Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
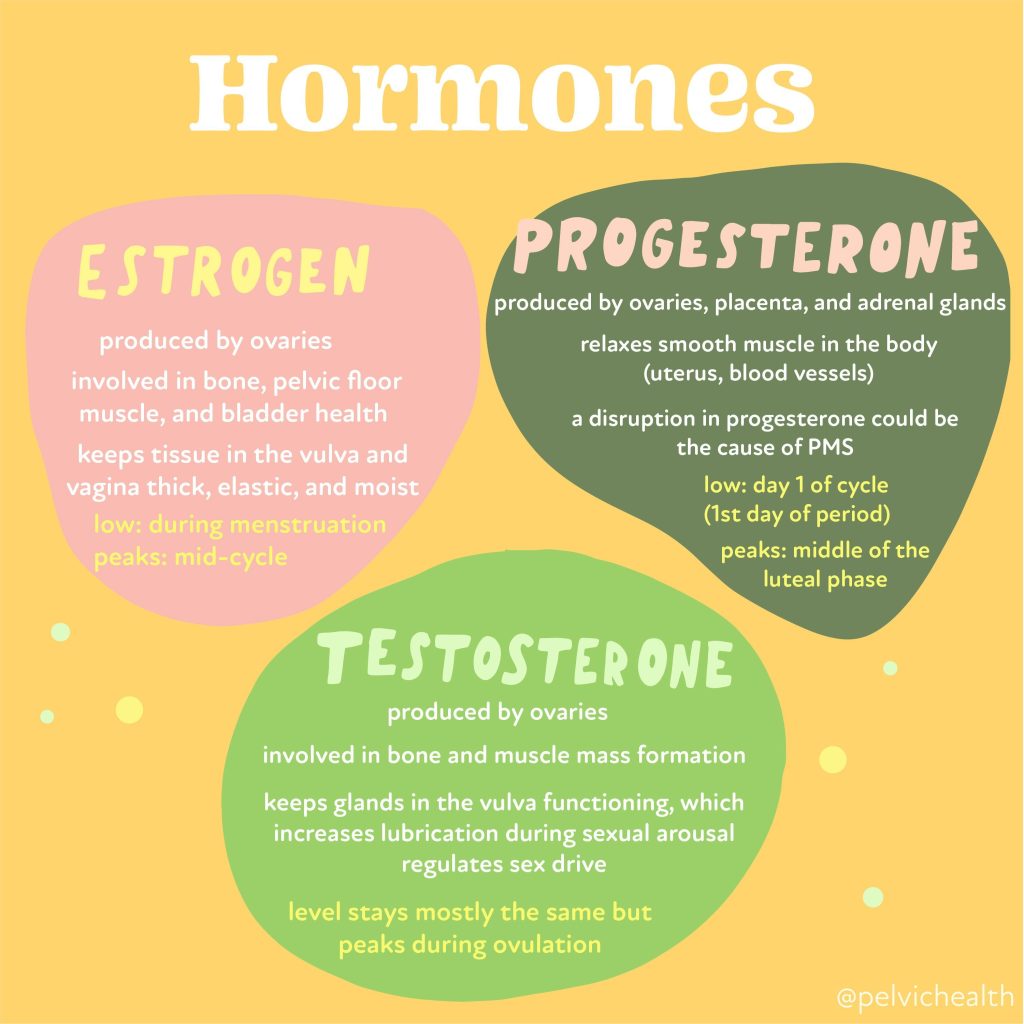
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Stephanie Prendergast, MPT, PHRC Pasadena
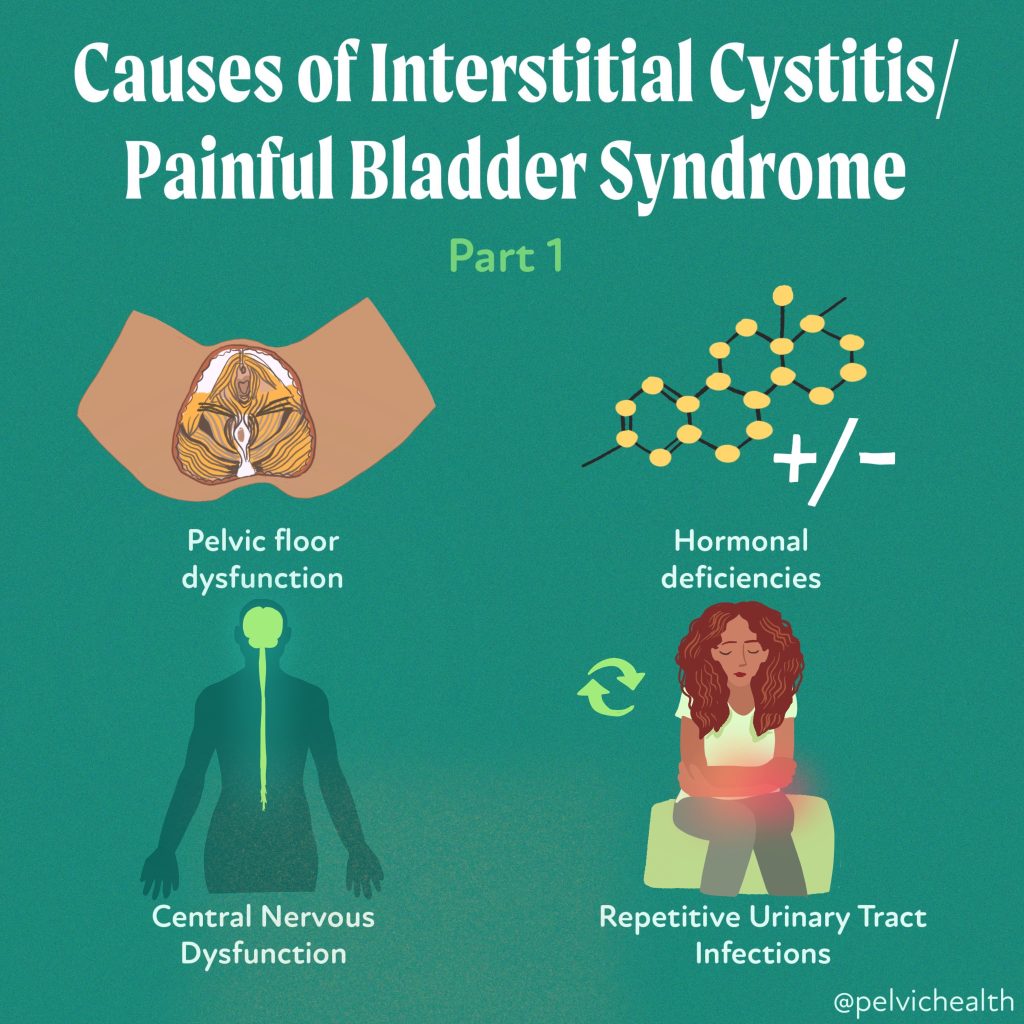
Here at PHRC we help people recover from irritative bladder symptoms with pelvic floor physical and occupational therapy. Bladder symptoms plague millions of people on a daily basis and anyone suffering can explain how much the symptoms compromise their quality of life. Multiple terms and diagnoses have been used to describe bladder symptoms which has led to inconsistencies and diagnosis and treatment challenges amongst clinicians, researchers, and patients. The diagnosis of “Interstitial Cystitis/Painful Bladder Syndrome” (IC/PBS) is a common pelvic pain diagnosis, yet the medical community continues to struggle with terminology and treatment guidelines. One main reason is that there are various phenotypes of the disorder and each subset comes with different treatment considerations. The American Urological Association’s (updated) 2022 IC/PBS Guidelines have deemed the diagnosis one of exclusion and recommend pelvic floor manual treatment as treatment given the majority of patients also have pelvic floor pain.
If a majority subset of patients with IC/PBS have pelvic floor dysfunction it begs the question is the bladder the victim or the cause of symptoms? If we can better define WHY someone has bladder symptoms we can better help them recover. In this post we are excited to share new research from our colleagues at UCLA helping to better define and treat these symptoms!
Lower Urinary Tract Symptoms and Myofascial Pelvic Floor Dysfunction
A recent study published in Scientific Reports introduces a novel condition termed Myofascial Urinary Frequency Syndrome (MUFS), which affects approximately one-third of individuals experiencing urinary frequency. MUFS is characterized by a persistent sensation of needing to urinate, regardless of actual urine volume—a symptom the researchers refer to as “persistency.” This sensation is accompanied by signs of myofascial pelvic floor dysfunction, including pelvic floor muscle hypertonicity and tenderness.
The Presence of “Persistency”
The study involved a comprehensive examination of patients presenting with urinary frequency. Findings revealed that 97% of MUFS patients exhibited pelvic floor hypertonicity with either global tenderness or myofascial trigger points, and 92% displayed evidence of impaired muscular relaxation. These symptoms are hallmarks of myofascial dysfunction. To confirm the association between these symptoms and pelvic floor musculature, the researchers assessed 68 patients with established pelvic floor myofascial dysfunction through comprehensive examination and electromyography. The presence of “persistency” was confirmed in these patients, and improvement was observed with pelvic floor myofascial release therapy.
