Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Jandra Mueller
Are you currently on birth control? Have you used birth control in the past? These are common questions I ask when doing an evaluation of a female patient who is experiencing painful intercourse, also known as dyspareunia. Most women I see are currently, or have been in the past, on some form of birth control. Typically they are prescribed initially for non-contraceptive related reasons starting in adolescence for skin conditions (acne), painful or heavy periods, or mood disorders, and then just continue using them once they become sexually active.
I’ve evaluated many women, both young and old, that have a history of using at least the pill, but many whom have also reported using other various types of birth control like the patch, the Depo-Provera shot, or the NuvaRing. Most of the reasons reported for switching birth controls were not because they weren’t effective in preventing pregnancy, but because there were individual intolerances to the various forms, like extreme mood shifts, abnormal bleeding, weight gain, headaches, changes in energy levels, diminished sex-drive, vaginal dryness and breast tenderness. Another big reason women switch from the pill to, lets say the patch or the ring, is the convenience of not having to remember to take a pill every day at the same time, especially if that is the only medication you take. This becomes a disaster when you miss 2-3 pills and have unprotected sex – you fear an unwanted pregnancy and you end up taking the plan-B pill “just-in-case.”
Here are some common responses (and the reasons) women often report trying all sorts of different birth control pills or methods or eventually why they stop using birth control all together:
- Compliance “oh, I just kept forgetting to take my pill”
- Adverse reactions “I’m so sensitive to hormones,” “I’m an emotional wreck,” “I hated the way it made me feel,” “I gained so much weight”
- Sexual changes “I lost my sex drive,” “I feel dry down there”
If some of these sound familiar, you are not alone. To make matters worse, recent research suggests that oral contraceptive birth control pills can cause vulvodynia, as well as other side-effects such as recurrent UTIs (or symptoms of UTIs), yeast infections, or the menopausal state in which our bodies are temporarily in. This is also true of other forms of birth control such as the depo shot, NuvaRing, or the patch. For more information on how birth control wreaks havoc on our bodies, check out Dr. Gonzalez’s blog here.
When our doctors counsel us on the use of these medications, they are understandably concerned with the life-threatening effects of birth control, such as blood clots and effectiveness of the type of contraceptive which can change based on weight. What doctors often do not mention is since your ovaries are essentially shut down to prevent pregnancy, your body will also stop the production of very important hormones like estrogen, progesterone, and testosterone, which can significantly decrease your sex drive, and cause dryness and irritation in your vagina. This can make sex painful because your tissues stay chronically irritated, which can put you at risk for recurrent UTIs and yeast infections, and your clitoris and labia may shrink in size.
Yikes! I know 100% that I wouldn’t volunteer to take this pill knowing that information. Guess what? Like many of you who are reading this blog, I’ve taken the pill for many years, unknowing of the consequences. My first experience with the pill was when I was 13 years old, after my mom took me to the ER because I ended up curled up in the fetal position in the bathtub from relentless stabbing, knife-like pain in my lower abdomen. I was diagnosed with a ruptured ovarian cyst with multiple cysts still present in my ovaries. The treatment: oral contraceptives.
For the next 7 years of my life I tried multiple forms of the pill as well as the NuvaRing. It was a struggle to find the right fit for me. I was on and off birth control because of weight gain and extreme mood swings, though when I became sexually active I worried about unwanted pregnancy so I’d return to the pill or the ring and the cycle would continue. When I was 20 years old I was in a serious, monogamous relationship and I couldn’t think about the side effects of using one of these methods on the regular, it was just not an option – I needed something different. Then my Ob Gyn offered Mirena, an IUD.
What is Mirena?
Some of you reading may have heard of Mirena, but don’t be alarmed or feel you are out of the loop if you haven’t! Mirena is a levonorgestrel releasing intrauterine device (IUD) that is FDA approved for use up to 7 years.10 At that time it was the only hormone releasing IUD approved for use in the United States.
