Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
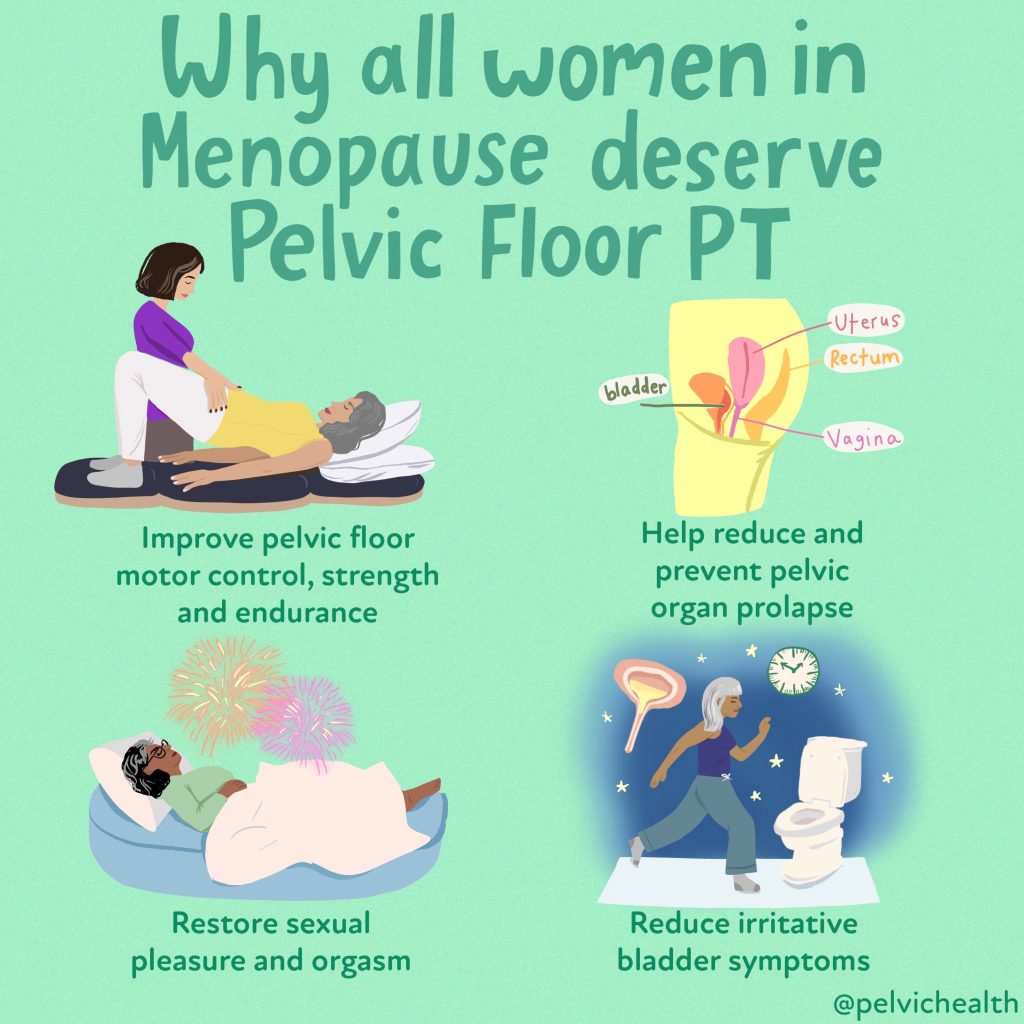
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
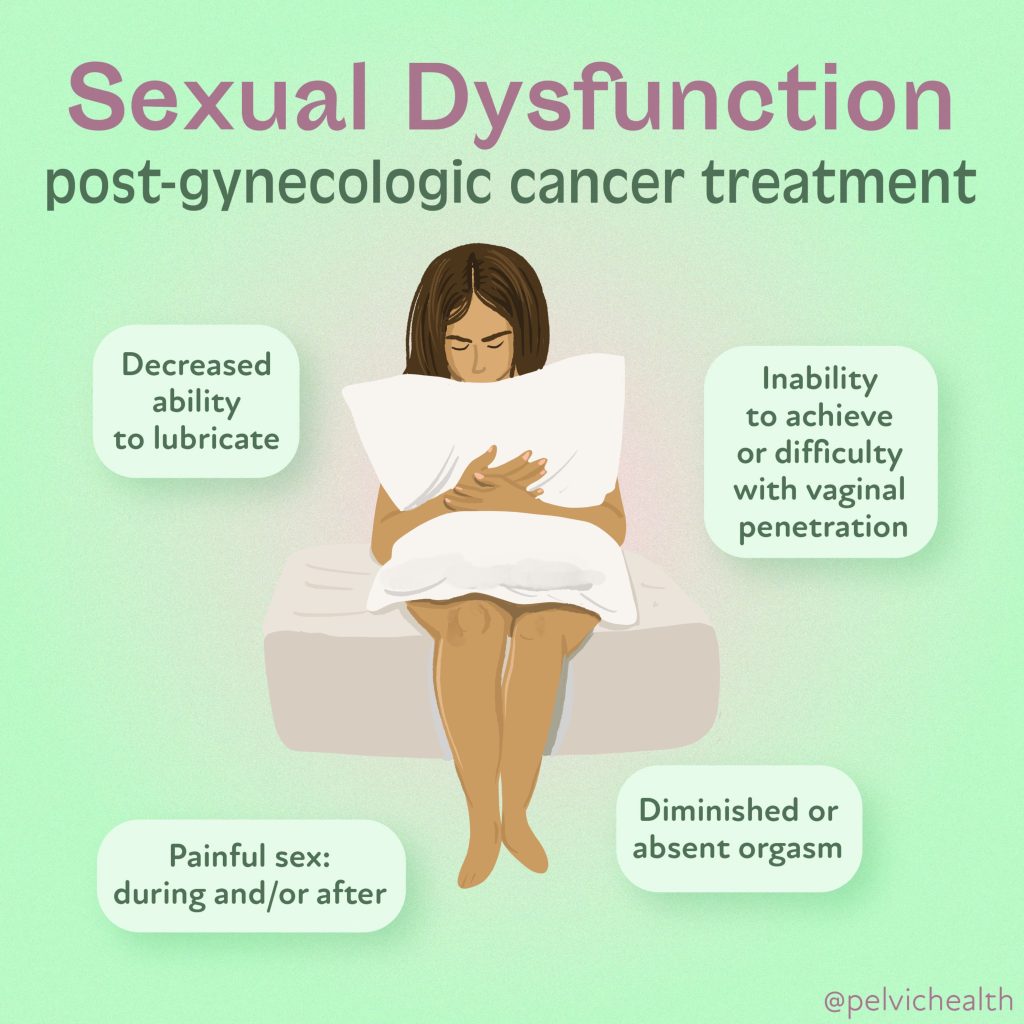
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