Importantly, MUFS presents a distinct symptom complex that differentiates it from other lower urinary tract conditions such as Overactive Bladder (OAB) and Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS). This distinction is crucial for accurate diagnosis and effective treatment, as traditional therapies for OAB and IC/BPS may not address the underlying myofascial dysfunction present in MUFS patients.
The identification of MUFS underscores the importance of considering myofascial pelvic floor dysfunction in patients with urinary frequency. It also highlights the need for targeted therapeutic approaches, such as pelvic floor myofascial release, to alleviate symptoms and improve quality of life for those affected by this condition.
Why we are so excited about this…
The diagnoses IC/PBS and OAB describe symptoms without stating a cause. This emerging research confirms that for some patients the origin of the symptoms is the musculoskeletal system and pelvic floor therapy can help! Most people go right to the doctor when bladder symptoms arise, once infections are ruled out pelvic floor therapy should be the next stop!
But the good news does not stop there. The same group of researchers took things a step further by validating a questionnaire that can help clinicians and patients identify who can benefit from myofascial pelvic therapy.
Explaining the Persistency Index
A recent study published in the American Journal of Obstetrics and Gynecology introduces the Persistency Index, a novel screening tool designed to identify myofascial pelvic floor dysfunction (MPFD) in patients experiencing lower urinary tract symptoms (LUTS). MPFD is a condition characterized by hypertonicity and tenderness of the pelvic floor muscles, often leading to urinary frequency and urgency.
The Persistency Index focuses on the symptom of “persistency,” defined as a continuous sensation of needing to urinate regardless of actual urine volume. This symptom is a hallmark of MPFD and distinguishes it from other conditions like overactive bladder or interstitial cystitis.
In the study, researchers evaluated patients with LUTS using the Persistency Index and found a significant correlation between high scores and the presence of MPFD. This suggests that the Persistency Index can serve as an effective screening tool, enabling healthcare providers to identify MPFD more accurately and tailor treatment plans accordingly.
The development of the Persistency Index represents a significant advancement in the assessment of pelvic floor disorders. By facilitating early and accurate identification of MPFD, this tool has the potential to improve patient outcomes through targeted therapeutic interventions.
Why this is so helpful…
People treating patients with bladder symptoms know very well some people have pain with their symptoms and others are more plagued with urgency and frequency without pain. By improving symptom classification we can offer more accurate therapies. For example, if someone does not have irritation of the bladder lining itself but rather pelvic floor dysfunction, this person should benefit from pelvic floor therapy and would likely not respond to procedures such as bladder installations. If someone has bladder pain from multiple UTIs and the bladder lining is irritated they may be a good candidate for an installation over physical and occupational therapy.
Conclusion
These recent diagnostic and treatment advances are helping people get to the right place for help. We are grateful to the authors for their work and for supporting myofascial pelvic floor therapy as a treatment option for patients!
Resources
Interstitial Cystitis/Bladder Pain Syndrome: Diagnosis and Subtypes
Working on mind over bladder? Urine good company
How to find informed medical providers
International Pelvic Pain Society Find a Provider
American Physical and Occupational Therapy Association’s Section on Women’s Health PT Locator
Herman and Wallace Find a Provider
Pelvic Guru Provider Directory
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: pelvic floor muscle dysfunction, urinary tract symptoms associated, pelvic floor myofascial release
A Novel Approach using Blue Mind Science
By Tracey Chester, LMFT, CCTP
Founder and Director of the Pain Trauma Institute
In the summer and fall of 2023 an innovative study was born, “Project Stoke” (Surfing Therapy with the Ocean and Kinesthetic Engineering). Project Stoke is a collaboration between the Pain Trauma Institute (PTI) and USC’s Department of Biokinesiology and Physical and Occupational Therapy led by Dr. Jason Kutch. Our project was focused on exploring the therapeutic potential of surf therapy for chronic pain; and served as a foundation for future research utilizing virtual reality as a modality to help this population. Building on previous work identifying patterns of neural dysfunction in patients with Chronic Overlapping Pain Conditions (COPCs), this initiative investigated how the immersive ocean environment and dynamic nature of surfing provided relief from pain and trauma-related symptoms. Surf therapy combines the physical and psychological benefits of surfing with structured therapeutic interventions, offering a unique and holistic approach to care.
