Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Stephanie Prendergast, PHRC Cofounder
What is Vulvodynia? Is it a symptom, a disease, or a syndrome? What does the term ‘Vuvlodynia’ mean to people with vulvar pain, pelvic pain specialists, medical professionals, and the community in general?
In a previous blog post I wrote about how in the pelvic pain world, diagnosis does not dictate treatment. Many pelvic pain diagnoses simply describe the location of the pain, but they do not tell us how the problem developed, what is causing it, or how to treat it. “Vulvodynia” means pain in the vulva, and I consider that to be a symptom.
On April 8th and 9th, I was honored to be one of 28 vulvoaginal experts invited to participate in the International Consensus Conference on Vulvovaginal Pain (Vulvodynia) Nomenclature (click here for the entire list of participants).The event was organized by Dr. Andrew Goldstein and ISSWSH. The motivation for a consensus meeting originated because “there is an unmet medical need for a comprehensive, evidence-based set of vulvovaginal pain diagnoses that can be easily utilized by both expert and non-expert healthcare providers to establish diagnoses in their patients and to guide treatment.”
The Mission of the group was to develop evidence-based consensus among experts, experienced in the diagnosis, evaluation, treatment and/or research in vulvovaginal pain for women, for appropriate nomenclature and definitions of female sexual dysfunctions. These definitions must be applicable across disciplines and useful in both clinical and research settings, and to serve as the basis of ICD codes for women’s sexual health problems.
The conference began with a historical overview of current vulvar pain terminology:
“Vulvodynia has been defined by the International Society for the Study of Vulvovaginal Diseases (ISSVD) as chronic vulvar discomfort, most often described as a burning pain, occurring in the absence of relevant visible findings or a specific, clinically identifiable, neurological disorder,”Patients can be further classified by the anatomical site of the pain (e.g. generalized vulvodynia, hemivulvodynia, clitorodynia) and also by whether pain is provoked or unprovoked.” Chronic is considered longer than 6 months.
The above definition was voted and agreed upon…..in 2003. I began working with people with pelvic pain in 2001, and I can tell you there have been tremendous advances in the management of these disorders. Reading this archaic, horrendous definition left me thinking WTF? How would I feel if I was diagnosed with Vulvodynia, and read online that it is chronic (doomed for life!), absence of relevant visible findings (I suppose it is all in my head and the fact that I am in pain is ‘irrelevant’), and that I would be ‘classified’ based on where my pain is?
I can say for sure that we do have identifiable causes, we do have visible findings, and women with vulvar pain have a treatable condition, NOT an unresolvable medical mystery. I was grateful this conference had been organized, because patients are being thrown under the bus. Tensions were running high as we shifted into the morning lectures on possible physiological causes of vulvar pain:
- Inflammation (David Foster, MD MPH)
- Neuroproliferation (Jacob Borenstein, MD, MPA)
- Hormonal (Andrew Goldstein, MD, FACOF, IF)
- Genetic ( Nina Bohm-Starke MD, PhD)
- Peripheral Neuropathic (Lee Dellon, MD, PhD, FACS)
- Central Neuropathic (Melissa Farmer, PhD)
- Musculoskeletal (me!)
- Psychosocial (Caroline Pukall, PhD, C.Psych)
- Systemic (Deborah Coady, MD)
Listening to the lectures on these 9 evidence-based vulvar pain subsets confirmed why I consider ‘Vulvodynia’ a symptom and not a helpful diagnosis. I used five actual case examples to make this point that more developed nomenclature is necessary to help suffering women get appropriate treatment. The five women I described all have ‘Vulvodynia’.
Leah is 30 years old. Her vulvar pain developed following multiple urinary tract infections that were appropriately treated with antibiotics but unfortunately led to multiple yeast infections. Her treatment plan included manual therapy to treat high-tone pelvic floor muscles and vulvar connective tissue restrictions. Leah also needed to work with a naturopathic doctor to get to the underlying cause of the repetitive infections. Both the musculoskeletal dysfunction, inflammation, and the systemic infections were primary causes of Leah’s vulvar pain.
Michelle is 30 years old. Her vulvar pain developed after she was in a car accident. During the car accident her knees hit the dashboard, causing sacroiliac joint dysfunction. Because of the close relationship between the sacroiliac joint ligaments and the pudendal nerve, she subsequently developed pudendal nerve irritation which in turn caused a high-tone pelvic floor and constant vulvar pain. Because of the pudendal nerve irritation, Michelle could not initially tolerate physical and occupational therapy. I referred her for a pudendal nerve block (peripheral neuropathic treatment), then we resumed physical and occupational therapy that included manual therapy as well as orthopedic treatment strategies for her sacroiliac joint (musculoskeletal treatment), which was a driving factor in Michelle’s case (but clearly not in Leah’s case above).
