Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Joshua Gonzalez, MD
The advent of oral birth control pills in the 1960s was heralded as a huge victory for women’s rights. Finally, women could take control of their bodies and their fertility. Since then, oral contraceptive pills (OCPs) have become ubiquitous in reproductive aged women with nearly 10 million women today using The Pill as their primary means of contraception (Guttmacher).
Unfortunately, most of those women have no idea how these medications work and often have not been told of their potential side effects. Worse yet, many women are given oral birth control pills for non-contraceptive reasons: erratic mood, recurrent migraines, irregular menses, menstrual cramping, endometriosis, and even acne. Starting in adolescence, OCPs are handed out to women like candy. Women can spend many years in their young adult lives on these medications simply because they haven’t been properly counseled on alternative forms of contraception.
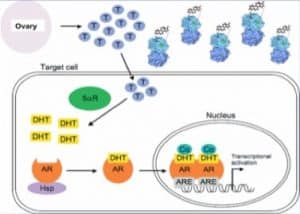
So what’s the big deal? Why should you be worried if you’re on an OCP? Well, let’s talk about how these medications work. OCPs are drugs mostly comprised of synthetic hormones. That is, fake hormones. These medications trick your ovary into thinking there’s enough real hormone around by exposing it to a hormone-like compound. Consequently, ovarian production of very important sex steroid hormones stops, as does ovulation. Hence, no pregnancy!
The problem is that your body needs sex steroid hormones for lots of different things. Estrogen, progesterone, and testosterone are all important for the health of a woman’s body. Yes, I said testosterone (more on that later). These hormones are important for bone health, cardiovascular health, libido, mood, cognition, and especially the health of the genital tissues. And when the body isn’t exposed to these hormones, like when you’re on an OCP, there can be consequences.
One recent study found that women using a hormonal contraceptive method experienced less frequent sexual activity, arousal, pleasure, and orgasm and more difficulty with lubrication (Smith). It is not uncommon for young women on OCPs to report pain with intercourse (called dyspareunia) as well. Some women may not experience dyspareunia but can present with other symptoms like urinary urgency, urinary frequency, recurrent urinary tract infections (UTI) or yeast infections. All of these things can happen with OCP use, but often go unrecognized or ignored.
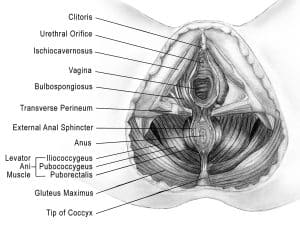
To understand why this happens, one must appreciate the anatomy of the genital tissues and how they respond differently to specific hormones. These details are not known by most patients on OCPs and often are lost on the physicians who prescribe these medications.
The female genitalia are comprised of three unique anatomic structures: the vulva, the vagina, and the vestibule. Each of these tissues arise from different embryological structures during fetal development. And each of these tissues respond uniquely to specific sex steroid hormones.
The vulva and vagina primarily rely on estrogen to maintain their health. When a woman goes through menopause and her ovary stops producing estrogen, these tissues can become dry, inflamed, chronically irritated, and literally shrink (atrophy). Similar things can happen to younger women on an OCP. When these tissues are chronically irritated they become a breeding ground for bacteria and yeast and can lead to recurrent infections. The lack of estrogen can also cause less vaginal lubrication, which can lead to pain with sexual activity.
The vestibule is a thin rim of tissue at the opening of the vagina. If you’ve never heard of it, you’re not alone. It is often ignored and easily missed during routine pelvic exams. Your gynecologist probably went right by it when she inserted that speculum. But it can cause even more problems than the vulva and vagina combined. The vestibule is an area responsible for mucus secretion, which provides lubrication during sexual activity. It is an area also intimately related to the urethra, the opening to the bladder that you urinate from. And unlike the vulva and vagina it is an area rich in testosterone receptors. When vestibular tissue is unhealthy, like when there are low levels of circulating testosterone caused by OCP use, it too becomes chronically inflamed or irritated. This can lead to pain with penetration and/or urinary symptoms that can be incorrectly assumed to be a UTI or yeast infection.