Beyond pain relief, surf therapy offers broader psychosocial benefits.
Blue Mind science, pioneered by Wallace J. Nichols, explores how aquatic environments positively affect the brain, reducing stress, enhancing focus, and fostering a sense of calm. These principles underpin the transformative impact surf therapy has on participants managing complex chronic conditions. Surf therapy combines physical exercise, psychological resilience, and social connection within the therapeutic context of nature, offering an innovative application of Blue Mind principles. Preliminary evidence suggests that it engages both neurological and physiological mechanisms that alleviate pain, reduce stress, and improve overall quality of life. Further research is warranted to explore the specific neural and biochemical pathways involved, including the potential role of water-induced states in modulating chronic pain and trauma.
The theoretical framework in this study is one of immersive therapy with a manageable level of threat The dynamic and immersive nature of surfing incorporates exposure to manageable physical challenges, promoting neuroplasticity and resilience. Alex and Jake both overcame fear-avoidance behaviors, regaining trust in their bodies through incremental successes on the board. This process aligns with Blue Mind principles, which suggest that water-based activities stimulate the release of feel-good neurotransmitters like dopamine and serotonin, enhancing mood and reducing the perception of pain.
The need to focus entirely on the oncoming wave forms a unique state of mindfulness, that is characterized by reduced anxiety and enhanced emotional clarity, achieved through the sensory experience of water, which includes its sound, movement, The experiences of our participants provide compelling evidence of the multidimensional benefits of surf therapy in managing chronic pain and trauma.
Using the Groundswell Community Project model,
Which was adapted for chronic pain in this study, integrates Positive Psychology, Somatic Therapy, Mindfulness, Play, and indigenous connections to nature. Sessions consisted of approximately 70% land-based activities and 30% water-based surfing, focusing on promoting present-moment awareness, emotional processing, and bodily attunement. This combination not only encourages physical activity but also creates a safe, supportive space for participants to explore their emotions and develop resilience.
The pilot study involved nine participants (three males, six females aged 30-62 years old). Dr. Jandra Mueller, Director of Education at the Pelvic Health and Rehabilitation Center, was involved with participant selection based on meeting criteria of COPCs. Resting stage EEG as well as clinical questionnaires and self-reported pain data were collected both prior to and after being in the water. The EEG data was collected using a 4 channel MUSE device collecting at 256 Hz. Dr. Kutch explains, “In this pilot project, we aimed to build a multidisciplinary team that can use neuroscience and engineering approaches to understand and develop these therapeutic effects. Our Aim for this addressed the question of whether 6 weeks of surfing therapy reduces pain and neural dysfunction in patients with COPCs.”
The study showed promising results. Pain scores decreased by an average of 50%, with significant improvements occurring during water-based sessions. The McGill Pain Questionnaire highlighted a 56.17% reduction in descriptive pain terms, reflecting a shift from intense descriptors like “exhausting” to milder terms such as “tired.” EEG data also revealed changes in neural markers associated with pain, further supporting surf therapy’s potential as a therapeutic modality.
For many participants,
Surf therapy became a turning point in rebuilding trust and confidence in their physical abilities. Initially hesitant and apprehensive about their limitations, participants found themselves gradually pushing past their fears. Christina, who struggles with multiple injuries, endometriosis and pelvic pain used the buoyancy of the ocean and the encouragement of her instructors to take small but meaningful risks. Over time, standing on the surfboard, even for brief moments, became a powerful statement of her resilience. For Jake, who suffers from chronic pelvic pain, the physical challenges of surfing helped him confront his fear of pain and re-injury. Each session provided a safe space to explore his body’s boundaries and rediscover its capacity to adapt and recover.
Surf therapy offered participants moments of respite from the constant pain and emotional weight of their conditions. Jake described how being in the water provided a brief but meaningful reprieve, allowing him to focus on the present and escape the grip of chronic discomfort. Similarly. Nina, who suffers from complex pelvic pain, experienced a transformative moment during her first session, where the playful, freeing environment of surf therapy brought her genuine joy for the first time in years. For all participants, these moments of relief were more than physical—they symbolized hope and a renewed connection to happiness.
Physically, surf therapy engages the body in ways that improve strength, coordination, and proprioception while alleviating inflammation. The cold ocean water activates the parasympathetic nervous system (PNS), contributing to reduced pain perception and a calming effect. Psychologically, immersion in water triggers a state of mindfulness and relaxation associated with the “Blue Mind state.”. Participants like Nina described this state as a rare reprieve from the constant weight of chronic pain and emotional grief.
