaxing the pelvic floor.
The diaphragm is a nice, big dome-shaped muscle that sits beneath the rib cage, separating the thoracic and abdominopelvic cavities. In addition to your abdominal muscles and those tiny muscles between the ribs, the diaphragm helps you breath. Because of its position and size, it is your most efficient breathing muscle. When you take a deep breath in, the diaphragm drops down into the abdominopelvic cavity and then naturally recoils back up as you exhale. So how exactly does the diaphragm help facilitate pelvic floor muscle relaxation you ask? Well, if we go back to how the diaphragm and pelvic floor muscles are positioned, we can see that they both run horizontally or along the horizontal plane. In part, because of this positioning, when you take a deep belly breath allowing air to fill your lungs, the abdominopelvic cavity expands and the pelvic floor muscles drop down/lengthen. That’s all fine and dandy but why is it important for individuals with pelvic pain or dysfunctional urinary/bowel emptying to achieve this pelvic floor muscle lengthening and relaxation? Good question!
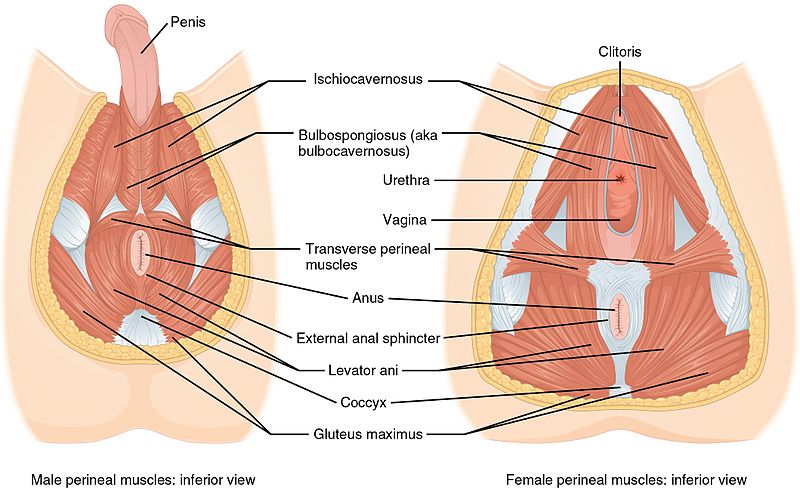
As Shannon discussed in a prior blog on pelvic floor anatomy, the pelvic floor are a group of muscles that sit at the base of the pelvis. These muscles run from the pubic bone and attach back toward the tailbone. Just like any other muscles in the body, the muscles of the pelvic floor have to be able to appropriately contract AND relax. A lot of my patients that present with pelvic pain, as well as many others with dysfunctional urinary or bowel symptoms, have difficulty relaxing their pelvic floor muscles. Let’s briefly separate these two conditions so we can understand why pelvic floor muscle relaxation is important for managing pain and dysfunctional voiding/emptying:
- Pelvic Pain: As we previously mentioned, the pelvic floor are a group of muscles that must be able to contract and relax. And just like any other muscles in the body, the muscles of the pelvic floor have nerves and blood vessels that run through and supply them. If your pelvic floor muscles are not relaxing as they should, this may impair the mobility and function of the nerves and blood vessels, causing pain. It’s kind of like flexing your biceps all day long – it would be painful, right? The same sort of rationale applies to contracted or high tone pelvic floor muscles. For patients with pelvic pain, I recommend that they practice their diaphragmatic breathing at least five to 10 minutes, one to two times a day. I also typically recommend that my patients try to incorporate their breathing throughout the day to help counteract all the tension they may be accumulating. Additionally, this is also a great tool to help manage flares in pelvic pain symptoms. You can further help facilitate pelvic floor muscle relaxation by practicing your belly breathing with different positions such as a deep squat or child’s pose.
- Dysfunctional Urinary/Bowel Emptying: If we take a look at the pelvic floor anatomy again, we can see that the pelvic floor muscles surround the openings of the urethra and anus. If the pelvic floor muscles are super tight or if they they are not able to appropriately relax down, it may be difficult to easily or completely empty the bladder or bowels. Oftentimes, if a patient has issues starting their flow of urine or difficulty evacuating stool, I have them practice their diaphragmatic breathing while on the toilet; (proper positioning with something like the squatty potty can also come in handy! As you start to do your deep breathing, the pelvic floor muscles should relax down, allowing your urethra and anus to more easily open.
