Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Shannon Pacella, DPT, PHRC Lexington
The pelvic floor is a phrase used very frequently here on the blog as well as in our clinics, but to those unfamiliar with this area of the body, it may still be this illusive mystery. I want to break down the pelvic floor into each of the muscles it is comprised of, in order for you to get a better grasp of what’s going on down there.
If you are partial to 3D visuals and videos, you can Take a Tour of the Pelvic Floor.
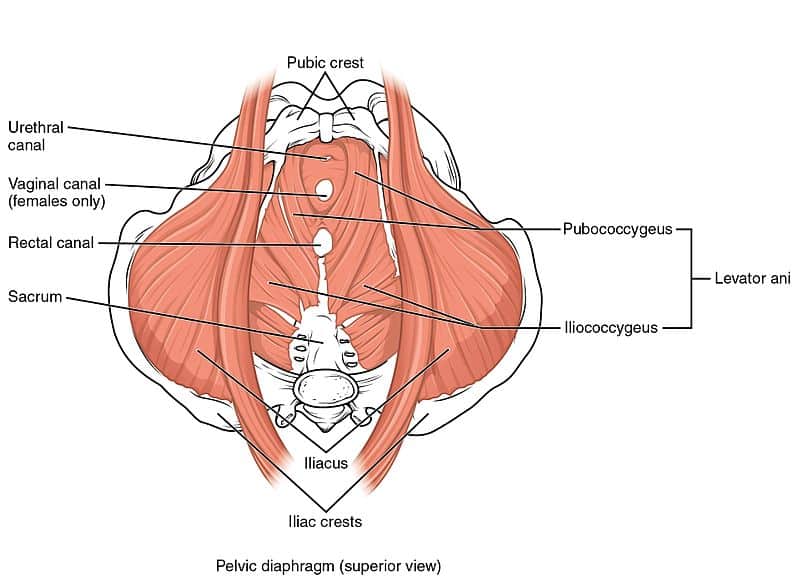
The pelvic floor is comprised of multiple layers of muscles that close off the bony frame of the pelvic outlet and are key in supporting the pelvic organs. To quote from our previous blog post: A Cock in the Hen House: A look inside the Male Anatomy, “Although the external anatomy is different, all the other internal muscles that make up the pelvic floor are the same for men and women. The muscles sit in the pelvis like a muscular bowl, providing support to the organs of the pelvis and assisting in bowel, bladder, and sexual function. In women, the pelvic floor supports the uterus, the bladder, and the colon. In men, the pelvic floor supports the prostate as well as the bladder and the colon.”
First let’s discuss the bones that make up the pelvis/pelvic girdle. The pelvic girdle is a basin-shaped ring of bones connecting the vertebral column to your femurs. The pelvic girdle contains and protects the pelvic organs and allows for attachment of the pelvic floor muscles.
The pelvic girdle is comprised of:
- Ilium: the largest pelvic bones – when you put your hands on your hips you are touching the ilium.
- Ischium: the part of the pelvis that you sit on (aka sit bones).
- Pubis: the front part of the pelvis that joins both sides together via the pubic symphysis.
- Sacrum: the sacrum attaches to the ilium via the sacroiliac (SI) joint.
- Coccyx: also known as the tailbone, and attaches to the lower part of the sacrum.