This freedom extended beyond pain.
Nina found herself smiling and laughing with others, marveling at how the ocean’s embrace could momentarily lift her from the depths of grief and exhaustion. Mental resilience was a key outcome of surf therapy for all participants. Jake noted how the process of confronting his fears in the ocean helped him manage the “fear of pain” itself—a psychological hurdle that had often kept him from engaging in physical activities. Each session became an exercise in pushing through discomfort and proving to himself that he could recover afterward. Christina echoed this sentiment, as the supportive environment of surf therapy helped her focus less on potential failure and more on the empowerment and joy of the experience.
Additionally, the ocean’s vastness and rhythmic waves foster a sense of awe and connectedness to something greater than oneself—a perspective that can shift attention away from pain and foster a sense of purpose and grounding. Surf therapy also reframes recovery goals within the biopsychosocial model of chronic pain management. Rather than striving for complete elimination of pain, participants emphasized functional improvements, emotional growth, and reconnection with activities that bring joy.
Surf Therapy
represents a powerful, holistic approach to managing chronic pain and trauma, offering hope and empowerment to those navigating these challenges. It fosters physical strength, stress relief, and emotional release while building resilience and self-confidence. Participants also benefit from a sense of community and peer support, reducing feelings of isolation often associated with chronic illness. While more research is needed, the study underscores surf therapy’s potential as an innovative and effective approach for managing chronic pain. Its dynamic, nature-based framework offers a unique pathway for healing, combining physical movement, mindfulness, and emotional connection in a transformative experience. With further validation, surf therapy could become a powerful tool in chronic illness and trauma recovery.
—
More About the Author
Tracey Chester, LMFT, CCTP, Founder and Director of the Pain Trauma Institute
Tracey is the founder and clinical director of the Pain Trauma Institute. She is a certified clinical trauma professional, a licensed marriage and family therapist, surf therapist, and a certified grief counselor.
“For me, it is a personal mission to help patients struggling with chronic pain or illness to achieve a full and meaningful life, despite their health struggles, as I know firsthand what it is like to live with chronic pain and its devastating effects on all aspects of life. Pain does not happen in a vacuum; it happens in a human being with a personality, likes and dislikes, strengths and weaknesses, and ways of thinking”
More About the Pain Trauma Institute
At the San Diego Pain Trauma Institute we empower you to relieve pain of all kinds through evidence-based mental health services and collaboration with our community of medical and research advisors. Pain Trauma Institute is a mental health clinic ocean therapy, grief counseling, psychotherapy for depression, anxiety, and other mental health issues related to chronic pain, caregiving, day-to-day life stressors, and trauma of all kinds.
We are a team of mental health therapists and physicians here to facilitate healing as a whole person. Through holistic treatment we seek to relieve suffering by understanding the current stressors you’re managing as well as the root cause rather than treating symptoms alone. We offer grief and trauma-informed care, meaning we take into account the mental, emotional, social, and physical factors impacting your unique experience.
Chronic Overlapping Pain Conditions
Improved understanding of neuroscience drives advancements in new technologies and treatments. For more information on this topic, check out the iCarebetter: Endometriosis Unplugged Podcast, where Jandra Mueller and Stephanie Prendergast talk with Jason Kutch, PhD about his groundbreaking research and own experience with pelvic pain. You can listen on both Apple Podcasts or Spotify.