How exactly does one perform a diaphragmatic breath?
- Lie on your back with your knees slightly bent and head supported. Place one hand on your chest and one hand on your abdomen. This little trick will help you know if you are performing the breath correctly.
- Breathe slowly through your nose and allow the air to flow from the thoracic cavity down to your abdominopelvic cavity. As you take your deep breath in, the hand on your chest should remain as still as possible, while the hand on your abdomen should rise. It’s important to note that you are not using your abdominal muscles to push out your stomach, but rather, allowing the air to fill the abdomen.
- Exhale slowly through your mouth and allow the abdomen to recoil back down to its resting position. The hand on your chest should continue to remain as still as possible.
Depending on how your pelvic floor muscles are resting, you may or may not be able to notice initially that your pelvic floor muscles are relaxing down with your breath. That’s okay! This should develop as you start to regularly practice your breath and become more in tune with your pelvic floor. You can also consult with a pelvic floor physical and occupational therapists who can give you cues/hints to help you become more familiar with how your pelvic floor is moving.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual appointments!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical and occupational therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical and occupational therapistss committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. The cost for this service is $75.00 per 30 minutes. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By: Admin
If you’ve recently been to your physical and occupational therapists, massage therapist, personal trainer, or body worker and heard the words “fascia” and “manipulation” in the same sentence, you are not alone. Fascia has become quite the buzzword for treating everything from chronic neck pain, ACL repair surgery, plantar fasciitis, and yes—even pelvic floor dysfunction. But what is fascia and how does keeping it healthy help you decrease shoulder pain AND pain with intercourse? The truth is that fascia is literally the entire body—head to toe we are covered in layers of connective tissue that surround our internal organs, our muscles, nerves, and bones. These layers of connective tissue are separated by a ground substance that is fluid and mobile, allowing our layers to slide and glide on each other to allow healthy and balanced movement. The structure of these bodily layers can be likened to the layers and sections of an orange to illustrate how fascia is a 3-dimensional network that houses and protects our internal structures: The superficial layers are much like that fuzzy, spider web-like layer just beneath the skin, adhered lightly to the layers below; the deeper layers are like the thin white sheath that separates the juicy flesh of the fruit from the outer layer. Now imagine a dehydrated, super tough orange that you spent 10 frustrating minutes peeling…that’s unhealthy connective tissue!
The complex nervous system of a human being allows us movement and cognition–so unlike an orange, we suffer from our immobile connective tissue by receiving its faulty nerve signals into our central nervous system which registers discomfort and pain. Understanding the manifestation of pain is a science in and of itself, and could fill blog posts from here until the next millennia; nociception, or how our brain perceives possible dangerous sensations through free-nerve endings in the skin, which helps protect us from harm. But often time there is the experience of pain long after the injury has happened and tissue healing time is far past–this is when pain becomes chronic and begins to affect everything in our lives. To learn more about brain and chronic pain check out this short 5 minute video, and then look up Dr. Lorimer Moseley and Dr. David Butler’s world renowned book developed from their research Explain Pain. The question is: how does fascia contribute to pain?