Now that you have some reference material, let’s go through each muscle one by one:
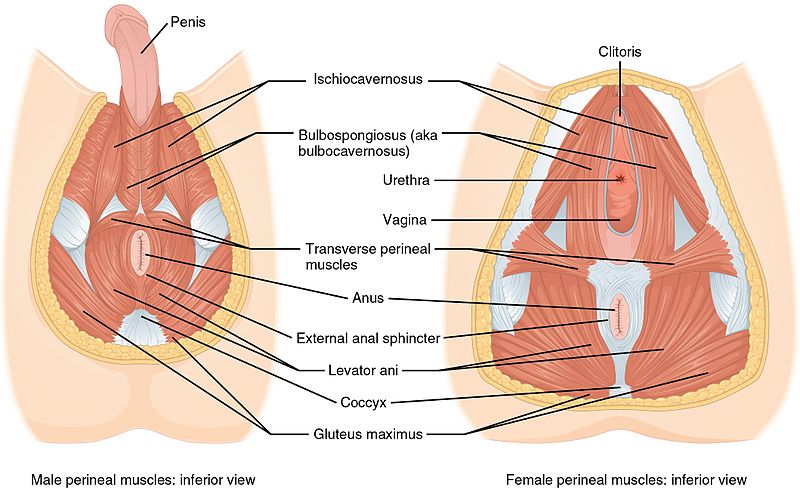
- Bulbospongiosus: in men, this muscle runs along the underside of the base of the penis and forces blood into the penis during erection, and aids in ejaculation. In women, this muscle runs from the clitoris to the perineum along each side, constricts the vagina, and forces blood into the clitoris.
- Ischiocavernosus: attaches from the pubic symphysis to the ischial spine on each side, and forces blood into the penis and clitoris during erection.
- Superficial & Deep Transverse Perineal: this muscle has superficial (thinner band) and deep (broad) fibers that run underneath the perineum – the space between the anus and vagina (in women) or base of penis (in men). Supports the prostate and vagina.
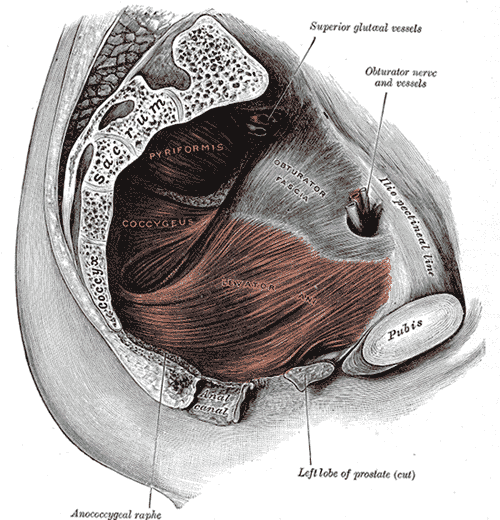
- Ischiococcygeus (aka Coccygeus): attaches from the tendinous arc of the ischial spine to the lower sacrum and coccyx. Moves the coccyx forward and supports the pelvic viscera.
- Levator Ani is a group of muscles (highlighted above in red) comprised of:
- Pubococcygeus: attaches from the pubis to the lower sacrum and coccyx.
- Iliococcygeus: connects with pubococcygeus muscle and attaches to the coccyx.
- Puborectalis: wraps around the rectum to form a muscular sling.
- External Anal Sphincter: attaches to the tip of the coccyx and surrounds the anal canal. This muscle closes the anal orifice.
- Obturator Internus: attaches from the pubis and ischium to the femur, helps to turn your hip outward (lateral/external rotation). *Fun fact: tightness and/or trigger points in this muscle can refer pain to the coccyx/tailbone.
- Piriformis: muscle deep in the buttocks (underneath gluteals), attaches from the sacrum to the femur, also works to rotate the hip outward (lateral/external rotation). Tightness in this muscle can be linked to sciatica (nerve pain down the back of the thigh), due to its proximity to the sciatic nerve.
Whew! That was a lot of information to get through! Now that you have a better understanding of what the pelvic floor looks like, let’s go over some ways this complex area of the body may lead to pelvic floor dysfunction in men and women.
Pelvic Pain
- Vaginal/penile/scrotal/perineal or anal pain
- Tailbone/sacroiliac joint/pubic symphysis pain
- Pain that interferes with sitting and exercise
- Pain that radiates to the abdomen/buttocks/thighs
Urinary Dysfunction
- Urinary urgency, frequency, and hesitancy
- Urinary retention
- Pelvic organ prolapse & incontinence
- Decreased force of urinary stream
- Pain/straining with urination
Bowel Dysfunction
- Constipation
- Fecal Incontinence
- Pain/straining with bowel movements
Sexual Dysfunction
- Pain with intercourse/penetration
- Pain post ejaculaton
I hope this helped to give you a better understanding of the pelvic floor anatomy.