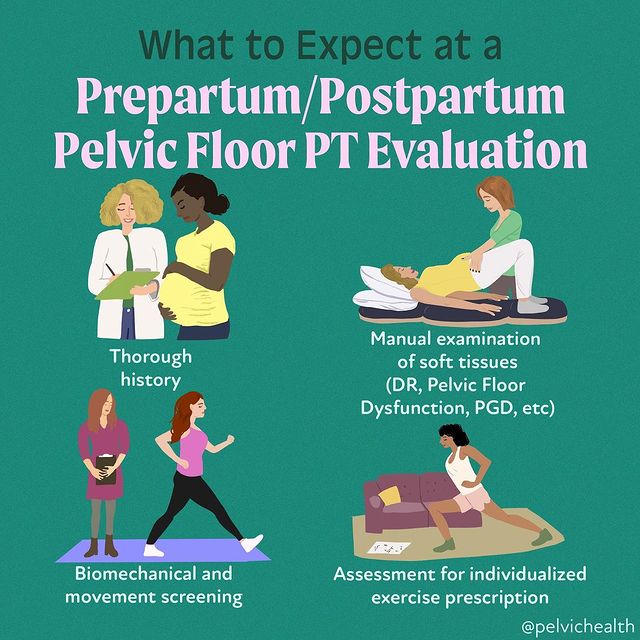
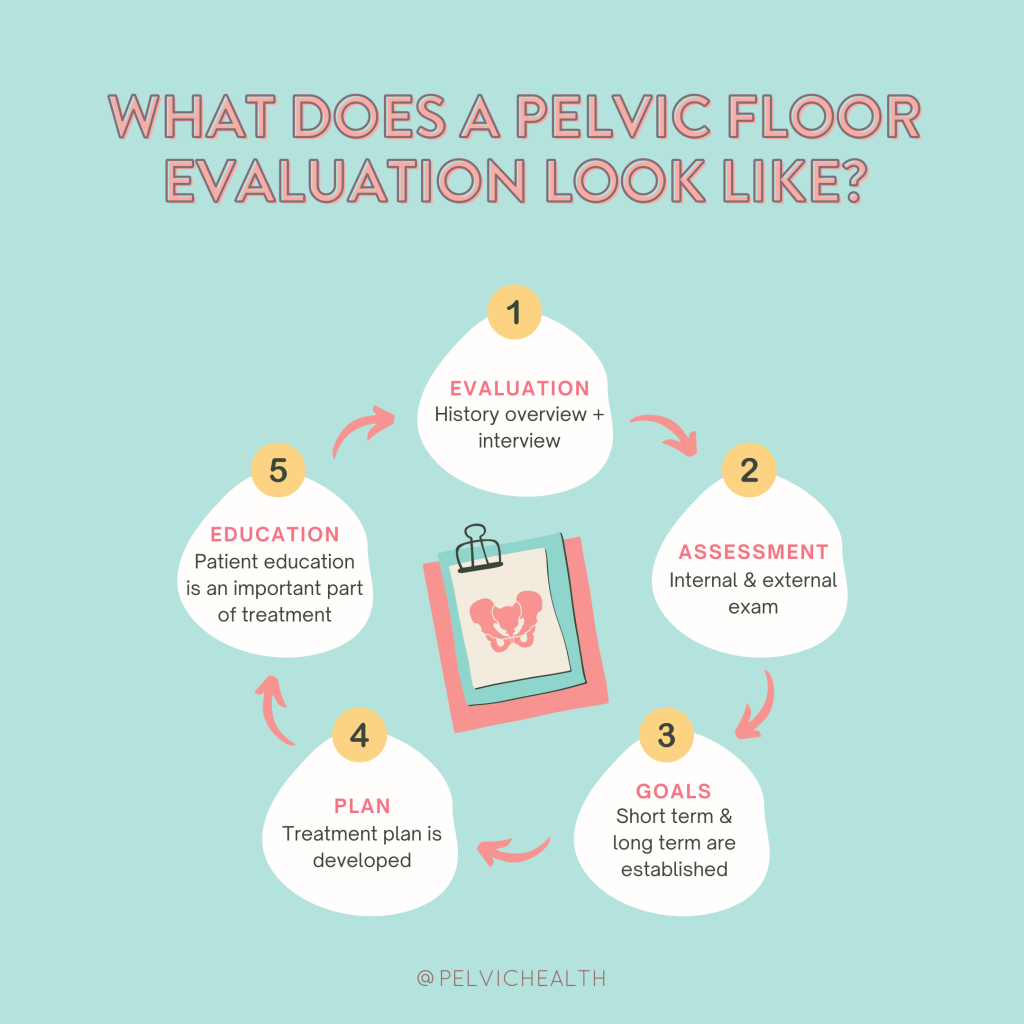
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Stephanie Prendergast, MPT, Cofounder, PHRC Pasadena and Cambria Oetken, DPT, PHRC Westlake Village
Spoiler alert: the answer is both. Let us explain.