IUDs are forms of long acting reversible contraception (LARC), and are T-shaped flexible devices made from either copper or a backbone. They release small amounts of levonorgestrel, a type of progesterone, throughout either a 3- or 5-year period. They are known to be the safest and most effective forms of birth control in preventing unwanted pregnancies.1 They were initially designed for women who were seeking birth control after they had a baby; but due to the high effectiveness in preventing unwanted pregnancies, they are the first line choice of birth control for all women – baby or no baby, teenager, young, or old according to the American College of Obstetrics and Gynecology.1
Naturally, my follow up question during my evaluation is “Have you considered using an IUD?” The responses here are mixed but overall they aren’t in favor of the IUD. Here are some answers I’ve heard:
– “My Ob/Gyn never told me about it”
– “My doctor said it would be too painful to insert it”
– “My doctor said it isn’t a good option because I haven’t had a baby”
– “I thought I couldn’t have one because I haven’t had a baby”
– “It’s weird to have something in my ‘vagina’ for that long”
– “Oh yeah, my friend told me it hurt really bad when she got it and she bled for a really long time”
– “I’m worried about getting cancer”
– “I’m worried it will get lost”
For those of you who have heard of the IUD or have asked your doctor about them, do any of these responses resonate with you?
What is considered a long acting reversible contraception and why have I not heard of them?
Like I mentioned earlier, an IUD is a form of a LARC and they are considered to be the first line choice of contraception for all women. ACOG released a statement in Sept/Oct 2015, which urges obstetrician-gynecologists to encourage use of a LARC device, educate patients on their options in LARC devices, and advocate for insurance coverage, payment, and reimbursement.
The use of LARC devices in adolescents and young women was initiated due to the high rate of unintended pregnancies, mostly due to inconsistent use with other forms of contraception in this population, which has become a significant public health concern. Think about it, it’s a hassle to remember to take a pill at the same time every day or to make sure you schedule your doctor appointments on the regular to get your depo shot every 3 months or re-fill your prescription for the patch or the ring. In addition to the compliance issue, there is also a higher failure rate of these methods – 9% with the pill, patch, and ring and 6% with the shot, compared to 0.2-0.8% with LARC devices.2
My question now is, if this is THE thing to have, research shows that it is the safest, most effective, and the device recommended by ACOG, why am I seeing all these young women still on the pill with very little knowledge about an IUD? Statistically speaking, less than 10% of all U.S. women use a form of LARC as their method of birth control, and only 4.5% of women under 20 use a LARC device3 most commonly the IUD. The percentage of women who use contraception and an IUD as their method are much higher in other countries. For example: Asia (27%), Europe (17%), Africa (15%), Latin America/Caribbean (9.6%) are all ahead of us in using these forms of devices.4
The biggest reason stated is that Ob Gyns may not have the most recent evidence on IUDs and even ObGyns who have a favorable attitude towards IUDs may use overly restrictive criteria when recommending an IUD to an adolescent or nulliparous women, meaning women who have not had babies. Studies show that approximately 67% of Ob Gyns consider a woman who has not yet had a baby an inappropriate candidate for an IUD, and 43% of Ob Gyns feel this is true of adolescents.5
Now that you know some information about LARC devices, let’s talk about what they actually are.
There are two categories of LARC devices: the implant and the IUD.
The Implant – Nexplanon
Nexplanon is the implant that is FDA approved for use in the US. It is a small device that is inserted into your arm and can last up to 3 years. It works by slowly releasing a hormone called etonogestrel, a type of progesterone, into your bloodstream and stops ovulation. The implant differs from short acting reversible contraception (SARC) aka the pill, the patch, the shot, and the ring, in that it does not contain ethinyl estradiol (synthetic estrogen).
This is an important difference to understand. What this means is that due to the lack of the synthetic estradiol, in the process of preventing pregnancy it does not shut the ovaries off from producing other sex hormones like estrogen and testosterone. However, because it is inserted in your arm, the synthetic progesterone gets released into your bloodstream and has to go through your liver to be processed (similar to other systemic forms of contraceptives). Similar to OCPs, this process causes an elevation of a protein called sex hormone binding globulin (SHBG), which is produced by our liver once our liver metabolizes, or breaks down, the synthetic progesterone.
SHBG basically sucks up all of our available or free testosterone rendering it ‘inactive.’ In short, testosterone is really important for the health of our tissues ‘down there,’ and can ultimately be responsible for those side effects such as low energy, diminished sex drive, poor tissue health, vaginal dryness, as well as conditions known as vulvodynia, vestibulodynia, and dyspareunia. To read more about SHBG check out these blogs.