References:
- Carriere B, Feldt CM. The pelvic floor. Germany: Georg Thieme Verlag; 2006.
- Netter FH. Atlas of human anatomy. 6th ed. Philadelphia, PA: Elsevier Inc.; 2014.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Admin
If you don’t know what or where your coccyx is, count yourself lucky. This little bone can make quite a ruckus when it’s not happy, often called coccydynia. The coccyx, or tailbone, is our little vestigial tail, after eons of evolution. It is often ignored and forgotten by most, but to me, it’s one of the most important bones in the body. Today we’ll go over why the coccyx matters and how it plays a role in pelvic pain, muscle tightness, nerve issues and even your neck movement!
#1) The coccyx: small but MIGHTY rudder
The coccyx is a tiny bone that joins with the pelvis at the sacrum to create the sacrococcygeal joint. Despite popular thought, the sacrococcygeal joint is mobile in many people. This joint varies from synovial (maximal mobility), to fibrocartilaginous (moderate mobility), to ossified (no mobility).1 Also, it is not unusual to have a small articular disc at the sacrococcygeal joint to help with this movement. Research has documented normal coccygeal movement is between 5-25° from standing to sitting.2 So, the coccyx can move. The location of the coccyx, at the base of the spine, and its ability to move can have far reaching implications on the rest of the body. For example: a change at the coccyx changes how the sacrum and pelvis moves. The pelvis is the body’s center of mass, so where the pelvis goes the body goes. Who would think such a little rudder could steer such a big ship?
#2) The coccyx: central attachment point of fascia, ligaments and muscles
The coccyx is also a central attachment point of fascia, muscles and ligaments on the inside and the outside of the pelvis. I mean, just look at all those beautiful muscles. And check out these ligaments!
So, if you imagine, a coccyx off-axis may create some problems. Let’s just take the pelvic floor muscles as an example. If, say, the coccyx is pulled over to the left, all the pelvic floor muscles attached to the left side of the coccyx will get short and weak, while the ones on the right will get stretched out and weak. This could lead to decreased “core” strength (pelvic floor is part of the “core”), incontinence (urinary or bowel) and/or pain (bowel, bladder, sex, exercise). The ligaments that attach to the coccyx also provide passive stability to the pelvis, primarily at the sacroiliac joint. A shift at the coccyx could create ligamentous tension, leading to the same problems. Some of these ligaments, like the anterior longitudinal and supraspinal ligament, even run all the way up to the head and neck! You can imagine how childbirth, a fall or throwing your back out could create a problem, not only locally at the tailbone, but further up or down the chain.
#3) The coccyx: base of the nervous system, MAGIC
This may be one of the more magical things. The spine houses the spinal cord. The spinal cord is the brain’s extension to the rest of the body. It starts in the skull, runs the whole spine and then attaches to your coccyx. The filum terminale (pictured above as Terminal filum), is the final thread of spinal cord that secures itself to the first coccygeal vertebra. Sometimes, if there is stiffness in the spine or at the coccyx itself, it can impact the mobility and health of the nervous system. When this happens the body may become protective in order to keep the nervous system safe. Often this protection can create symptoms of numbness and tingling, or a tightness that does not resolve after normal healing time. Examples of this would be a “hamstring tear” or “adductor strain” that has never fully healed. Often, the tight “muscle” is actually an unhappy nerve, and stretching it may feel good in the moment, but afterward worsens the symptoms. Treating the tailbone is one aspect, along with a multitude of other rehabilitation techniques, to improve the health and mobility of the nervous system.