Check it out for more information and please share your questions, we are happy to help answer them!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags, surf therapy programs, physical and mental health, surf programs, surfing sessions, sleep quality, stress hormones, international surf therapy organization, surf therapy sessions, physical health, post traumatic stress disorder
By PHRC Admin Team
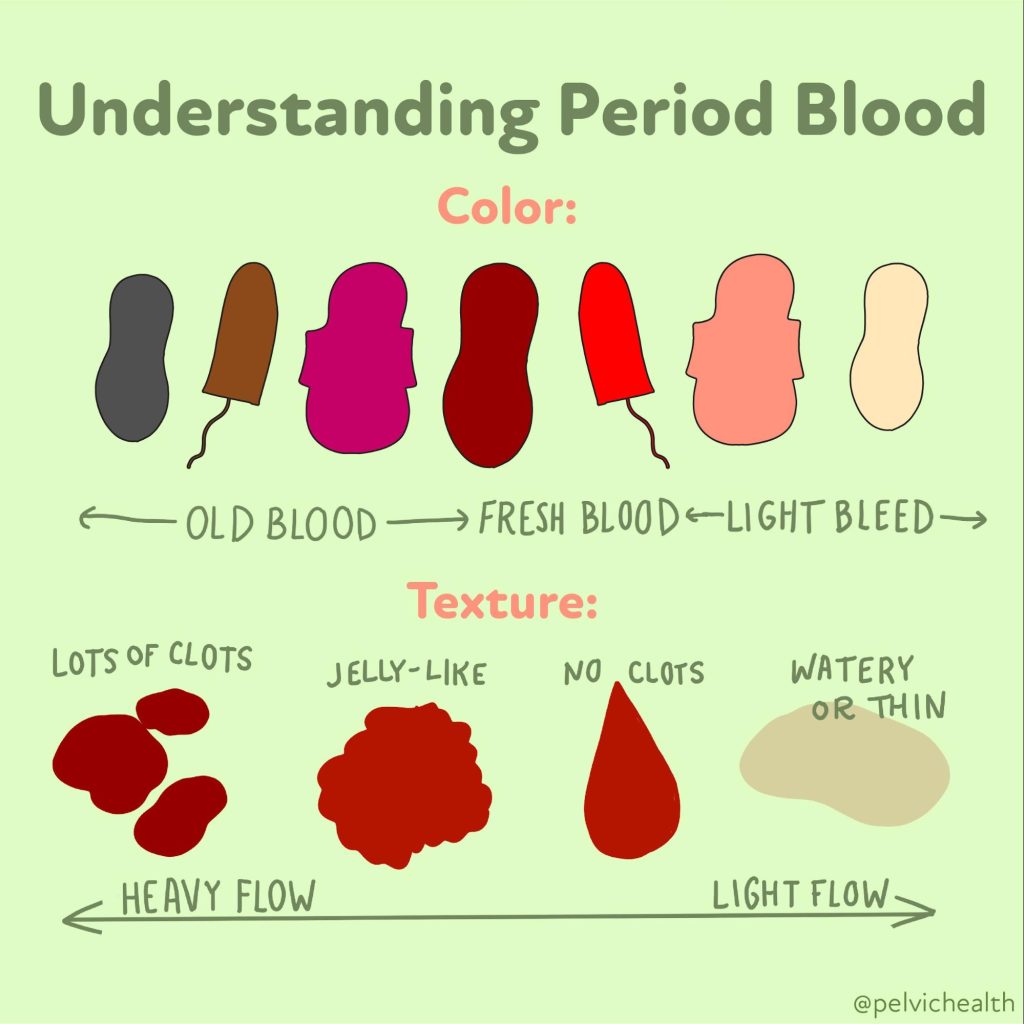
Menstruation. The word alone can bring a lot of emotions – confusion, embarrassment, relief, or sometimes just plain annoyance. Despite the fact that it’s a natural part of life for many people, there’s still so much we aren’t taught about our periods and menstrual cycles. Here are ten things I wish I was taught about my period.
1. Every Period is Unique
Just like us, no two periods are the same. Your flow, duration, symptoms, and cycle length can be different from your best friend’s or your sister’s – and that’s perfectly normal. While we want consistency with our cycles, even each cycle may be different. Our bodies are unique, and so are our periods.
2. Periods Aren’t Dirty
There’s a lot of stigma and taboo around menstruation, despite the fact that it is a natural, biological process and nothing to be ashamed of. It’s time we stop treating periods as something dirty that needs to be hidden away.