Vaginal dilators are tools used to assist in the treatment of pelvic floor dysfunction, specifically when there are issues with penetration of any kind. Historically, patients have had to direct their own care and may have purchased dilators online or they were given dilators by a provider who gave little to no direction about how to effectively use them. Understandably, this has resulted in confusion, frustration, and ultimately, individuals not using them. Under the care of a pelvic health professional, and when introduced at the right time and circumstances, dilators can be helpful. However, when introduced at the wrong time, or under the wrong circumstances, they can be emotionally and physically problematic.
What Are Dilators?
Dilators are smooth, cylindrical devices that come in a range of sizes and materials, typically silicone or plastic. Most dilators can be used both rectally and vaginally, though there are specific brands that are meant specifically for these needs as well. Graduated dilators, meaning they start small and short and gradually increase in width and length, help to gradually stretch and desensitize the pelvic tissues, including the vaginal walls, vulva, and surrounding pelvic floor muscles. Dilators can be used as part of a pelvic floor therapy program to help with:
- Pelvic floor muscle tightness or ‘spasms’ (e.g., vaginismus, pelvic pain).
- Post-surgical healing, such as after a hysterectomy, pelvic cancer treatments, or vaginal reconstructive surgery.
- Scar tissue management after childbirth or injury.
- Improving pelvic muscle control and awareness.
- Sexual dysfunction, such as painful intercourse (dyspareunia).
Types of Dilators
They come in various shapes, sizes, and materials, but most follow a graduated set-up:
- Graduated Sizes: vaginal dilators typically come in a set with several sizes (small to large). The smallest size is generally used first, with the goal of gradually increasing to larger sizes over time as comfort and tolerance improve.
- Material: Most vaginal dilators are made of medical-grade, body-safe materials like (medical grade) silicone or soft plastic. They are designed to be smooth, non-porous, and easy to clean.
- Design: Some vaginal dilators are straight, while others may be slightly curved or come with a handle or flared base for easier removal.
Conditions That May Benefit from Dilators
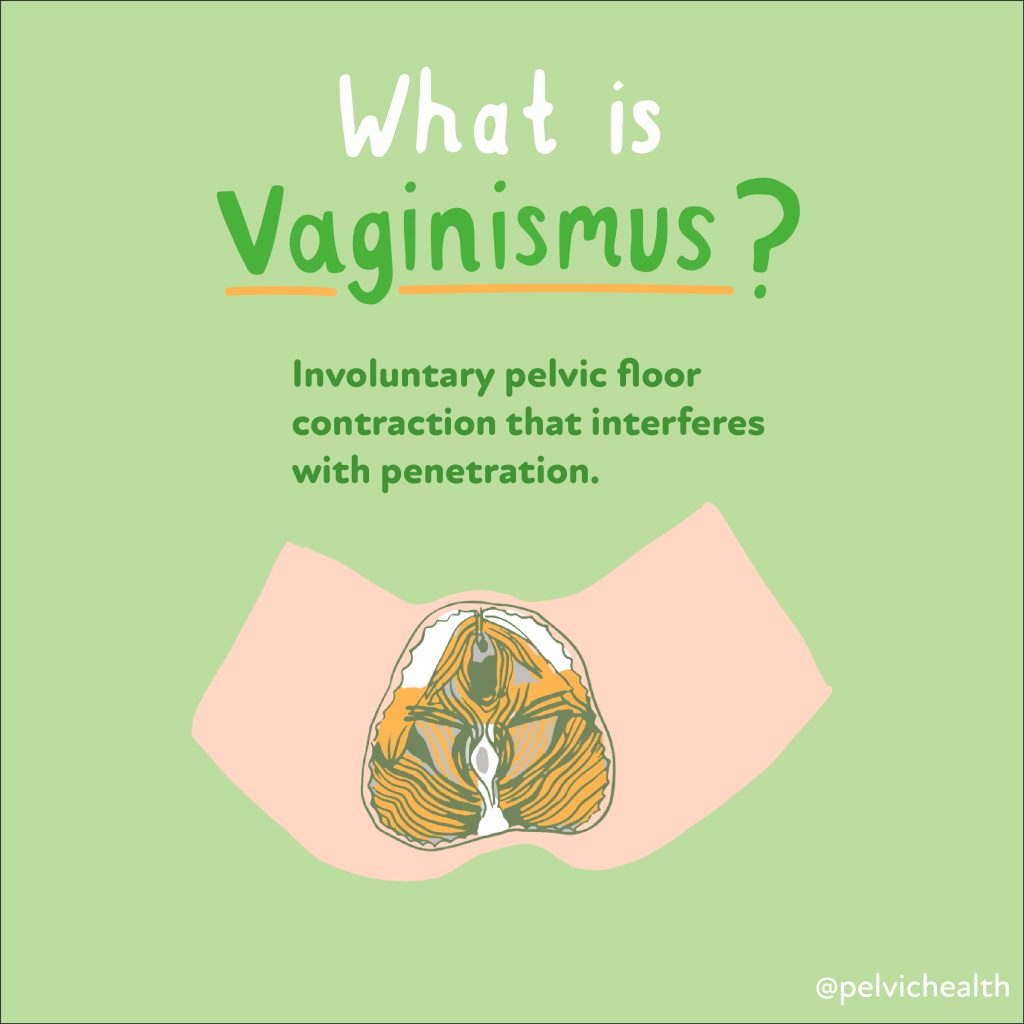
Vaginismus
A condition where the pelvic floor muscles involuntarily contract, making vaginal penetration painful or impossible.
Pelvic Pain
Chronic pelvic pain, which can be due to a number of reasons such as muscle tension or scarring, may benefit from gradual dilation to help release tension.
Postpartum and Peripartum Care
After childbirth or prepping for a vaginal delivery, pelvic floor muscles and the surrounding tissues may need rehabilitation to regain flexibility, especially after tearing or episiotomy.