#4) Oh Coccyx, My Coccyx
So, what to do with all this information? Well, hopefully be a little more thoughtful to your coccyx, it’s a cool little bone. Nice things you can do for your coccyx include: proper sitting posture, pelvic clocks, or even just going for a gentle walk to get some blood flow. And, if you’ve got pain down there, be sure to see your local pelvic floor PT or come visit us to get that tail wagging again!
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual appointments!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical and occupational therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical and occupational therapistss committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. The cost for this service is $75.00 per 30 minutes. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
References:
1.Lee DG, Lee L-J, Vleeming A, Jones MA. The pelvic girdle: An integration of clinical expertise and research. 4th ed. Edinburgh: Elsevier/Churchill Livingstone; November 17, 2010:24-25.
2. Fogel G, Cunningham P, Esses S. Coccygodynia: evaluation and management. J Am Acad Orthop Surg.2004;12:49–54.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
As a physical and occupational therapists specializing in pelvic floor disorders, specifically pelvic pain, I have noticed a strong correlation between chronic pain, the thyroid, and the endocrine system. I wanted to explore what hormonal imbalances can do to chronic pain. I won’t go into too much detail about persistent pain here, instead please refer to the blog post Pain as the Ultimate Protector to get a quick refresher. Pain was once believed to be a signal of tissue damage, but now, the understanding is that pain is not so specific. Persisting pain is complex and signals are sent from the brain to the body and from the body to the brain. Pain can build in intensity varying on many factors including, fear, stress, systemic inflammation, hormonal and autoimmune issues, or history of a trauma.
The thyroid is a major player in the endocrine system and there is a link between elevated muscle enzymes and creatinine in the blood which can influence chronic muscle fatigue/pain. During an abnormal stress response, which is associated with chronic pain, dysregulation of the adrenals occurs resulting in chronic pain and fatigue. Chronic pain of the musculoskeletal system is a common symptom of autoimmune thyroid issues. As a result, it is important to look at the endocrine system, adrenals, nutrition, and the musculoskeletal system when dealing with chronic pain. When the body is under a significant amount of stress whether it be with chronic pain, emotional stress, physical stress, etc the thyroid becomes compromised and is unable to keep up with the adrenal insufficiency or stress response. In most cases, the thyroid shuts down or becomes overactive, disrupting the homeostasis of your body. Let’s delve into the complex world of the thyroid or endocrine system, shall we?
Quick Facts about the Thyroid:
An estimated 20 million Americans have some form of thyroid disease, and up to 60% of those with thyroid disease are unaware of their condition. The thyroid is a hormone-producing gland that regulates the body’s metabolism. The metabolism is responsible for producing energy and it affects body functions such as heart rate and energy levels. The thyroid gland is relatively small, located at the middle/lower neck, and it produces hormones that influences every single tissue, organ, and cell in the body. The two most common conditions are hypothyroidism and hyperthyroidism. Hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormone. Common symptoms include: fatigue, increased sensitivity to cold, constipation, dry skin, weight gain, muscle weakness, muscle aches, tenderness, stiffness, pain/swelling in the joints, heavy or irregular menstrual periods, thinning hair, depression, slowed heart rate and impaired memory. Hyperthyroidism is a condition causing the gland to produce too much thyroid hormone. Common symptoms include rapid heart rate (tachycardia), heart palpitations, increased appetite, nervousness/anxiety/irritability, tremor, sweating, changes in menstrual patterns, increased sensitivity to heat, changes in bowel patterns, difficulty sleeping and brittle hair.
Hashimoto’s Disease occurs when the body’s immune system attacks the thyroid and destroys the body’s ability to produce hormones. Common symptoms are similar to hypothyroidism.
Graves’ Disease occurs when the body’s immune system attacks the thyroid, causing overproduction of the hormone responsible for regulating the metabolism. Common symptoms are similar to hyperthyroidism.