The implant was ultimately designed to be a more convenient form of birth control that could release a steady state of hormone over a longer time period without interrupting a woman’s ability to get pregnant once she decided to go off contraception. It is very effective in preventing pregnancy, which is what your Ob Gyn is ultimately concerned about. However, though it is better than other forms of contraception because of the lack of synthetic estrogen, it is not the BEST option considering it still raises your SHBG, which puts you at risk for developing some of those nasty side effects.
The IUD – Paragard, Mirena, Skyla, and Liletta
Again, an IUD is a flexible T-shaped device that is inserted into the uterus (not the vagina). There are now 4 IUDs that are FDA approved for use in the United States. One of the IUDs is a copper releasing device (ParaGard) and the others are levonorgestrel-releasing IUDs (Mirena, Skyla, and Liletta).
According to a study that looked at differences in the effect of age, parity, device type on expulsion, perforation, or failure (unintended pregnancy), they showed no difference in these areas in adolescents or in nulliparous women. The only differences they found were with the copper IUD causing increased pain and was more associated with higher rates of expulsion and premature discontinuation. (7) What I also found that was interesting about this article is they looked at the type of providers that were placing the IUDs. Often a family practice or nurse practitioner you may see for your annual exams are the ones who place the IUD and there have been shown to be more complications with non-OB Gyn practitioners who are performing the insertion.7
If you would like more information on the use of a long-acting reversible contraceptive device, contact your Ob Gyn office to make an appointment and discuss this option. Stay tuned for more detailed information regarding the different IUDs and why we believe an IUD is a superior choice over the implant.
Stay tuned for next week’s blog on more IUD differences and questions to discuss with your physician.
References:
- Adolescents and long-acting reversible contraception: implants and intrauterine devices. Committee Opinion No. 539. American College of Obstetricians and Gynecologists. Obstet Gynecol 2012;120:983–8.
- Trussell, J. Contraceptive failure in the United States. Contraception. 2011;83(5):397-404.
- Teal SB, Romer SE, Goldthwaite LM, et al. Insertion characteristics of intrauterine devices in adolescents and young women: success, ancillary measures, and complications. Am J Obstet Gynecol 2015;213:515.e1-5.
- Buhling K, Zite N, Lotke P. Worldwide use of intrauterine contraception: a review. Contraception 89 (2014) 162-173.
- Usinger K, Gola S, Salas M, Smaldone A, Intrauterine Contraception Continuation in Adolescents and Young Women: A Systematic Review, Journal of Pediatric and Adolescent Gynecology (2016), doi: 10.1016/j.jpag.2016.06.007.
- Benacerraf B, Shipp T, Lyons J, et al. Width of the Normal Uterine Cavity in Premenopausal Women and Effect of Parity. Obstet Gynecol 2010;116(2):305–10.
- Aoun J, Dines V, Stoval D, et al. Effects of Age, Parity, and Device Type on Complications and Discontinuation of Intrauterine Devices. Obstet Gynecol 2014;123:585-92.
- Rose S, Chaudhari A, Peterson M. Mirena® (Levonorgestrel intrauterine system): A successful novel drug delivery option in contraception. Advanced Drug Delivery Reviews 61 2009;808-812.
- Hall AM, Kutler BA. Intrauterine contraception in nulliparous women: a prospective survey. J Fam Plann Reprod Health Care 2016;42:36-42.
- Rowe P, Farley T, Peregoudov A, et al. Safety and efficacy in parous women of a 52-mg levonorgestrel-medicated intrauterine device: a 7-year randomized comparative study with the TCu380A. Contraception 93 (2016);6:498-506
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
When I was younger, the phrase “You are what you eat,” totally confused me. Doughnuts are so delicious and sweet, therefore if I eat a half dozen of glazed old fashioned doesn’t that mean that I would also be sweet and highly desirable? Obviously, I now know that my logic as a kid was inaccurate, otherwise I would still be on a doughnut and milkshake diet. I now know the importance of healthy eating and the benefits of fruits and veggies.