But the real damage of OCPs is their effect on a naturally occurring protein in your body called sex hormone binding globulin (SHBG). SHBG is a protein in the blood that binds testosterone and renders it inactive. Only a small amount of the testosterone your ovary makes then is actually used by the body. The rest is bound to SHBG. When women take OCPs, their SHBG skyrockets! Many physicians who prescribe these medications do not appreciate this point. With higher SHBG levels, more testosterone is bound and not usable by the body. OCPs already decrease ovarian testosterone production and now most of what’s left of your testosterone is being gobbled up by all the SHBG floating around. Worse yet, SHBG levels often remain elevated even after OCP discontinuation.
Many women I’ve treated have been misdiagnosed for years, told they have recurrent UTI or yeast infections or interstitial cystitis. Their physicians failed to appreciate that their symptoms were primarily a hormonal deficiency and that their OCP use was to blame. If you’re on The Pill now or were at one time you could be at risk. If you recognize or have experienced any of the symptoms I’ve mentioned, it’s worth discussing this with your health care provider. If they don’t believe you or have never heard of these potential adverse effects from OCPs, then maybe it’s time to find a new provider.
Case Example:
One particular patient stands out in my mind. When we first met, CL was 24 years old and had already been struggling with the effects of her birth control for more than two years. She first noticed pain in her vulva and vestibule (termed vulvodynia and vestibulodynia, respectively) during and after sexual intercourse. The pain was mild at first, but then intensified and lasted for longer periods as time went on. Soon she could barely sit more than a few minutes before a similar raw, burning pain would suddenly flare. She started avoiding sex and noticed a significant decrease in her libido. She began experiencing urinary frequency and urgency too. She was told by numerous physicians that she had recurrent urinary tract and yeast infections, prescribed countless rounds of antibiotics and fluconazole. She was even diagnosed and treated for interstitial cystitis. Despite being dismissed by many, she knew all the while the problem had not been addressed. This problem wasn’t in her head and it certainly wasn’t an infectious issue. Her problem was The Pill. When I first explained the real cause of her symptoms, CL cried both tears of sadness and relief.
Women have stayed quiet about these issues for far too long because they think painful sex or recurrent infections are “normal.” They’re not. I have no doubt that The Pill did a great deal for women’s reproductive rights, but at what cost? With alternative methods of contraception—non-hormonal, often more reliable methods—why are we still so quick to prescribe these jagged little pills. They may be easy for women to take, but the consequences may be ultimately too hard to swallow.
Continue on to Part Two: Treatment solutions and alternative birth control options here.
Additional reading:
In 2015 an International Consensus Conference on Vulvar Pain was held to examine levels of evidence surrounding causes of vulvar pain and associated factors. During this meeting, it was decided that hormonal insufficiencies can cause vulvar pain. The details and resource list have been published in three locations, the references are listed below.
http://www.nva.org/wp-content/uploads/2015/01/2015_ISSVD_ISSWSH_and_IPPS_Consensus_Terminology.2.pdf
http://www.sophiebergeron.ca/images/publications/Pukall_2016_Vulvodynia.pdf
American College of Obstetrics and Gynecology: http://www.sophiebergeron.ca/images/publications/Bornstein_2015_ISSVD.pdf
References.
- https://www.guttmacher.org/united-states/contraception
- Smith NK, Jozkowski KN, Sanders SA. Hormonal contraception and female pain, orgasm and sexual pleasure. J Sex Med. 2014 Feb;11(2):462-70.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Elizabeth Akincilar, MPT, Cofounder, PHRC Merrimack
In May 2015 a Delaware jury ordered Boston Scientific, a medical device company, to pay a woman $100 million for pain complications following vaginal mesh placement for treatment of pelvic organ prolapse. A few months prior to that a Texas woman was awarded $73 million for similar complications. Some think that these cases are just the tip of the iceberg because many more similar cases are pending. Many companies like Johnson & Johnson have pulled some of their mesh products from the market altogether, whereas others continue to offer them.