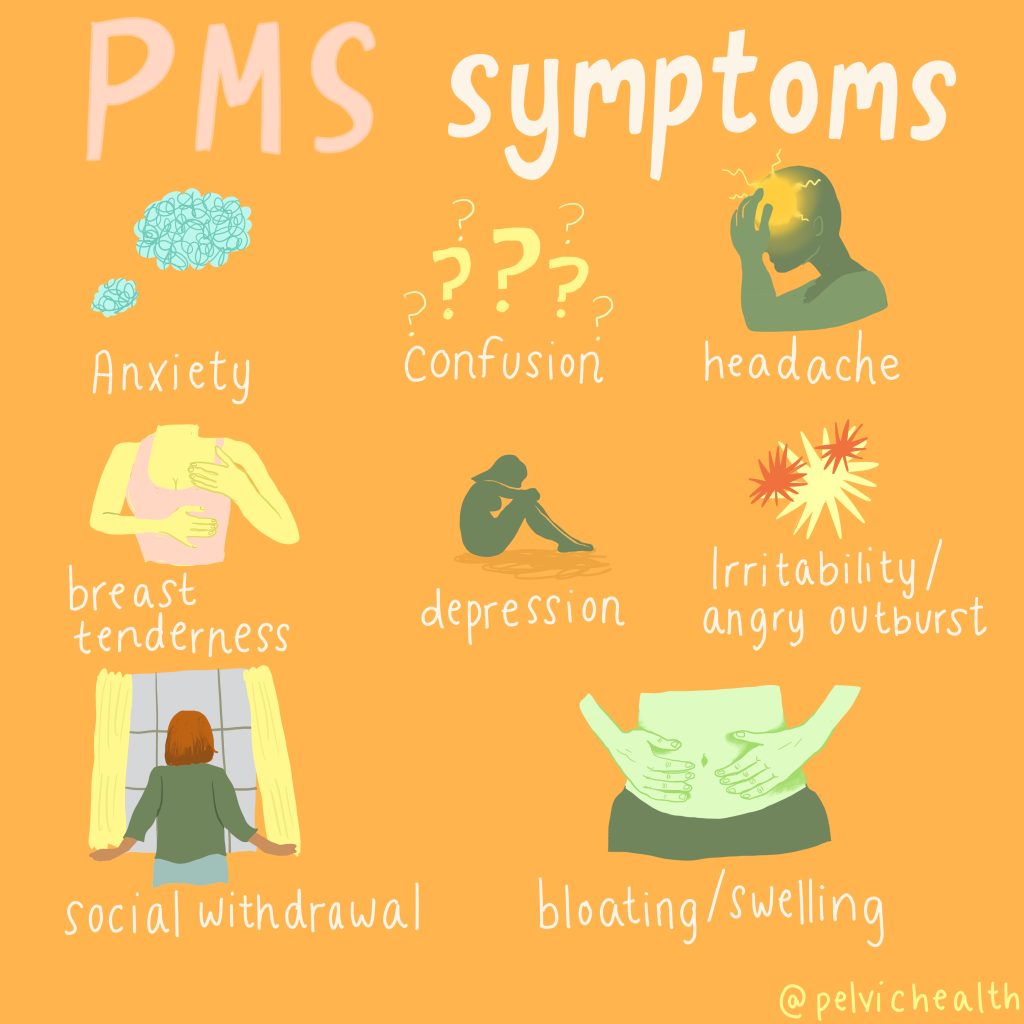
3. PMS is Real
Those mood swings, bloating, and cravings aren’t just in your head. Premenstrual Syndrome (PMS) is a legitimate medical condition that affects many people who menstruate and can vary from mild symptoms to severe, impacting one’s quality of life. If you suffer from severe, debilitating symptoms, there are providers that can help with this and please seek help.
4. Tracking Your Cycle Helps
Keeping track of your cycle can help you understand your body better, and give you more objective information to discuss with your provider if you have concerns. It can also help identify any irregularities early on. There are many apps available these days that make tracking your period a breeze.
5. Menstrual Products Vary
There’s more than just pads and tampons. Menstrual cups and period panties are eco-friendly alternatives worth exploring. These options can be more economical and environmentally friendly than traditional products.
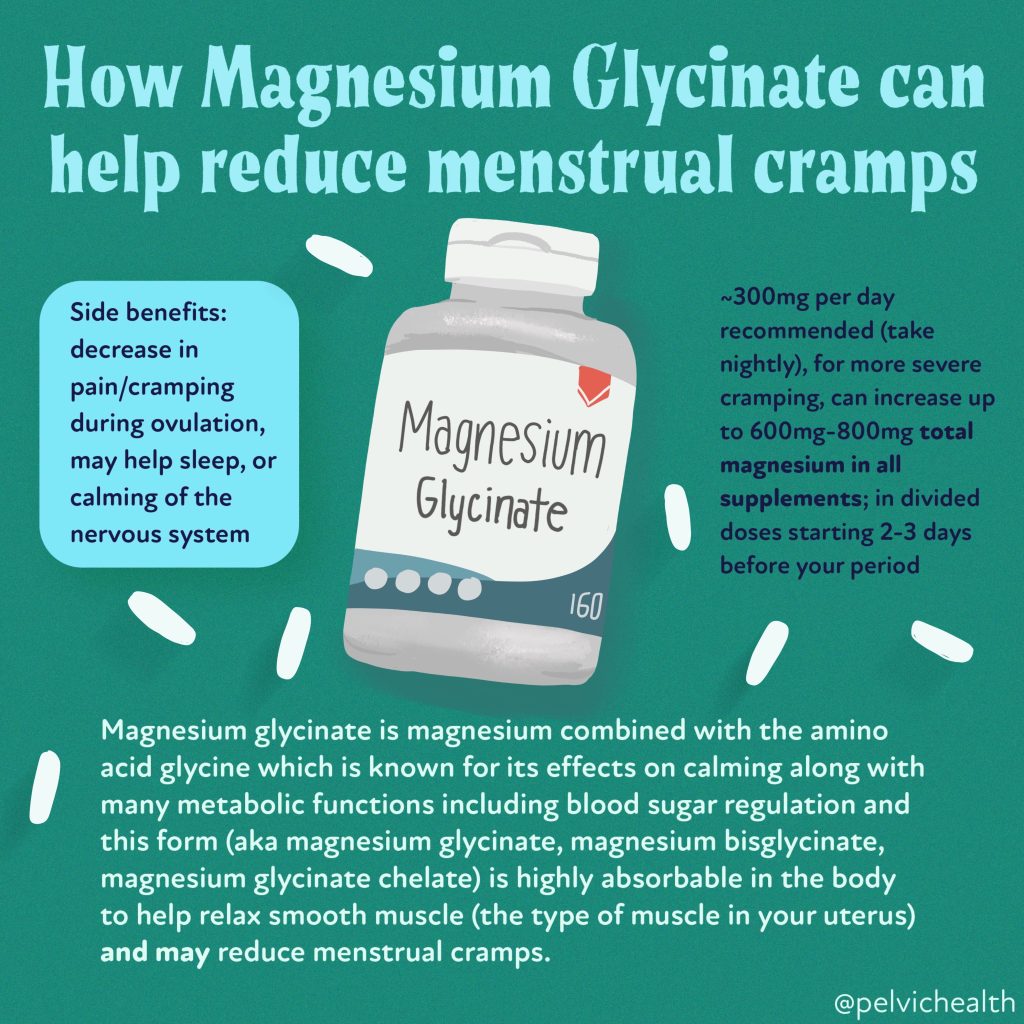
6. Exercise Can Help
While it may be the last thing you want to do when you’re on your period, light exercise can actually alleviate cramps and boost your mood. It releases endorphins, the body’s natural painkillers and mood elevators. Gentle yoga or massage, self-myofascial release techniques are also ways to help calm the nervous system and reduce menstrual pain, especially if you do these regularly.
7. Healthy Eating Matters
Certain foods can help manage period symptoms. Iron-rich foods can combat fatigue, calcium can help with PMS, and dark chocolate can soothe cravings! Remember, there are no ‘good’ foods or ‘bad’ foods when it comes to real foods. Though, food can be reactive in some people due to underlying issues such as small intestine bacterial overgrowth (SIBO), and these can increase bloating symptoms or other GI issues. Reducing, or eliminating sugar, is something that can help to improve symptoms, though many of us find ourselves with all the sugar cravings at this time. This could be a sign that we are deficient in certain nutrients, such as carbohydrates, and reaching for foods rich in nutrients (including carbs) may be helpful instead of that bag of peanut M&Ms. What is most important is finding out what helps you during this time!