Post-Surgery
After surgeries like a hysterectomy, pelvic reconstruction, vestibulectomy and gender affirming surgeries, vaginal dilators can help restore normal vaginal tone and elasticity.
Comprehensive Cancer Care
Gynecological and colorectal cancer survivorship is improving with the use of medical therapies including surgery, medications, and radiation therapies, but can impact the elasticity of the tissues and surrounding muscles. Dilators are often recommended in this population to improve function and tissue health.
Menopause
Vaginal atrophy and dryness due to reduced estrogen can cause discomfort, and a vaginal dilator may help maintain vaginal health and comfort. Sexual health is not the only important factor, routine gynecological care may also be more difficult when these structures are affected and a vaginal dilator can be helpful here as well.
How to Use (Vaginal) Dilators
PSA: every person’s dilator program should be individually tailored based on their findings (impairments), symptoms, and the overall goals for their plan of care. It is best to work with a pelvic floor physical or occupational therapist to determine an effective plan. Goals for dilator therapy can include:
- Trying to expand or maintain the diameter of the vaginal canal
- Desensitizing painful tissues
- Reducing pelvic floor myalgia (muscle pain)
- Reducing fear and anxiety around insertion and penetration
- Improving sexual confidence
- “Biofeedback” for pelvic floor motor control exercises
Depending on the patient’s goals, the type of vaginal dilators and instructions may vary. Earlier we cautioned that sometimes people may start dilators too early in their treatment plan; in general, dilator therapy should be postponed if:
- Someone has active vaginal infections.
- Someone is experiencing severe burning with insertion as this could indicate a non-muscular issue that should be evaluated by a specialist. Conditions such as neuroproliferative or hormonally mediated Vestibulodynia or genitourinary syndrome of menopause (GSM) or lactation (GSL) are common conditions where individuals start dilators per instruction of a care provider, or self-directed, and need a more thorough evaluation from a provider knowledgeable in sexual health to determine the best approach to care.
- Someone experiences increasing amounts of pain instead of decreasing discomfort as the session continues or lasting pain following dilation.
Dilator prescription should be a dynamic process between the user and the provider. Every few weeks we should be able to make physiologic changes and revise the treatment plan if necessary to address plateaus in progress in order to help people restore their pelvic health.
Important Tips for Success
Patience is key
Progress may feel slow, but with goal setting and working with a provider who can help address barriers, people see functional improvement over time
Pain is not normal
If you experience pain or burning (beyond mild discomfort), stop using the dilator and consult with your pelvic health therapist or healthcare provider to reassess your approach.
Gradual Progression
Do not rush to the larger dilators. The goal is to gradually stretch and relax the tissues, not force them.
Set the Environment
Try using calming music, meditation or white noise for optimal relaxation and avoid being on your phone or watching tv.
Use a mirror
A mirror can be helpful for you to connect more while using dilators and also help you become more familiar and comfortable with the anatomy. A mirror also allows you to track your progress and have a direct visual on the depth of your dilator being inserted.
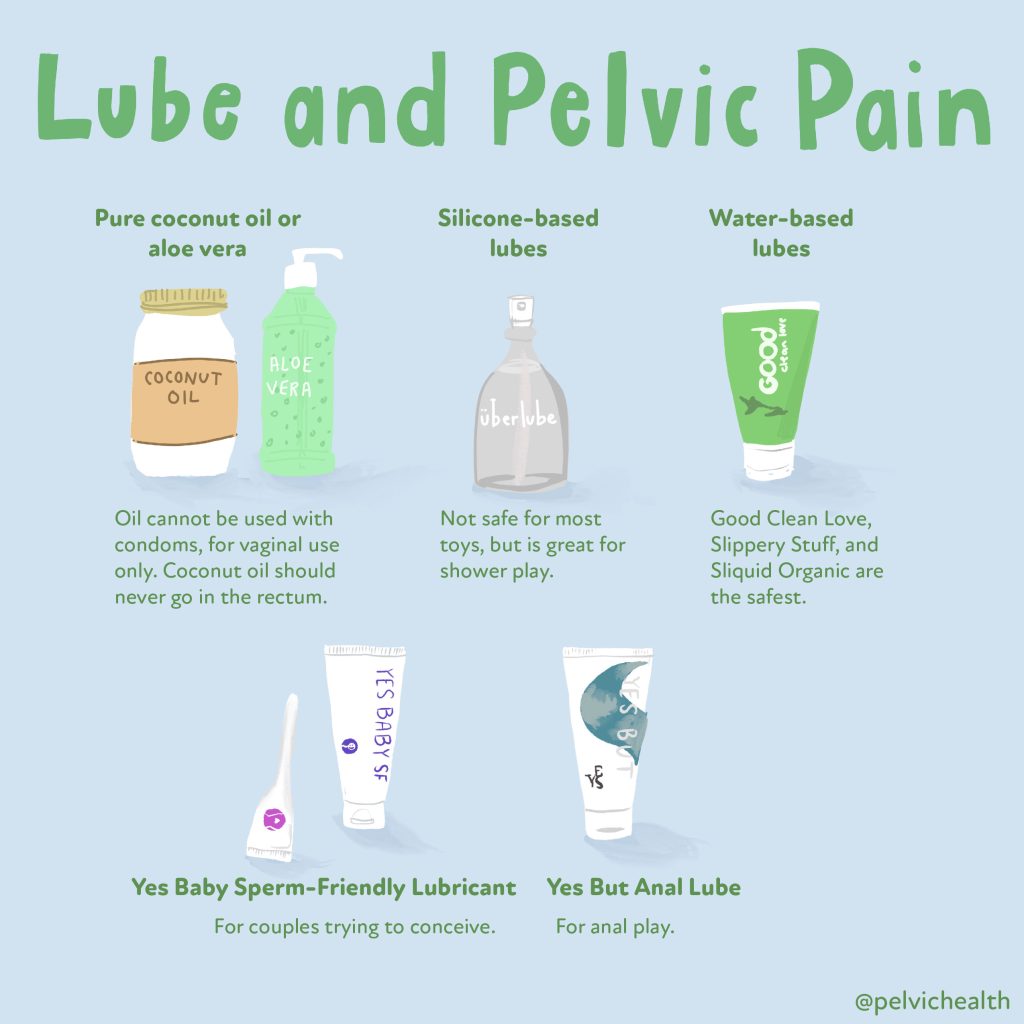
Lubricants
Use lube! But use the proper type of lubricant. Most dilators will require a good water based lubricant. Silicone or oil based lubricants should not be used as they can break down the materials over time. All lubricants are not created equal and should be compatible with the vulvovaginal environment. Check out our blog on lubricants for more information on ideal pH, osmolality, and brands we recommend.