The Offender: Mesh
Utilization of graft, traditionally a piece of living tissue that is transplanted surgically, has been used in pelvic floor reconstruction for over a century. In the beginning, grafts used in surgery to treat incontinence and prolapse were associated with a fair amount of complications. Things started to change when general surgeons began using synthetic grafts, or mesh, for hernia repairs and began getting much better outcomes. It wasn’t long before pelvic surgeons recognized the opportunity to improve their surgical outcomes and began using similar mesh products for pelvic floor conditions.
Fast forward to 1998 when the tension-free vaginal tape (TVT) mid-urethral synthetic (MUS) sling was introduced. This was a serious game changer for pelvic surgeons. Not only did it become the current gold standard for treatment of stress urinary incontinence (SUI), but it paved the way for the US FDA approval of transvaginal mesh prolapse repair. In 2010 approximately 210,000 synthetic slings were placed in the USA.2 Success rates were estimated at 51-99% for retropubic (behind the pubic bone) and transobturator (TOT) slings4-6.
Because of the success of the MUS slings, medical device marketing teams recognized a HUGE opportunity. It has been estimated that the prevalence of pelvic organ prolapse in women over 60 was 41.1%!1 Surgery for prolapse is performed twice as commonly as for continence surgery. That’s like 30 million potential patients!!! As you can imagine, transvaginal mesh ‘kits’ started coming out of the woodwork. CHA-CHING!!!!! In 2010 approximately 75,000 women underwent transvaginal mesh placement for POP.2
The Complaints
Unfortunately, using mesh in surgeries for both incontinence and pelvic organ prolapse had some serious repercussions.
One study reviewed the complication rates for mid-urethral synthetic (MUS) slings for urinary incontinence between 1995 and 2007, and reported 4.3 – 75.1% for retropubic slings, and 10.5 -31.3% for transobturator (TOT) MUS. The retropubic approach had a higher occurrence for bladder injury versus the TOT approach which reported more groin pain. However, pelvic pain and pain with intercourse has been reported in up to 24% following MUS slings. Another major concern after MUS surgery is urinary function. Some women report severe difficulty or inability to urinate or urinary frequency after MUS surgery. Overall, voiding dysfunction rates are estimated to be between 2.8 and 38% following a retropubic sling and 0-15.6% with the TOT approach7.
Early on, the results of transvaginal mesh looked promising for the treatment of pelvic organ prolapse (POP) in a few short-term studies. They were introduced to reduce recurrence as well as improve durability. Many companies began to market ‘mesh kits’ to simplify their placement transvaginally. However, serious complications started to emerge. Now it’s thought that the studies were not rigorous enough and many of the complications surfaced after the duration of the trial protocols.
The complications included mesh extrusion, also called erosion or exposure, as well as infection and pain. Mesh extrusion is when the mesh is exposed within the vaginal canal. The Society of Obstetrics and Gynecology of Canada reported a mesh erosion rate of 5-19%. Another study from the Society of Gynecologic Surgeons reported an erosion rate of synthetic mesh to be 10.3%. The symptoms of mesh erosion include vaginal discharge, vaginal pain, pain with intercourse, or pain experienced by the sexual partner. Pain with intercourse, or dyspareunia, has been reported at rates of up to 38% following transvaginal mesh placement8. Mesh actually causing infectious complications is relatively rare.
The Contributing Factors
It is unclear exactly what the contributing factors are of these devastating complications. Some ideas include poor surgical technique, deficient training, infection, patient factors, or an inherent defect of the synthetic material. In addition, there are still lots of unanswered questions regarding vaginal tissue, the aging process and how the mesh affects the vaginal wall healing and inflammatory responses. Other potential risk factors include concomitant hysterectomy, advanced patient age, smoking and diabetes mellitus.
What actually leads to the pain after mesh placement is likely multifactorial. It is thought to be a combination of nerve or muscle damage/entrapment and/or tension on the vagina or surrounding structures as a result of retraction (shortening) of the mesh, scarring, or chronic inflammatory response to the mesh.