Research has shown in animal models and in humans that this complex layered system has multiple functions. Superficial and deep fascia act as padding and covering for protection of delicate structures such as nerves, blood vessels, muscles and bones. The composure of a layered system allows for sliding mechanisms, as multiple sheaths made up collagen, fibrin, and reticular fibers, separated by a unique fluid primarily composed of hyaluronic acid; and it is also considered a part of our nervous system.1,2 The deeper layers of connective tissue between the superficial retinacula and the muscle help maintain the fluidity of our movements. When thickening, or densification, occurs at a particular point in the connective tissue of the shoulder, the calf muscle, or the groin, where vital layers of connective tissue must glide, a pain response is usually created as the tissue pulls and rubs irregularly. The fascia uses a sliding structure to enable smooth movement; the fluid-like substance between layers contains hyaluronic acid is found to be more viscous is denser points of fascia—it begins to act more like honey, with the layers sticking together, creating faulty movement and faulty messages back to the spinal cord and brain.3 Because we now know that fascia is innervated with both free nerve endings and mechanoreceptors that respond to pressure and friction, we can better understand pain syndromes based on faulty joint movements that arise in the myofascial system, and why they are not detected on modern imaging modalities such as a CT scan or MRI.4
Deep fascia does not exist separately, but actually is strongly adherent to the muscles of the trunk. This means that approximately 30% of muscle fibers in the trunk are merged through the deep connective tissue and respond to the stretch and stress of your muscular contractions, which in turn stretch and activate fascial mechanoreceptors, igniting a neural feedback loop through the spinal cord to activate perfect movement.5 This “sense of space” and “recognition of tension” through the system is called “proprioception” and it allows us to perceive the depth and height of a set of stairs, have the ability to balance on one foot, catch a ball in mid-air, and regain our balance if we lose our footing. Antonio Stecco, MD, PhD, states that “fascia is the organ of proprioception,” which means that this previously unknown “organ” that encapsulates our entire being plays a lead role in knowing where your body is in space.6
You probably didn’t think you had another organ in your body, let alone an organ that literally is your entire body! It’s exciting to think that we are still discovering and exploring the intricate world of fascia and how it contributes to the nervous system. Dr. Jean Claude Guimberteau, a hand surgeon in France, conducted some of the first scientific studies on this “new” organ beneath our skin and created some of the most stunning video footage the world had even seen of what fascia actually looks like en vivo; check out this short clip to glimpse the complexity of our connective tissue.
How does this fascial system relate to my testicular or vulvar pain, burning and aching during sitting around the sit bones and tailbone, or my searing pain that I have every time I attempt intercourse?
Just as the muscle fibers are continuous with the deep fascia in the trunk, so are the layers connected to each other through central points of the body where increased force, movement, or friction may occur. As I mentioned earlier, we need the layers of connective tissue to slide and glide appropriately on each other with ease, and for this we need a healthy intracellular matrix that is fluid, i.e. less sticky, less dense and adhered. Once these layers build increased density—mostly to protect us from pain and unhealthy movement– and adhere to each other, we find decreased blood flow to the area, and decreased cellular exchange. This results in increased movement compensation, pressure, and pull on an already taxed system—like sitting on tight fascia around the delicate structures of the pelvic floor for 8-10 hours per day. At PHRC we treat both the superficial and deep fascia. See Stephanie Prendergast’s previous blog post on loose connective tissue and how pelvic floor physical and occupational therapistss treat superficial layers of fascia with skin rolling. PTs also treat the deeper layers of connective tissue where they interact with the muscle fibers—particularly muscles that connect to the pelvis bones, as well as the protective fascia housing the pudendal nerve and vital blood structures that reside near your sit bones. See Stephanie’s blog on how trigger point release helps regain normal muscle function and treat fascial pain.
So how can I get my fascia healthier? Once it’s stuck, can it get un-stuck?
Lucky for all of us the research on treatment for dysfunctional fascia is rich with new discoveries. Numerous un-embalmed cadaver dissections and scientific journal studies have helped to create the Stecco Method of Fascial Manipulation based on decades of clinical work by Italian physiotherapist, Luigi Stecco. This research is not the first to recognize the connective tissue matrix beneath the skin.In fact, early physicians throughout history have written in depth about the importance of this spidery substance—but it is not until now that the science has reached randomized control trials in the US to help show exactly how the fascial layers work as a system—creating “lines and planes” of movement that can be therapeutically treated as such. Essentially, Fascial Manipulation has discovered a series of specific points where the deep fascial layers coalesce to connect body segments to each other—much like acupuncture points that form meridian lines. These points, called Centers of Coordination, or “CCs,” are points that are replicable on each human body, laid out systematically in multiple movement planes, in order to treat the poor-gliding dysfunctions that occur in the connective tissue. When a practitioner palpates these specific places (sagittal, horizontal, or frontal) that elicit pain from the patient and reveal palpable restrictions, the treatment that occurs is deep pressure coupled with friction to the specific center of coordination (CC) until the pain decreases by greater than 50%. The treatment is performed only in a single plane of movement at one time (think forward-backward motions or lateral motions being separate treatments), and should trigger a deep ache that resolves into a low-level ache or soreness for a day or two afterward. The friction, causing heat, and the pressure, triggering mechanoreceptors in the tissue, ignites a cellular cascade that breaks down the coagulated hyaluronic acid—that “sticky” stuff I mentioned earlier—and leaves the patient with pain free movement. See Fascial Manipulation link here to learn more.