This discovery came from my own health journey, which may sound familiar to many of you. No doctor could figure out why I had horrible abdominal pain. I had constant fatigue and headaches. I underwent a plethora of tests, but no one could give me any answers. Thankfully, my mom (the wisest woman I know) suggested I do a food journal to see if something in my diet was the problem. After, only a few days of tracking my diet, I noticed several unhealthy trends. I began researching strategies to improve my diet and began to notice improvement in my health and less symptoms overall. I was amazed that something as simple as eating more “green things” could make me feel better. In reality, it makes so much sense. What we supply our body with will impact how it will run. For me, I was not being mindful of what I was eating or buying at the grocery store. Since the frozen food and packaged items I purchased were labeled as organic or vegan then I assumed that they must be good for me. No wonder my body hurt so much, I was not feeding it anything of substance! This experience made me to want to know more about how diet can impact not only myself, but my patients as well.
I was fortunate to learn about how nutrition can play a role in patients with pelvic floor dysfunction as I recently completed a certification program as a Women’s Health and Nutrition Coach through the Integrative Women’s Health Institute. The integrative Women’s Health Institute was founded by Jessica Drummond, a pelvic floor physical and occupational therapists and a health coach with a certification in clinical nutrition. Jessica founded the Institute to help educate professionals and patients about functional nutrition and its role in pelvic health and pain disorders. The programs Jessica offers are very informative and in-depth, so there is no way to share all of the information in one blog post, but there are a few key tidbits that I feel everyone could benefit from.
First, every person is unique, therefore when it comes to diets there is no one size fits all. What one person may lack and therefore require in nutrients, another person may have in abundance. I recommend that one consult with an integrative medical provider, naturopath or dietician before making any drastic changes to their diet. Lab tests may be helpful in determining if you are deficient in certain vitamins, which can help you and your provider decide foods that can be helpful in correcting the deficit.
Rule out food sensitivities. If you read Liz’s blog post on the gut microbiome, you may recall that the gut plays a huge role in immune health. So, if certain foods irritate the lining of the gut, it can result in an overall inflammatory response that is not just limited to the gut region. If a person continues to eat a food that they are particularly sensitive to, it can lead to chronic inflammation that can lead to pain anywhere in the body, such as the pelvis. For some people, food sensitivities can present as fatigue, skin conditions such as eczema, brain fog, nausea or headaches to name a few.
So, how does one determine if they have any food sensitivities?
If only there was an app for that, where when you swipe right for cheese and hope that you get a notification that you were a match! In the meantime, there are two options. One is a blood test can look for different inflammatory markers that can be related to food sensitivities. The other is the gold standard in terms of effectiveness: an elimination diet.
The name should hopefully explain the process. You eliminate all foods that are most likely to cause food sensitivities for at least 3 weeks. Drummond recommends eliminating the following: gluten, dairy, soy, eggs, corn, beef, citrus fruits, peanuts, coffee, baker’s yeast, potatoes, onions and nightshade vegetables. After the 3 weeks have passed, you add one item back into your diet for 1-4 days and then remove it and monitor your symptoms. If you experience symptoms, wait until the symptoms resolve before you add a different food back in. If you identify an item that you are sensitive to, you must eliminate it from your diet for 3-6 months. This would be the time to add in gut healing foods, such as bone broth, which is high in glutamine an amino acid that supports gut epithelial health. You can make your own bone broth or you can order it online here or here. You may still be stuck on the list of foods you need to eliminate on the diet and if you are like me are thinking What the heck am I supposed to eat?! Lots of things: Organic hormone-free lean protein such as chicken or salmon, leafy greens, apples, avocados, beans and lentils. It may seem like a daunting task, but the results gained from doing an elimination diet should make it worthwhile.
One final note regarding food sensitivities, if you suspect you may be gluten intolerant or have Celiac’s Disease you should consult with a medical provider, as the testing to rule out this disorder requires ingesting gluten versus eliminating it.
.
So let’s say you’ve done an elimination diet or maybe you aren’t ready to do one or don’t feel that it is beneficial for you and you want to know what else can you do to support your body and decrease inflammation related to your pelvic floor dysfunction.