The FDA’s response
Some of these complications were found to be irreversible and debilitating which lead to two FDA notifications in 2008 and 2011. In 2008 the FDA released a Public Health Notification in response to the complications related to surgical mesh. In 2011 the FDA Safety Communication stated that the complications ‘are NOT rare’ and the ‘transvaginally placed mesh in POP repairs does NOT conclusively improve clinical outcomes over traditional non-mesh repairs’. Their aim was to educate the public and healthcare providers about mesh and provide recommendations for informed decision-making. In fact, the FDA published a list of questions patients were encouraged to ask their surgeons prior to undergoing vaginal mesh placement as well as recommendations following surgery. Here’s a few examples of the pre and post mesh placement questions recommended by the FDA. You can find the complete list of the recommended questions.
Recommended preoperative questions:
- Why do you think I am a good candidate for surgical mesh?
- What are the pros and cons of mesh in my particular case?
- How likely is it that my repair could be successfully performed without surgical mesh?
- If surgical mesh is to be used, how often have you implanted this particular product? What results have your other patients had with this product?
- What can I expect to feel after surgery and for how long?
- If I develop a complication, will you treat it or will I be referred to a specialist experienced with surgical mesh complications?
Recommendations for postoperative care:
- Notify healthcare provider if you have any of the following:
- Persistent vaginal bleeding or discharge
- Pelvic or groin pain
- Pain with sex
- Post-operative pelvic floor physical and occupational therapy
- Many women with pelvic organ prolapse can benefit from pelvic floor physical and occupational therapy to improve their musculoskeletal function, decrease certain pains, and help restore normal bladder, bowel, and sexual function. Often times, pre and post-operative physical and occupational therapy is not offer to patients and it should be. Click for more information.
Treatment Options
For complications with a MUS sling in some women, either complete or partial removal of the sling is the only effective treatment. Removing the sling can be challenging for the surgeon and the extent of tissue damage is often unknown. Other possible treatment strategies include pelvic floor physical and occupational therapy, pain medications, and nerve blocks.
In women experiencing vaginal mesh exposure, treatment options include observation, use of topical estrogen or antiseptics, systemic or topical antibiotics, office-based trimming of the extruded material, and partial mesh excision or total mesh excision. Medical management alone with antibiotics, antiseptics and topical estrogen yield low success rates. Office-based mesh excision can be challenging due to limited visualization and discomfort for the patient. A more formal mesh excision, often a total excision, is preferred.
One study looked at 481 patients who underwent vaginal mesh revision. After mesh excision/revision surgery, 73% reported an improvement in pain, 19% experienced no change in pain, and 8% reported an increase in pain. Patients with prior chronic pelvic pain were significantly less likely to experience improvement in pain symptoms.3
Mesh excision has possible complications of its own. If the mesh was placed closer to the front of the vagina, excising it can injure the bladder or urethra. If the mesh was placed towards the back of the vagina, removing it could cause damage to the bowel.
The Mesh Hunter
Gynecologist and pelvic surgeon, Mark Conway, MD, commonly surgically excises vaginal mesh for women experiencing pelvic pain. During a brief interview, he gave us his two cents on mesh. Full disclosure, he has served as a plaintiff’s expert witness on mesh liability cases.
How do you determine who is a good candidate for surgical mesh removal?
Essentially, any patient with mesh that has pain is a potential candidate for surgical excision. However, an examination is essential. Upon vaginal exam, if palpation of the mesh causes pain, especially if it reproduces the pain the patient is complaining of, that is a good indicator that removing it would likely decrease or eliminate the pain.
How many surgical mesh removals have you performed?
200-300
What are the greatest challenges in surgically removing mesh?
It is easier to remove a completely intact mesh versus one that has been previously surgically revised. The transobturator mesh is more difficult to remove because the material is much more difficult to get to. Also concerning the TOT mesh, it can be very difficult to locate in the groin. Another challenge is removing mesh that goes through the sacrospinous ligament, as is used in some repairs for pelvic organ prolapse. Lastly, mesh can get fibrotic and adherent, essentially stuck, to the bladder, urethra and bowel, which can be challenging to remove.
What are the greatest risks involved in mesh excision?