What’s up with those crazy scraping tools that leave me black and blue?
Other connective tissue treatments, such as IASTYM (Instrument Assisted Soft Tissue Mobilization), better known by the popular manual treatment devices Graston, leave the patient with visible skin discolorations and often deep bruising. IASTYM originates in Asia and is often called “Gua Sha,” translating to “rub” or “friction.” This scraping technique is believed to created fluid exchange, increased “ion flow,” and even “neutralize acidic conditions.”Although most of these claims have yet to be shown in scientific literature, it seems that fluid exchange within the extracellular matrix, may be a closer to the reality than previously thought.
…And those weird suction devices that leave purple dots on the skin—is that treating fascia?
If you watched the Summer Olympics you’ll see that sporting purple spots are en vogue! Those purple bruises are the signs of Myofascial Decompression which is a treatment applied to the layers of fascia using tools traditionally found in Acupuncture cupping techniques. Myofascial Decompression@, or MFD, is applied through a pumping action to create negative pressure and “suck” the fascia upward away from the deeper structures. MFD treats the dense connective tissue decreased mobility by drawing the tissue up into the cup and increasing tension on the surrounding tissue. The key difference between MFD and Acupuncture related cupping is that the patient is instructed to actively move the limb or trunk to stretch the fascia underneath the cups. When the MFD cup is released, a dark purple or red spot where it has been indicates an area that has been treated, leaving newly mobile and blood-flushed tissue in its place. In treating pelvic pain and scar tissue, physical and occupational therapistss will utilize MFD to help mobilize densified connective tissue around the bony pelvis to help relieve referred pain and increase healthy blood flow to the internal pelvic floor musculature.7
All of this sounds great, but pretty expensive…what tools can I use at home to treat my connective tissue?
Bust out that foam roller you’ve been hiding under your bed since you discovered your IT band just isn’t ever going to get less painful: that’s your fascial self-treatment tool! Foam rollers of all shades and densities have flooded the market, but regardless of how much of a glutton for pain you have become, I still am partial to the soft foam roller that Sue Hitzmann created during her launch of The MELT Method. Sue Hitzmann uses accessible language to introduce physiologically complex functions of the human body, and describes how fascia plays a vital role in maintaining a healthy nervous system. Similar to the Stecco Method, where there are key points of fascial treatment that relate to movement dysfunction, she describes specific movements performed on her soft foam roller and hand-foot treatment balls as ways to apply pressure, friction, and rinsing motions activate “the 5 R’s” of MELT: Reconnect, Rebalance, Rehydrate, Release, and Reintegrate to heal traumatized and painful fascia and the proprioceptive “body sense” within it. Her movements are applied in a system, linking them together in what she calls “body maps” for various pain syndromes, and always beginning and ending with a body scan linking the breath to the “neurocore”—a term she coined to explain how integral the diaphragmatic breath is to reintegrating healthy, pain-free movement back into the body.8 See Sue’s MELT Method page here.
The bottom line on fascia is that it encompasses your entire being,so embrace this previously esoteric substance that helps your movement be spot on and less painful when you finish your day. An important note is that we can actively or passively treat the fascia all day long, but healthy habits are still the key: Less time sitting on the back-line of connective tissue that travels from the back of your skull down past your pelvic floor, all the way to your toes; take walks, drink water, and explore how fascia can enhance your mobility and free you up for more delightful activities…and who knows, maybe a little hanky-panky with your partner won’t seem so daunting after all!9
References:
- Cowman M., et al. Viscoelastic Properties of Hyauronan in Physicological Conditions. F1000 Research. 2015, 4;622.
- Branchini M., et al. Fascial Manipulation for chronic aspecific low back pain: a single blinded randomized controlled trial. F1000 Research. 2015; 4:1208.
- Stecco A., MD, PhD. The Fascial Manipulation, Stecco Method. Level 1, lecture and lab. University of California, San Francisco. January 6-8, 2017.