Cleaning and Care
- Clean after each use: Wash the dilator with mild soap and water. Some dilators are also dishwasher-safe (check manufacturer instructions).
- Inspect for damage: Regularly check for signs of wear, cracks, or damage, and replace dilators as needed.
- Storage: Store dilators in a clean, dry place, away from direct sunlight and extreme heat.
When to Consult a Professional
If you experience persistent discomfort, pain, or difficulty using the dilators, it’s important to consult a pelvic floor physical and occupational therapists or return to your medical provider. A pelvic floor therapist can help assess the condition of your pelvic floor muscles, address underlying causes, and tailor a treatment plan to your needs. Vaginal dilator therapy depends on multiple factors, which is why consulting with a healthcare provider is essential. Dilators alone are rarely the answers to pelvic pain, if you are struggling please come find one of us to help you! Your pelvic health deserves it!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: vaginal dilator, physical and occupational therapy, dilator therapy, painful sex, pelvic exam, silicone dilator, medical condition, deep breaths,
Slimming Success or Health Setback? Weight Loss Drugs + The Pelvic Floor
By Cambria Oetken, DPT, PHRC Westlake Village
What is Ozempic?
You may be familiar with the name “Ozempic,” “Semaglutide” or even “GLP-1” likely due to their social media presence and celebrity influencers, so what really are these drugs and what do they do in our bodies? Semaglutide has gained increased attention in the most recent years for its role in managing type 2 diabetes and aiding in weight loss. This GLP-1 receptor agonist (GLP-1 RA) has been a game-changer for many patients struggling with type 2 diabetes however, it is now playing a role in weight loss. You may have heard other hot names that are also “GLP-1 receptor agonists” such as Trulicity, Wegovy, Mounjaro, Bzetta, Bydureon and Adlyxin to name a few. The question is, are these medications safe and effective? What are the side effects? If I have pelvic floor dysfunction, can this negatively or positively affect it??
So what in the world is GLP-1?
Glucagon-like peptide 1 (GLP-1) receptor agonists belong to a class of type-2 diabetes medications that mimic the function of the GLP-1 hormone secreted by the pancreas. Overtime, if there is poor glucose control in the body, this enzyme becomes less effective at regulating glucose, this is when a synthetic GLP-1 receptor agonist comes into play. GLP-1 RA can suppress appetite, delay gastric emptying, reduce plasma glucose levels and enhance insulin secretion in order to regulate glucose levels.
Ozempic, Wegovy, Zepbound etc….
Ozempic is an injection that was approved in 2017 to help lower blood sugar levels and reduce the risk of heart attack, stroke, or death in adults with type 2 diabetes and known heart disease. This drug is not approved by the U.S Food and Drug Administration for weight management however there are some that are. Wegovy (semaglutide) injection is a well known drug that IS approved by the U.S Food and Drug Administration (2021) for chronic weight management in adults with obesity or are overweight. Other examples of drugs that are FDA approved for weight management include, Zepbound and Saxenda. There are some differences between the types of drugs and dosages. For example, the dosage for Wegovy can be up to 2.4 mg performed once weekly as an injection whereas Ozempic contains lower doses of semaglutide at around 0.25 mg once weekly to start increasing to up to 2.0 mg. The significant difference is that Ozempic is approved to address insulin resistance for those with Type 2 Diabetes and not for weight loss, whereas Wegovy is approved as a weight loss treatment for those who qualify. The issue that has arisen is Ozempic is increasingly being prescribed off-label for weight loss without an FDA approval on its safety and efficacy. Additional concerns, as reported by the FDA, include compounding multiple GLP1 receptor agonists together leading to serious side effects. Due to this increase in off label use, patients should be aware and educated on treatment options, the impacts of off-label prescribing, and the side effects of these medications. Always speak to a provider regarding these options.