Bleeding can be a risk because the area is so vascular. Also wound infection and damage to the urethra, bladder and/or bowel are also risks.
How often have your patients already undergone a surgical mesh removal before consulting you?
80% of the patients that come to see me have already undergone at least one surgical mesh revision, and often they are on their 3rd or 4th procedure. In fact, patients are often told that their mesh had already been removed or can’t be removed any further, yet I am almost always able to find and remove additional mesh.
Do you utilize mesh in SUI and/or POP treatment?
I do not utilize transvaginal mesh for POP. I only perform a laparoscopic approach. I don’t place midurethral slings, but I will refer patients to a urologist to have it done.
Although surgeons and clinicians are recommended to report mesh and device complications, adverse events are underreported and the reporting process can be time consuming and is completely voluntary. Until a national registry exists, recognition of device-associated complications will be further delayed and not reported in the literature, thus exposing even more patients to these risks. Until then, I encourage women to do their homework before considering a mesh placement procedure. Find a surgeon who has performed many of these procedures and utilize the FDA’s recommended list of questions before you commit to surgery.
- Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–1166
- US Food and DRug Administration (2011) FDA safety communication: update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse 13 May 2013.
- Danford JM et al. Postoperative pain outcomes after transvaginal mesh revision. Int Urogynecol J (2015) 26:65-69.
- Serati M, Ghezzi F, Cattoni E, et al. Tension-free vaginal tape for the treatment of urodynamic stress incontinence: efficacy and adverse effects at 10-year follow up. Eur Urol 2012;61(5):939-46 17.
- Ward K, Hilton P; Group UaITT. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 2004;190:324-31 •• First randomized controlled trial between TVT and Burch colposuspension. .
- Ogah J, Cody J, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev 2009;4:CD006375 19. B
- Kasturi S, Hale DS. “J” cut of sling for postoperative voiding dysfunction following synthetic midurethral slings. Int Urogynecol J 2011;22(8):933-6
- Bako A, Dhar R. Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct 2009;20(1):103-11
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
What is GYROTONIC®?
When I first heard a colleague talk about gyrotonic about 4 years ago, I was like “GYRO WHAT? To me it sounded like some form of geriatric exercise, so I asked her more about this type of exercise and she gave me the low down. ‘Gyro’ in greek actually means spiral or circle, and tonic means tone or invigorate. I then decided to sign up for some classes to check it out. I walked into a studio in Boston and to my surprise, I stumbled upon a small room with about 7 of these large pieces of equipment. All of the gyrotonic towers were intriguing to me, as they are handcrafted, and each one looks like a unique, wooden masterpiece. Growing up, I was a competitive swimmer and ended my career in college. I was always looking for an exercise similar to swimming where I would not have to jump in a freezing cold pool and expose myself to chlorine. When I started my first session with gyrotonic, I knew I had to become a certified instructor. Not only was I so happy to have found a fluid and rhythmical movement that reminded me of swimming, but I also really enjoyed having a one-on-one session where my super knowledgeable instructor had all eyes on me. If I did something wrong or engaged a muscle incorrectly, she was able to modify the exercise for me. I was coming back from a right hip injury, and gyrotonic was the best way I could have eased back into safe exercising because of the personalized treatment.
**Photo taken at GYROTONIC® Boston Central
EVERYONE is familiar with pilates and its popularity in the exercise world, however not many people are familiar with gyrotonic. As a gyrotonic instructor, I am often asked the question “What is gyrotonic?” and “How does it differ from pilates?” Gyrotonic is a unique movement method that incorporates simultaneous lengthening and strengthening of muscles. It helps to stimulate circulation and improve joint mobility and coordination. Gyrotonic exercise includes spiraling, circular movements, and more rhythmical movements, making it feel more like dancing, swimming, yoga, and Tai Chi. Most conventional strengthening regimens are more linear or isolated movements that do not include functional everyday movements. As humans, we do not move in a single plane, so it is important to do strengthening and exercise in more of a circular plane in order for it to carry over to activities of daily living. The whole idea of gyrotonic is to strengthen/stabilize muscles while lengthening the muscles and allowing the joint to move through a natural range of motion without compressing the joint.