- Stecco C, Gagey O, Belloni A, et al. Anatomy of the deep fascia of the upper limb. Second part: study of innervation. Morphologie. 2007;91:292:38-43.
- Stecco C, Gagey O, Belloni A, et al. Anatomy of the deep fascia of the upper limb. Second part: study of innervation. Morphologie. 2007;91:292:38-43.
- Stecco A., MD, PhD. The Fascial Manipulation, Stecco Method. Level 1, lecture and lab. University of California, San Francisco. January 6-8, 2017.
- DaPrato C, Kennedy C. Myofascial Decompression Techniques (MFD): A Movement Based Myofascial Course. Level 1 Course. University of California, San Francisco. March 14-15, 2016.
- Hitzmann, S. The MELT Method, First Edition. New York, Harper Collins; 2013.
- Raghavan P, Ying L, Mirchandani M, Stecco A. Human Hyaluronidase Injections For Upper Limb Muscle Stiffness in Individuals With Cerebral Injury: A Case Series. EBioMedicine. 2016;9:306-313.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Elizabeth Akincilar-Rummer
MEN!!! Are you ready?? Birth Control for men is here….almost.
Contraception. For some of us, that word has been a saving grace in preventing unwanted pregnancies and diseases. For others, it is fraught with moral and ethical dilemmas. But, those who are the most concerned with and often the most involved with contraception, are women. Let’s be real, women, versus men, take the brunt of birth control. And, maybe we should, since we are the ones who would have to endure 40 weeks of pregnancy and the birth of a child. Maybe the responsibility should be primarily on our shoulders. But, what about everything that occurs after the birth of a child? That lifelong responsibility of a child parents accept when they decide to conceive is on both parents, right? So, why wouldn’t the responsibility of birth control be for both the man and the woman? Good question. I think it should. I think we should have a choice. I think a couple should be able to decide, together, who should take on the responsibility of birth control.
Before you get your panties in a bunch, I know what some of you are going to say. You’re thinking, we already have a choice. Men can use a condom, they can use the withdrawal method, or they can undergo a sterilization procedure. Uh huh. Right. As if those are great choices. Let’s look at each option. Studies show that if you use the withdrawal method perfectly, 4 women out of 100 will get pregnant. If it’s done incorrectly, 27 out of 100 women will get pregnant. And, by the way, the withdrawal method is extremely difficult to do correctly if the man doesn’t have excellent self-control, men who ejaculate prematurely, and for men without a significant amount of experience. Condoms are 98% effective when used perfectly. Studies have shown that up to 40% of men use condoms incorrectly. And, sterilization isn’t an option for most couples since many of them will actually want to eventually get pregnant, and sterilization is not easily reversible. Where does that leave us? Not with a good choice, that’s where.
First, let’s just look at some numbers. How popular is birth control? Who uses it? I’ll tell you. Many, many, many women.
- 99% of sexually active women from 2006 to 2010 in the US used at least one form of contraception1
- 12 million women take oral birth control pills each year in the US2
- 89% of at-risk Catholic women, 90% of at-risk Protestant women, 83% of black women, 91% hispanic and white women, and 90% of asian women in the US use contraception3,4
What are the available birth control options available for women?
- Hormonal methods, such as the pill, patch, injectables, hormonal IUD, and the vaginal ring
- Non-hormonal IUD
- Read Jandra Mueller’s two-part blog post for the full story on IUDs: part 1 and part 2
What the possible side-effects for hormonal methods of birth control?
- Intermenstrual spotting, nausea, breast tenderness, headaches, weight gain, mood changes, decreased libido, vaginal discharge
- In some women, dyspareunia and pelvic pain
- Associated with increased blood pressure, benign liver tumors, and a slight increased chance of developing cervical cancer
- Increased risk of heart attacks, stroke and blood clots, which can be fatal
Are there hormonal birth control methods available for men? No.
Is it possible? Yes.
Let’s look at the history behind this curious absence in modern medicine.