- Drink water! Your body needs water to stay hydrated, to flush out toxins and keep your colon happy. Dehydration can lead to bowel dysfunction, primarily: constipation. Constipation can play a huge role in contributing to pelvic floor dysfunction. Stephanie talked about this in more detail in a previous blog post. Previously, everyone lived by the rule of 8 cups of water a day. That is a great way to start, but not everyone needs the same amount of water. The new rule of thumb is to drink the amount of water best suited for your body weight. You should take your weight and divide that number in half and the result is the amount you should drink in ounces. For example: If you are 200 pounds, you should ideally drink 100 ounces of water a day. For every 30 minutes you exercise, you should add in an extra 8-12 ounces. Other factors may require you to increase your water intake such as being pregnant, if you are breast-feeding or undergoing different medical treatments such as chemotherapy.
- Eat real food. In order to help your body function to it’s full potential, you need to feed it high quality, nutrient dense food. Try to stick to organic fruits and vegetables and grass fed, organic and hormone-free meat. Some examples include cruciferous vegetables, broccoli, avocados, wild salmon and other lean proteins, and lemon. Avoid processed foods, frozen meals or meal replacement bars. They often contain high amounts of oil, sugar and fat and very little fiber or nutrients. Some processed foods can contain large amounts of chemicals which are used to add flavor or prolong the shelf life of the item. For all of those reasons, processed food can lead to the inflammatory process I discussed above.
- Limit your sugar intake. Increased sugar consumption can lead to elevated cortisol (a stress hormone) levels which can have a negative impact on your sex hormones. Elevated cortisol can cause a bunch of other symptom such as headaches, sleep problems and weight gain.
- Spice up your life! Certain spices such turmeric, garlic, ginger, oregano, cloves, dill, sweet basil and cinnamon have anti-inflammatory properties. Be mindful that certain spices, such as pepper, are nightshades and can be irritating for some people. Other anti-inflammatory foods include: Lime zest, button mushroom, oyster mushroom, onion, sweet potato, parsley
Now that is definitely not everything you need to know, and it is certainly not the solution for everyone’s pelvic dysfunction. As we know, chronic pain is not something that can be treated with a magic pill. It usually requires a multi-disciplinary approach with different providers and interventions being utilized. A person’s diet can often be forgotten when discussing strategies to treat pelvic pain and dysfunction. Changing one’s diet does not mean it will eliminate one’s symptoms, but it can certainly help supplement other treatment modalities.
Want to learn more? Check out the following resources for more information:
The Elimination Diet: Discover the Foods That Are Making You Sick and Tired–and Feel Better Fast by Tom Malterre MS, CN and Alissa Segersten
The Integrative Women’s Health Institute: http://integrativewomenshealthinstitute.com/
Prescription for Nutritional Healing by Phyllis A. Balch
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Admin
The Kegel, the black box of the exercise world.
Are you really doing it right?
In today’s post we are going to review some simple exercises to help get to know the pelvic floor muscles. Now, I strongly recommend going through my past post “Exercises for Short/Tight Pelvic Floor” first. Generally speaking, patients with pelvic pain should not kegel as a therapeutic exercise. Kegel exercises may be better suited for postpartum women or those with prolapse or stress urinary incontinence, but not always. Of course, a pelvic floor physical and occupational therapists is the best judge of where you fall on the spectrum of pelvic floor muscle function and if you need to lengthen or strengthen your muscles. With that said, this post is to teach people, who should kegel, how to kegel.
Okay, that said I will proceed. Remember, if you have any discomfort or negative change in function, stop the exercises and go find your nearest friendly- neighborhood pelvic floor PT.
So, Dr. Kegel had a reasonable idea. Let’s have people, women mostly, start strengthening the muscles of their pelvis so they don’t have to have surgery and can do self rehab. Now, barring the fact that many people, women and men, don’t need to do Kegels, there was one other fault to this idea. Pelvic floor muscles are intricately connected to the rest of the body, meaning a kegel by itself can’t do very much. Its isolation limits its power. Using other muscles can help facilitate a full pelvic floor contraction and core recruitment. Ideally, this should occur automatically, but we’ll talk about that another day. So, we’ll start with some basic individual muscle contractions of the pelvic floor then move to more integrated exercises. To understand this a bit more take a look at what Diane Lee says about the “core”.