8. Period Pain Isn’t Always Normal
Severe pain isn’t something you should just “put up with”. If your period pain is interfering with your daily life, it could be a sign of conditions like endometriosis, so don’t hesitate to seek medical advice. If your period is interfering with your ability to work, go to school, or enjoy social activities, this isn’t normal and there are treatment options.
9. Hormonal Birth Control Affects Your Period
Different types of hormonal birth control can lighten your period, make it disappear, or cause spotting. It’s important to discuss these potential changes with your healthcare provider before starting a new method, to better meet your contraception or symptom goals. While contraception is wanted by many for various reasons, there may be unwanted side effects. If you have concerns or notice any changes in your mood, urinary, or sexual functioning, discuss this with your care provider. There are so many options, it may take some time to find what is right for you.
10. Your Period Doesn’t Define Your Worth
Having a period (or not) doesn’t validate or invalidate your identity. You’re valuable and important, no matter what.
Let’s normalize talking about periods and empower each other with knowledge. The more we understand our bodies, the better equipped we are to take care of them. Need more resources? Check out our previous blog series about Period Health 101.
(Please note: Always consult a healthcare professional for medical advice related to periods and menstrual health.)
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: menstrual cycle, menstrual period, normal menstrual cycle, emotional and physical symptoms, luteal phase, menstrual blood, first period, body prepares, period products