Finally, special attention is focused on spinal motions to increase mobility and stability of the spine and pelvis. We, myself included, are so used to sitting all day long, whether it be in the car or at work. With prolonged sitting, we lose the mobility in our spines. This rigidity in our spines can cause a forward head and rounded shoulder position, and in turn can displace the center of gravity, and cause the pelvis to work extra hard to maintain an upright position.
Specialized Equipment: The gyrotonic expansion system is a pulley tower that provides smooth, even support and resistance. There is also an adjustable bench and rotating handle unit that can be adjusted to fit individual body types. The gyrotonic tower supports the natural range of motion of joints and allows for functional three dimensional movement.
GYROTONIC® and persistent pain: It is often difficult finding a form of exercise that allows movement and release of endorphins, especially when you are experiencing pain. Gyrotonic is a specifically gentle form of exercise similar to yoga, however, the equipment allows you to take away some of the effects of gravity and allows you to experience less impact. The equipment also adapts to your body so that you can be as comfortable as possible doing the gentle motions.
Exercises: Here are some basic exercises that incorporate the gyrotonic principles without use of the gyrotonic expansion system. These are simple exercises to do while at your work desk and will help to improve sitting posture. Take note that these exercises should be done without any pain. If you experience any pain, please stop the exercise.
Step 1 – Finding your sit bones:
This simple exercise is REALLY important in order to find a “balanced” or more upright sitting posture. Sitting in a firm chair, make sure you have your feet supported by the floor about hip distance apart. Take your hands and place your palms face up underneath the bony part of your bottom. As you do this, see if you are shifting your weight to one side more than the other. You should feel equal pressure in both of your hands. If you are leaning to one side, shift your weight and find that nice balanced position.
Upright Seated Posture Poor Seated Posture
Step 2 – Seated Figure 8:
This is a great exercise for releasing tension in the pelvis/hips/low back. This aids as a gentle hip/back stretch by incorporating sitting posture and balance. It also helps to improve postural support and balance, which is SO important when sitting at a desk all day. Start by finding your sit bones and feel your feet grounded on the floor about hips distance apart. Maintaining a neutral spine, start by shifting your torso forward so that you have more weight on the front of your sit bones/thighs. Then, shift your weight over to your right sit bone and then back onto your right posterior sit bone or your right buttocks muscle. Next, allow your weight to come forward through the center and then repeat on the left side. You want to think of making a circle around each sit bone so that it makes a figure 8 shape. Here is a video to better help guide the exercise.
Step 3 – Spinal Motions on Chair: This exercise helps improve mobility in the spine.
Arch/Curl: Maintaining a seated position like the above exercises, lift your chest toward the ceiling and open your palms so that they face forward. Come back to neutral and then go into the curl. Curl: Tuck your chin and curl your upper back and lower. Try to maintain an elongated spine reaching through the top of your head. Try to prevent too much hunching or collapsing by vacuuming your lower belly towards your spine in order to prevent any compression in your spine. Repeat this arch and curl motion 5 times.
Seated Arch Seated Curl
Side Arch: Start in a neutral spine with arms by your side. Slowly, side bend your torso to the left, keeping your palms facing forward. Do not compress your left side, instead think of the left side bending but also elongating and maintaining space in the left hip. Come back to neutral and repeat on the right side. Perform this exercise 5 times on each side.
Right Side Arch Left Side Arch
Spiral (rotation): start in a neutral spine and rotate body to the left. An emphasis of the rotation should be placed through the rib cage. Come back to neutral and then switch sides, rotating to the right side. Repeat exercise 5 times on each side.
Right Spiral Left Spiral
Wave: Start in a neutral spine position and spread feet a little further than hip distance. Lift spine into arch position and then slowly bend forward at the hips. Once you get closer to your thighs, start to tuck your tailbone and curl your low back. Think of the curl starting from the lowest part of your back and then ending with a tuck of the chin. This should create a wave-like appearance and it feels wonderful!
Want to give it a try? Here is how to find a gyrotonic studio near you!
Find a gyrotonic studio near you!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.