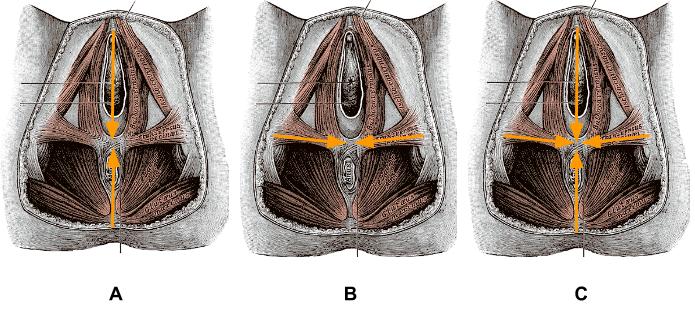
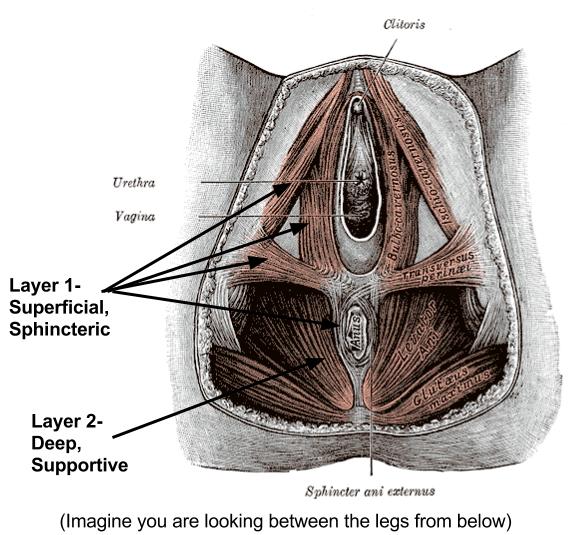
Week 1: Synchronizing Superficial Sphincters!
So let’s start with the first level of the pelvic floor, the most superficial (most close to the surface). This is the sphincter work. You can try 1-2 sets of these a day for a week just to get the sensation of recruiting these superficial muscles.
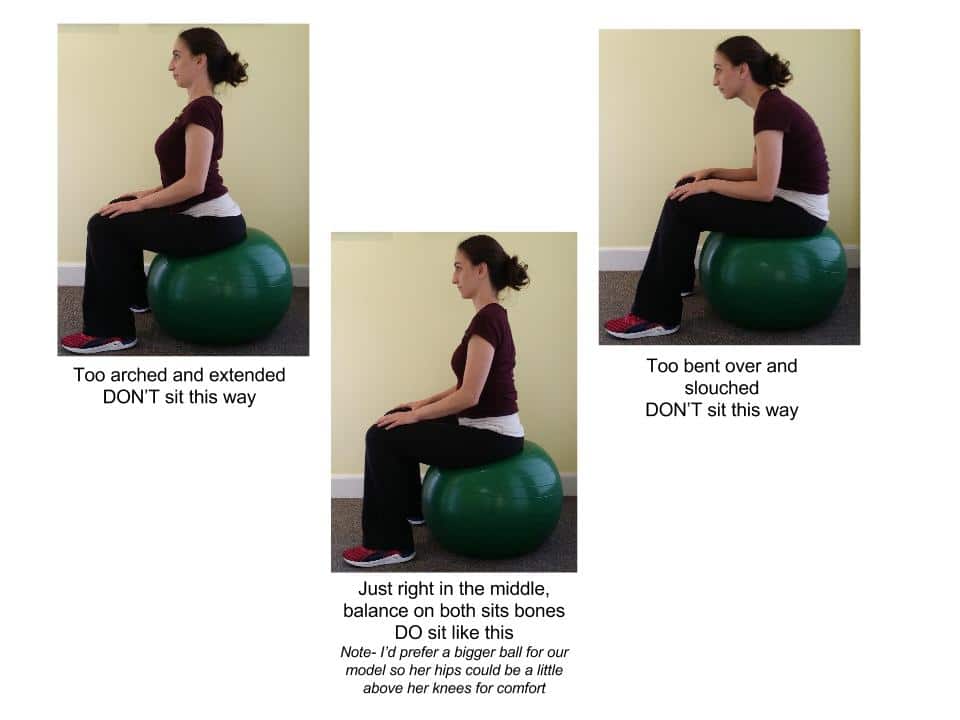
Start sitting in a neutral position, equally weighted on your sits bones right to left and back to front. It can be very helpful to do this on a yoga ball.