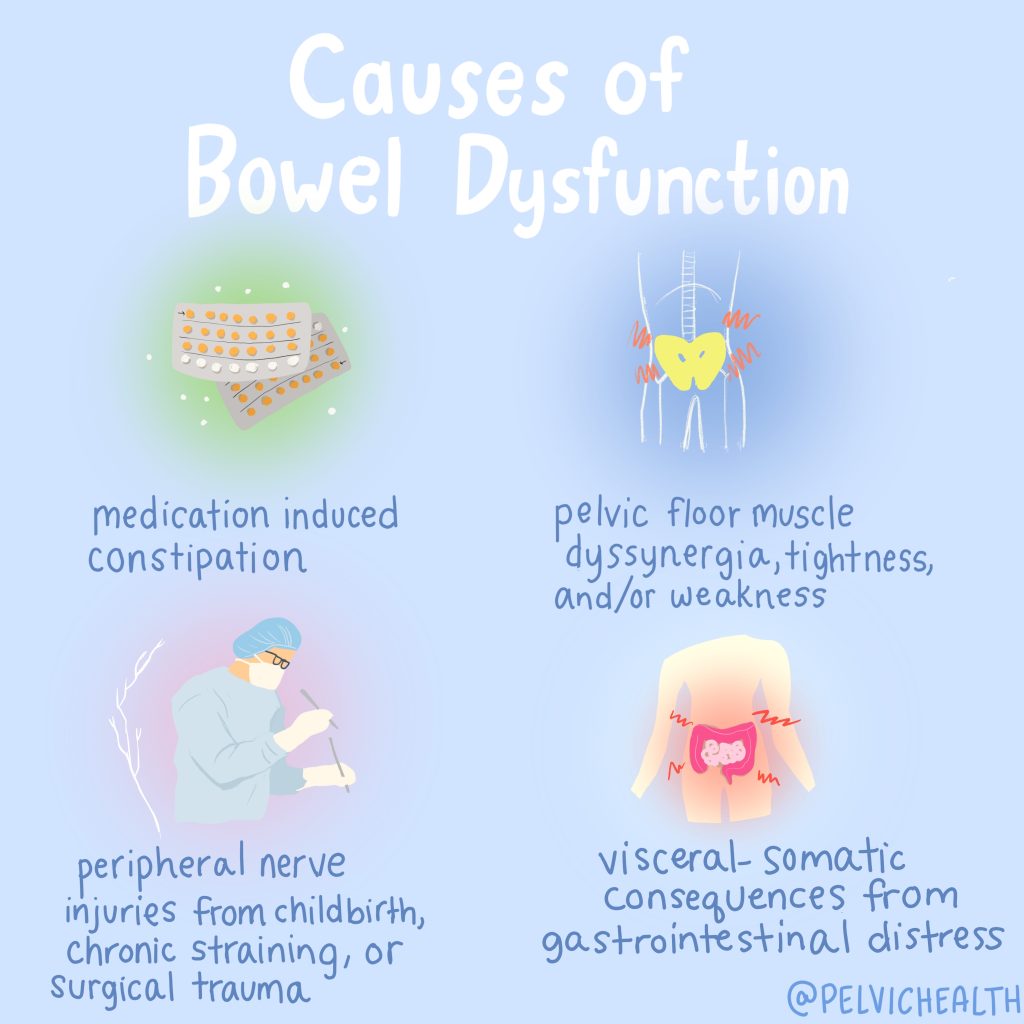
Common side effects and how they may impact your pelvic floor:
The most common side effects of GLP-1 RA include gastrointestinal effects such as nausea, vomiting, diarrhea, and constipation however usually do not cause the need for discontinuation of the drug. Other side effects include itchiness, redness, or other reactions at the injection site, headache, dizziness, mild tachycardia (increased heart rate), and infections. Some serious side effects include pancreatitis, gastroparesis, bowel obstruction, gallstone attacks, and bile duct blockage, however these side effects are rare and have been difficult to confirm a cause and effect relationship.
Constipation and diarrhea as well as bowel incontinence can be indicators of pelvic floor dysfunction and thus these types of drugs could exacerbate these existing symptoms. One of the common side effects of Ozempic is gastrointestinal issues, including constipation. This can occur due to its effect on slowing gastric emptying. When the stomach empties more slowly, food and waste move more gradually through the digestive tract, which can lead to reduced bowel movements and thus constipation.
Managing Constipation While on Ozempic
If you’re experiencing constipation while taking Ozempic, there are several strategies you can use to manage and maybe even alleviate this side effect:
1. Increase Fiber Intake
- Eat More Fruits and Vegetables: Incorporate high-fiber fruits and vegetables into your diet. (1 cup of raspberries has 8 grams of fiber!)
- Whole Grains: Opt for whole grain bread, cereals, and pasta.
2. Stay Hydrated
- Drink Plenty of Water: Adequate hydration helps support regular bowel movements. Opt for up to half your body weight in ounces of water a day.
3. Regular Physical Activity
- Exercise: Engage in regular physical activity to stimulate bowel function and improve digestion. Even walking for just 10 minutes a day can be beneficial!
4. Consider Over-the-Counter Remedies
- Fiber Supplements: Products like psyllium husk can help increase your fiber intake.
5. Proper Positioning
- Squatty Potty: Using a squatty potty or stool to elevate your feet can help relax the pelvic floor muscles to increase ease with bowel movements.
6. See a Pelvic Floor Physical and Occupational Therapists
- Muscle Coordination: A pelvic floor PT can help address motor control of the pelvic floor muscles to ensure you are properly utilizing your muscles effectively during bowel movements
- Manual Therapy: Manual therapy can be performed along the colon to assist is stool movement and reducing any discomfort
When to Seek Medical Advice
While mild constipation can often be managed with lifestyle and dietary changes, you should contact your healthcare provider if:
- Constipation Persists: If you experience severe or persistent constipation that doesn’t improve with home remedies.
- Severe Discomfort: If you have significant abdominal pain or discomfort.
- Changes in Bowel Habits: If you notice any unusual changes in your bowel habits or if you experience additional symptoms like nausea or vomiting.
There is a relevant study indicating an association between insulin levels and the activity of the pelvic floor muscles. In this study, the group with insulin resistance had lower activity of the pelvic floor muscles than those without insulin resistance. It is thought that skeletal muscles (such as those in the pelvic floor) can adapt to metabolic needs (such as insulin needs) in order to maintain energy balance and nutrient use, therefore decreasing activation of those muscles for energy conservation. There is also a known relationship between decreased muscle mass and short term use of glucose. Interestingly, for those struggling with Type 2 diabetes, insulin resistance and additional criteria could benefit from a GLP-1 receptor agonist and may have an added benefit of improved pelvic floor muscle activation.
An additional study looked at GLP-1 with the use of Metformin on the effect in men with Type 2 Diabetes and erectile dysfunction. Following 12 months of treatment, glucose management greatly improved than with Metformin alone, resulting in weight loss, improvement in blood glucose levels, increase in total and free testosterone levels and improvement in erectile dysfunction. The study concluded that there could be potential vasculature effects that occurred with the addition of GLP-1 RA.
To conclude, in patients who qualify for GLP-1 RA drugs, there could be both potential benefits in overall pelvic functioning but also potential increase in dysfunction if there is present pelvic floor dysfunction previously.