Thyroid Hormones:
Here is a very brief overview about the thyroid hormones that are important in regulating the body. Thyroxine (T4) is the major hormone secreted by the thyroid. T4 is then converted in the liver to T3 by the removal of an iodine atom. The important thing to note is the amount of T4 produced by the thyroid gland is controlled by another hormone called your thyroid stimulating hormone (TSH). This is produced in the pituitary gland located at the base of the brain. TSH is the most common thyroid level tested, however, it is important to have your T4 levels checked as well because the amount of TSH that the pituitary sends to the bloodstream depends on the amount of T4 in the pituitary. If the pituitary sees lower levels of T4, then it produces increased TSH so that the thyroid gland will produce more T4. You can think of TSH and T4 as a thermostat. When the heat rises to a balanced level, the thermostat senses this and then turns off the heat. Finally, it is important to note that pregnancy, oral contraceptive use, chronic pain, and autoimmune conditions can change the thyroid levels in the blood.
Thyroid Function Tests:
Thyroid functioning is tested through a blood test. The two most important thyroid levels to address are the TSH and T4 tests. Initially, the TSH level is the best way to see if your thyroid is producing what it should be. Then, combining that TSH test with the free T4 accurately determines if the thyroid gland is functioning. I don’t want to go into too much detail. To find out more information please click here.
Normal TSH levels are between .5 and 5.0, which is a wide range. It is important that your levels are closer to a one or two, especially if trying to conceive or if you have an autoimmune condition or chronic pain condition. A recent study was conducted to assess thyroid dysfunction in women of reproductive age and to see if thyroid dysfunction is associated with menstrual irregularities, anovulation, and infertility. The study showed that women who had TSH of less than 3.0μIU/mL had significantly better functional ovarian reserve than the group that had a TSH of greater than 3.0, which is still considered within normal range. From experience with my clients, many thyroid specialists do not think outside of the box and do not take the time to tailor thyroid treatments. If you are within the wide range, they often say you are okay. If you are having the symptoms of thyroid dysfunction and are at a 5.0 of TSH, even though it is “within the range,” you more than likely need a supplement to help support your endocrine system.
Thyroid Deficiency and Iodine:
The American Thyroid Association states approximately 40% of the world’s population is at risk for iodine deficiency. Iodine is an element that is needed when producing thyroid hormone. Because the body does not make iodine, it must be an essential part of your diet. It is found in various foods including cheese, cow’s milk, eggs, yogurt, saltwater fish, seaweed, shellfish and iodine containing multivitamins. This is especially important in the great lakes northwest regions of the US and Canada, where there was a major iodine deficiency in the 1920’s and people were treated with iodized salt to help with “goiter” and thyroid deficiency. These places continue to have decreased iodine in food and often people must take an iodine supplement in order to regulate thyroid conditions.
Some alternative ways to boost your endocrine system and regulate your body:
- Replace processed foods with whole foods
- Exercise regularly and it should be more weight bearing exercise
- Establish regular bedtimes and sleep
- Practice relaxation techniques,a great app is Headspace or Calm
- Avoid alcohol and stop smoking
- Avoid/limit sugar consumption
- Identify food intolerances or sensitivities (we usually crave foods we are sensitive to)
Because of all these factors that affect intensity of pain, it is important to look at an integrative approach.
- It is important to recognize that your pain is a signal that something is out of balance.
- If you have chronic pelvic pain, seek a pelvic floor specialist to help guide you in the right direction to attack the musculoskeletal component.
- Adrenal fatigue/autoimmune thyroid conditions are common with chronic pain.
Finally, when finding a thyroid health care practitioner/endocrinologist/naturopath, it is important to find someone who looks at the “whole body” and is open to finding the right thyroid treatment for you.
Resources:
- http://www.thyroid.org/media-main/about-hypothyroidism/
- https://www.ncbi.nlm.nih.gov/pubmed/16382004
- http://www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/dxc-20155382
- http://www.thyroid.org/iodine-deficiency/
- https://rbej.biomedcentral.com/articles/10.1186/s12958-016-0162-0
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.