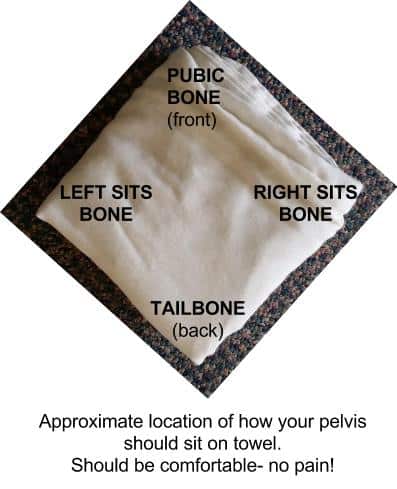
Or, if you don’t have a yoga ball you could sit upright on a firm chair on a folded hand towel. If using a hand towel, it is helpful to orient it with each corner matching the pubic bone, tailbone and two sits bones,so the square towel is rotated to make a diamond. This just gives better feedback to the muscles since they attach from the pubic bone, coccyx and sits bone.
Take a couple moments to relax and breathe easy, relax your breath and diaphragm, let your belly drop. Once you feel comfortable you can try some of these cues to activate your superficial muscles of your pelvic floor.
Exercise 1: Wink
There is a small thin sphincter around your anus. It has quick movement.
Very lightly try to wink your anus. Then relax. Wink your anus. Relax.
Try this a couple times, then breathe and let go all the way.
Exercise 2: Nod
There are some muscles that attach right below your pubic bone, to the fascia around your urethra and clitoris/penis. Try to nod the clitoris/penis. Relax. Nod. Relax. Nod. Relax.
You can also try the cue lift or flick the clitoris/penis (just don’t actually flick it with your finger ;).
Try this a couple times and relax and breathe.
Exercise 3: Draw
Now we are going to think a bit more globally.
A. Try to draw your pubic bone to your tailbone, or draw front to back and back to front, lightly. Relax. This should not engage your belly, hips or thighs, it should be very light.
B. Now try to draw sit bone to sit bone to meet in the middle, lightly. Relax. This should not engage your belly, hips or thighs, it should be very light.
C. Now try both at once, draw the Four Corners* together to meet in the middle, front and back draw towards the center, right and left draw to the center, lightly. Relax. Same as above, keep it light.
*remember Four Corners exercise for later
Note: There is a tendency to overdo this one, so keep it easy. It should feel like a hint of a movement. As with all the above exercises, your glutes, belly, jaw, shoulders are relaxed.
After you do all these exercises, go into a child’s pose or happy baby posture to help your pelvic floor let go and stretch. After you exercise a muscle it is helpful to stretch it to keep it mobile.
Happy Baby
Child’s Pose
Week 2: Diving into the Deep End
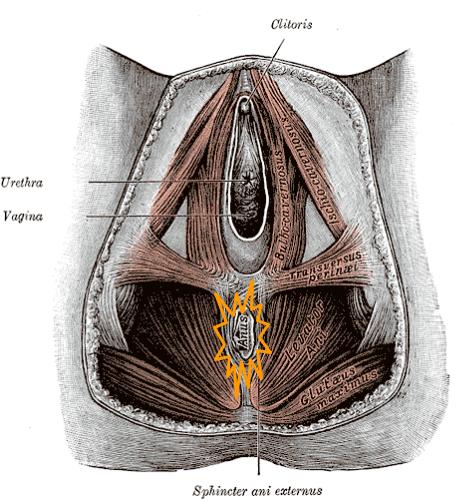
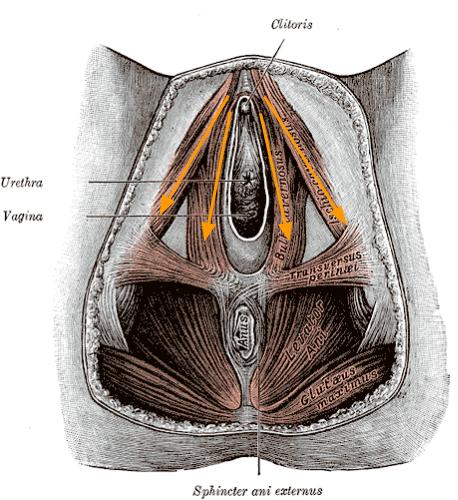
So after a week or so of Synchronized Sphincter work, if you have no increased symptoms and no pain, you can now dive into the deep end. In Week 1 the focus is on layer 1 of the pelvic floor, which tends to be flat muscles, primarily in charge of closing, hence “sphincteric”. Now, in week 2, we’ll focus on the deeper pelvic floor muscles. These muscles are in charge of supporting the pelvic organs and are considered part of our “core”.