Practical Considerations
For individuals experiencing pelvic floor dysfunction who are also managing obesity or type 2 diabetes, semaglutide may offer a multifaceted approach to health improvement. However, it is crucial to approach treatment comprehensively:
- Consult Healthcare Providers: Always discuss any new medication or treatment approach with your healthcare provider, especially when dealing with complex conditions like pelvic floor dysfunction.
- Integrate a Holistic Approach: Alongside semaglutide, consider pelvic floor physical and occupational therapy, lifestyle modifications, and other treatments tailored to pelvic health.
- Monitor and Evaluate: Regularly assess how the medication is impacting both your weight and pelvic floor symptoms, and adjust treatment plans as needed.
Conclusion
Semaglutide has proven to be an effective tool for managing type 2 diabetes and aiding in weight loss. While direct evidence linking semaglutide to improvements in pelvic floor dysfunction is still emerging, the medication’s benefits in weight management and metabolic health may offer indirect advantages for individuals dealing with pelvic floor issues. As always, personal health decisions should be guided by a thorough discussion with healthcare professionals to ensure a comprehensive and effective approach to treatment.
Research
https://pubmed.ncbi.nlm.nih.gov/37615353/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4559236/
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10533252/)
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10533252/).
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By PHRC Admin
Over the course of the years here at Pelvic Health and Rehabilitation Center, we have had numerous opportunities to collaborate with other professionals in the field. This blog is a compilation of the various articles, podcasts and resources we wanted to put in one place for you to be able to check out!
Article Reviews
‘Just do kegels’ is tired. What’s next for this hot women’s health market?
This LA Times article discusses how pelvic pain has historically been overlooked and misdiagnosed by healthcare providers, leading to a lack of awareness and research around the issue. However, in recent years, there has been growing recognition of the impact of pelvic pain on patients’ quality of life, leading to increased awareness and advocacy efforts. Despite this progress, many healthcare providers still lack adequate training and resources to diagnose and treat pelvic pain effectively. Women, people of color, and those from low-income communities are especially vulnerable to disparities in care. This article helps highlight efforts to improve provider education and increase access to specialty care for patients with pelvic pain. By addressing these gaps in care, we can work towards improving the lives of those who suffer from this debilitating condition.
Recurrent UTIs Can Lead to Pelvic Floor Dysfunction
Recurrent UTIs can lead to pelvic floor dysfunction and pain after the infection is cleared, as most people do not realize impaired pelvic floor muscles mimic UTI symptoms. Preventing UTIs is key for pelvic health so we stay on top of the research. A new report highlights how a type of bacteria may be at play, shedding light on potential new treatments. This NPR article, Why do some people get UTIs over and over? A new report holds clues, discusses why some individuals are more prone to urinary tract infections (UTIs) than others. Researchers have found that a type of bacteria called Gardnerella vaginalis may play a role in recurrent UTIs, as it can form a protective biofilm that makes it difficult for antibiotics to eliminate it. This biofilm can also make it easier for other bacteria, such as E. coli, to take hold and cause UTIs.
FDA Approves Treatment for Menopause-Related Hot Flashes
FDA approves a game-changing, non-hormonal treatment for menopause-related hot flashes! Say hello to Fezolinetant, offering relief without hormones. The U.S. FDA has approved Fezolinetant, a first-of-its-kind non-hormonal drug for treating hot flashes associated with menopause. Developed by Astellas Pharma, Fezolinetant works by blocking neurokinin 3 (NK3) receptors in the brain, which are responsible for causing hot flashes.
This approval marks a significant milestone, as it offers an alternative treatment option for those who cannot or do not want to take hormone replacement therapy (HRT). Clinical trials have shown that Fezolinetant is effective in reducing the frequency and severity of hot flashes. The drug also demonstrated a favorable safety profile, with the most common side effects being headache, urinary tract infection, and upper respiratory tract infection. Fezolinetant will be available under the brand name Quviviq and is expected to be launched in the United States in January 2023. This new treatment option brings hope to millions of women experiencing menopause-related hot flashes and provides an alternative to hormone-based therapies.
The Sexual Health and Wellness Institute
Treating Vulvar Pain: Q&A with Physical and Occupational Therapists Stephanie Prendergast
Good Clean Love
Pain from Vulvodynia and Dyspareunia
Podcasts with Stephanie Prendergast, MPT, PHRC Cofounder Pasadena
“Airtalk” on LAist with Larry Mantle
Listen to the interview here– 1:11:45: The Pain and Shame of Vulvovaginal Disorder with guest: Kayna Cassard, MFT, sex therapist and painful sex specialist and Chailee Moss, M.D., gynecologist with The Centers for Vulvovaginal Disorders.
Radiant Life Design
Expert Interview with Stephanie Prendergast, Physical and Occupational Therapists and Co-Founder of Pelvic Health and Rehabilitation Center– “During this live interview and Q&A with Stephanie, she gives us an overview of how pelvic floor physical and occupational therapy can help relieve pelvic pain as well as how to find the right physical and occupational therapists and what to expect during your sessions.”
Gynogirl Presents Sex, Drugs, and Hormones
Navigating Pudendal Nerve Disorders: Insights from Stephanie Prendergast– “As we discuss pudendal neuralgia’s insidious nature, you’ll learn about its varied symptoms, the importance of the Nantes criteria for proper diagnosis, and why a simple nerve block isn’t always the answer. We hear about the trials of pelvic floor therapy and how hope can be found in region-based methods and coordinated medical teamwork. Remember that health is a collaborative journey, and it’s vital to have a coordinated team of professionals for treatment.”
HEM Support
Fostering a Better Pelvic Health Community: featuring Dr. Stephanie A. Prendergast MPT– “Our founder Lauren recently sat down with Dr. Stephanie Prendergast, co-founder of the Pelvic Health & Rehabilitation Center. Dr. Stephanie shared her journey into pelvic health, the critical importance of pelvic floor education, and the gaps in medical training that often leave women without the support they need. From understanding the basics of pelvic health to recognizing early symptoms, their chat highlights how crucial it is to pay attention to your body and seek help early.”