Over the last century, many contraceptives have been introduced for women, yet not even one has been commercially introduced for men. Medicine has recognized the need for reversible and reliable birth control for men. It is agreed that a reversible hormonal method that suppresses sperm is the most practical implementation. Although reversible hormonal suppression of spermatogenesis (making sperm) was realized in the 1930’s, the first hormonal studies were only undertaken in the 1970’s. However, these feasibility studies were only further explored in the 1990’s. The studies in the 1990’s showed very effective and reversible sperm suppression, superior to condoms, and comparable to female contraception, with weekly testosterone injections.
In the last four decades, many studies have shown that hormonal suppression of spermatogenesis can prevent pregnancies, but development of commercially available products have stalled. Some of the early studies used supraphysiological doses of testosterone which had potential long-term adverse effects in healthy men. However, later studies found that the testosterone dose can be lowered by co-administering progesterone, essentially. However, there were only two studies that examined that method of administration.
The first study published in 2011 looked at administering progesterone and testosterone via an implant. It prevented 100% of pregnancies and was easily reversible. They did not report any serious adverse effects, but did report a high discontinuation rate among the participating men. This product was only a prototype and was not commercially available; therefore, it would require a significant amount of industrial research and development. They concluded that this study showed that male hormonal contraceptive products are considered medically and scientifically feasible.
The second study also published in 2011 also looked at administering progesterone and testosterone via an implant. They showed that 80% of the men in the study had a sperm count below the threshold of criterion for contraception. It also reported a high discontinuation rate among the participating men. They concluded that this study justified additional studies.
That brings us to the most recent study published in The Journal of Clinical Endocrinology and Metabolism in October 2016. The World Health Organization commissioned a trial that utilized a two hormone intramuscular injection to lower sperm count. The study included 10 study centers, worldwide, with 320 participants, but 100 continued users. They performed two intramuscular injections every eight weeks for up to four injection visits. The initial findings suggested a 96% effective rate with near complete suppression of spermatogenesis. They also showed that most of the participants returned to full fertility on an average of 26 weeks after discontinuing the injections. However, the Stage II Trial was interrupted due to reported side effects. The side effects reported were acne, injection site pain, increased libido, and mood disorders. The incidence of mild to moderate mood disorders was relatively high, but mostly in one of the study centers. Two independent safety committees evaluated the side effects and although they came to different conclusions, the study was terminated early. Since there was a difference in opinions from the two safety committees, the authors of this study feel that there is no definitive answer as to whether the potential risks outweigh the positive benefits in this study. The study also noted that while there is a risk for the men involved, albeit small, it is not a fatal risk, like that women risk by taking the birth control pill because of blood clots. It is important to note that for those that completed the first phase of the trial, more than 75% of the participants reported being satisfied and would be willing to use the product if it was available.
I wonder why one of the safety committees found the side effects so alarming that they had to terminate the study when hormonal birth control drugs for women cause similar and even more dangerous side effects, yet MILLIONS of women take the birth control pill every day. If we really want to compare dollars to donuts, one of the primary reasons this study was terminated was the adverse effect of mood disorders. I wonder if that safety committee is aware of this recent study published in JAMA psychiatry that reported 30% of women taking the birth control pill stopped taking it because of dissatisfaction secondary to side effects. They found that hormonal birth control was linked to a subsequent depression diagnosis and use of antidepressants. They also found a 40% increased risk of depression after six months of birth control pill use.
A few questions come to mind. Maybe safety committees have become more cautious compared to the time when many of the female hormonal drugs were being tested? Why aren’t there more studies examining male hormonal contraceptives? Why are the subject drop out rates so high in all of these studies? Why hasn’t there been any interest in commercially developing a product? Is it because the market research shows that men aren’t actually interested in such a product? Is there such a significant gender bias regarding birth control in our culture that there isn’t motivation to develop this product?
It seems that male hormonal contraception should already be a reality, but surprisingly, it’s not. I think a lot of women are more than ready to share the burden of contraception. The real question is, men, are you ready?
References:
- Daniels K, Mosher WD and Jones J, Contraceptive methods women have ever used: United States, 1982–2010, National Health Statistics Reports, 2013, No. 62
- WebMD, Comparing birth control pill types, accessed 26 February 2015.
- Jones J, Mosher WD and Daniels K, Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995, National Health Statistics Reports, 2012, No. 60
- Jones RK and Dreweke J, Countering Conventional Wisdom: New Evidence on Religion and Contraceptive Use, New York: Guttmacher Institute, 2011.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.