If you’re a visual learner take a look at the pictures below. If they just confuse you, skip it.
From Below
From the Side
Okay, now that you are thoroughly confused let’s just get down to business: how to facilitate the deep pelvic floor muscles.
Pick up the Hankie
In this exercise we transition from superficial to deep muscles. So start sitting on a yoga ball, or on a firm surface with a folded hand towel, like before.
1. Inhale feel the relaxation and drop of pelvic floor muscles into the surface (ball, towel).
2. Exhale, draw the Four Corners to the center.
3. Inhale, relax, feel the drop/bulge of the pelvic floor.
4. Exhale, draw the Four Corners to the center, imagining you are drawing the corners of a hankie together…. then, once the four corners are gathered, slowly lift the hankie deep into the pelvis.
(If you are sitting on the towel you can imagine you are drawing the corners of the towel together then lifting it up in the center)
5. Inhale, relax, everything.
6. You can repeat this ~ 5 times. If you’re doing this correctly you should feel your low abdomen tighten on it’s own and you should be able to breathe normally.
Variations:
A. Maintain the contraction for 2 easy breaths, then relax. Make sure you keep breathing the whole time- don’t hold your breath, that’s cheating 😉
B. Instead of “picking up the hankie” straight up, try picking it up on a diagonal. If you look at the orientation of the pelvic floor muscles they are actually like a sling, coming off the pubic bone, wrapping around the anus and back up to the pubic bone. This may be helpful in actually feeling the work. So, draw the anus towards the pubic bone.
C. If you feel like you just keep squeezing your butt you probably are. You can tell when you relax your muscles, your butt or hips relax too, meaning these extra muscles were working as well. If this is happening, then try laying down on your back and bring your legs up to your chest and hold them there with your arms, kinda like happy baby. This position inhibits you hips from working and relaxes your pelvic floor. That way you can sense when you are using your pelvic floor muscles versus your butt.
Move and Grove
Once you tap into your pelvic floor muscles you can try adding this contraction to everyday activities or exercise routines. What you should find is you have more stability and power, it will take you less effort lift, swim, walk, hike, ski, etc. Below are just a couple ideas to connect the pelvic floor with bigger movements.
1. Arm pulls/flutter arms
Using light resistance, stand comfortably with slightly soft knees (you can do this seated or on your back knees bent in neutral spine). Inhale to prepare, exhale draw your pelvic floor muscles deep and slightly up towards the pubic bone (same contraction as we’ve been doing). Now to feel the connection you can pull your arms straight down in front of you, or in a slight “V”. Inhale, keep the arms down, Exhale slowly bring the arms up and rest. Repeat as you’d like.
2. Hover Planks
On your hands and knees position, keep your spine in neutral. Inhale, exhale and draw your pelvic floor muscles in, and your navel to spine. Then hover your knees just above the ground. Take 5-10 breaths maintaining the alignment, slowly lower, and relax. Repeat as you’d like.
3. The sky’s the limit, just see if you can incorporate in your favorite exercises.
I hope you enjoyed this cursory introduction to your pelvic floor muscles. Hopefully this shed a bit more light on that black box. Remember, the strength of a kegel is not measured by the squeeze, but how it supports the rest of our movement and function.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.