The Body Nerd Show
“When was the last time you stretched your pelvic floor? Or strengthened it? Or even thought about it for that matter? On today’s episode, I’m joined by pelvic health physical and occupational therapists Stephanie Prendergast and she’s sharing everything you didn’t know you needed about the pelvic floor. So whether you have low back pain, hip pain, or pelvic floor issues or, you just love to nerd out about the body – today’s episode is for you! On today’s episode, you’ll learn: Why you might not need kegels, When you should see a pelvic floor PT, and how to find a pelvic health physical and occupational therapists in your area.”
Femme Farmacy
“We are joined today by Stephanie Prendergast, MPT, co-founder of The Pelvic Health and Rehabilitation Center. Pelvic floor physical and occupational therapy is an integral part of any woman’s healing journey and has many applications for women whether it be pelvic pain, pregnancy & childbirth or musculoskeletal issues. Stephanie is an icon in the space and has tirelessly advocated for people with pelvic floor dysfunction, pelvic floor physical and occupational therapistss and the field of pelvic health as a whole. She reaches millions of people around the world through her blog and is considered one of the foremost minds on pelvic health. If you’re struggling with pelvic pain of any kind, this episode is a must listen!”
Between Two Lips
The Between Two Lips Podcast is dedicated to all things pelvic health for women. Myself and my guests discuss topics such as incontinence, prolapse, pelvic pain, pregnancy, birth, perimenopause, menopause, sex and pelvic surgery. Nothing is TMI.
Interstitial Cystitis Association Podcasts
“Overview of physical and occupational therapy for bladder pain and general pelvic pain: Physical and Occupational Therapists Stephanie Prendergrast discusses the internal and external techniques used in pelvic floor therapy during the joint meeting of the International Continence Society and the International Urogynecological Association in Toronto. Prendergrast is a leader in developing techniques for pelvic floor therapy for interstitial cystitis patients with high tone pelvic floor dysfunction.”
Informed Pregnancy Podcast
“What is the pelvic floor? Triggers for pelvic dysfunction? Small but mighty, your pelvic floor muscles play important roles in sexual and reproductive health. Learn about normal pelvic floor structure and function, how to care for your pelvic floor in general and in relation to pregnancy and postpartum and how to recognize when symptoms may be related to your pelvic floor.
Podcasts with Jandra Mueller, MS, DPT, PHRC Encinitas
Endometriosis Unplugged with iCareBetter
The podcast where we dive deep into the world of endometriosis, sharing personal stories, expert insights, and practical advice for better care. Endometriosis is an estrogen mediated, inflammatory disease where endometrial-LIKE tissue is found outside of the uterus and impacts one in 10 people assigned female at birth.
Check out Episode #5: Stephanie Prendergast and Elizabeth Akincilar, founders of Pelvic Health and Rehabilitation Center, share about the management of pelvic pain and endo!
Now You Know
Why aren’t we talking about endometriosis?– “Anita Jones suffers from endometriosis, a disease that impacts more women than you may know. It is extremely painful and affects the lives of one in 10 women. Yet, most cases go undiagnosed or misdiagnosed for years. That’s what happened to TV presenter Anita Jones. She was told by doctors that her debilitating period pains were normal. Sound familiar? In this episode of Now You Know, Anita tells us about her journey with endometriosis. We also talk to an expert who helps us understand what exactly endometriosis is and its symptoms. And did you know some women with endometriosis may experience infertility?”
The Chronic Illness Therapists
Pelvic Pain, Endometriosis and Pelvic Floor Physical and Occupational Therapy
About the Podcast: Disrupting the mental health and medical system for people with chronic, invisible illnesses. We will no longer accept lack of answers, empathy, and guidance from the professionals we are told to trust. It’s not in your head, you are not a burden, and we’ll prove that to you one episode at a time.
Dr. Ruscio Radio
How Pelvic Floor Dysfunction Can Impact Your Health– “The health of the pelvic floor is key to our overall health in important ways. My podcast guest today is pelvic health expert Jandra Mueller, and she explains how gastrointestinal issues such as IBS and SIBO, hormonal imbalances, pregnancy, erectile dysfunction and trauma can all impact the health and tone of the pelvic floor, and how stigmas around normal bodily functions can present obstacles to patients seeking the help they need. Jandra dispels some myths and fears around pelvic floor issues, and discusses a variety of non-surgical interventions for pelvic floor concerns that can improve wellbeing and quality of life for patients.”
Abdominal Distention, Dr. Ruscio’s New Protocol– “Back on the podcast to discuss the surprising connections between pelvic floor health and gut health. This time, she weighs in on the three-step protocol I’ve developed to improve abdominal distension and how posture, breathwork, and emotions all tie into healing the gut and feeling better”
New Research to Resolve Constipation, Food Reactivity & Reflux
IC Wellness
Endo & IC with Dr. Jandra Mueller, DPT, MS
Part 2- Jandra Mueller, DPT, MS is a pelvic health physical and occupational therapists at The Rehabilitation Center. In addition to her doctorate in physical and occupational therapy, she also has her Master of Science in integrative health and nutrition. In Part one Episode 58 Jandra covered the root causes of Endo, and she is back for Part two to discuss diet and lifestyle.
Lotus
Understanding Endometriosis- Jandra Mueller, DPT, MS, PHRC, shares her personal and professional experiences with endometriosis, a condition that affects roughly one in ten people assigned female at birth. Join us for an incredibly insightful conversation!
The Hormone Puzzle Podcast
Pelvic Health and Your Fertility with Jandra Mueller, DPT, MS
This list is not exhaustive as our team has been interviewed various times since our opening in 2006! This list may be updated in the future to include other podcasts and articles we have been featured on. Are you interested in having us on your podcast or interviewing a team member for an article? Please send your inquiries to [email protected] with details so we can get in touch!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!