Gwen is 49 and a triathlete. Her vulvar pain started two weeks after she started an exercise regime called Crossfit. She noticed the pain when she attempted to have intercourse. This scared her; she did a google search on ‘pain with sex’ and thought she had pudendal neuralgia. I fully expected her to have numerous trigger points and pelvic floor tone issues based on her athletic history. Instead, I discovered that her periods have been irregular and she is in peri-menopause. Upon inspection, her vulvar tissues were thin and lacking estrogen. Her musculoskeletal structures were totally normal. The vulvar pain with intercourse coincided with a change in her exercise routine, but it also coincided with resuming intercourse after a period of inactivity and perimenopause. Her treatment consisted of topical hormonal cream and she did not need physical and occupational therapy.
Michelle, who is 23 years old, always had painful periods and was using oral contraceptives to reduce her painful periods. She began to experience vulvar pain with tampon use, and for two years she experienced vulvar pain with insertion. She then developed a Bartholin’s cyst that was surgically removed. Following this procedure, she felt daily pain at the incision site. Upon physical examination I could feel scar tissue at the surgical incision site and identified other musculoskeletal findings that were likely contributed to her provoked pain. It is plausible that androgen insufficiency from oral contraceptives was a contributing cause to the provoked vulvar pain that developed with insertion and that a neuroma secondary to surgery was contributing to the daily unprovoked pain. Her treatment involved cessation of the birth control pill, topical and systemic hormonal therapy, surgical excision of the neuroma, and physical and occupational therapy. Her case was hormonal, genetic, peripheral neuropathic, and musculoskeletal.
Barb is 53 and the mother of two children, ages 25 and 27, delivered vaginally. She underwent a complete hysterectomy and anterior vaginal wall repair for uterine and bladder prolapse. Mesh was used in this repair. Following surgery, Barb developed severe and debilitating vulvar pain. Her pain was caused by peripheral nerve irritation from the mesh and it eventually was removed. Following the removal of the mesh she underwent pharmacologic therapy for CNS hypersensitivity, pudendal nerve blocks, and physical and occupational therapy, which resulted in resolution of her symptoms.
All five women have ‘Vulvodynia’ for different reasons. And we do know what they are.
Following the physiology lectures, we heard presentations on physical examination findings and tests for women with vulvar pain. These include visual and palpation examination of the vestibule, examination of the pelvic floor muscles, histopathology, laboratory testing and psychometric evaluation.
Next, we were broken into 5 small subgroups with four objectives in mind:
- Develop, through expert consensus, nomenclature describing vulvovaginal pain (vulvodynia) and subgroups of vulvovaginal pain.
- Utilize the nomenclature developed to establish diagnostic criteria for vulvodynia and its subgroups.
- Utilize the nomenclature developed to establish evidence-based treatment guidelines.
- Utilize the nomenclature developed to develop suggested areas of future research.
On day two, one leader from each breakout group presented their group’s suggested nomenclature; there were five options to chose from. 28 of us voted and one group’s option was chosen. We then spent the rest of the day in animated, thoughtful, heated and intense discussions, debating what the evidence does and does not tell us, how nomenclature can support both researchers and clinicians, and how to support nonexpert and expert clinicians and most importantly, women suffering from vulvar pain.
At the 13th hour we did reach a consensus!
- We agreed to change the title of Vulvar pain classification from ‘Chronic Vulvodynia’ to ‘Persistent Vulvar Pain’.
- Evidence supports 7 subclassifications of vulvar pain
- Infectious
- Inflammatory
- Neoplastic
- Neurological
- Trauma
- Iatrogenic
- Hormonal deficiencies
- Vulvar pain can exist without an identifiable cause
- Vulvar pain can be described as localized, provoked, by onset (primary or secondary) or by temporal patterns (intermittent, persistent, constant, immediate, delayed)
- Vulvar pain is associated with certain factors (IMPORTANT: there was not enough evidence to support cause or effect, we can state we know vulvar pain can exist with the following impairments)
- Neuoproliferation
- Musculoskeletal
- Psychosocial
- Genetic
- Hormonal
- Neurological
- Peripheral neurologic
- Central neurologic
- Comorbid pain syndromes
This classification has the potential for tremendous improvement in clinical care for our suffering patients. I was honored to be part of it and to see how far we have come in 15 years, we just need our nomenclature to show it.
The results of our meeting are currently being written up and submitted to the International Pelvic Pain Society, The International Society for the Study of Vulvovaginal Disease, and The National Vulvodynia Association. We are hoping that these three societies will adopt the new nomenclature and that they will become part of the ICD coding.
Readers we want to hear from you! If you have any questions please do not hesitate to leave them in the comment section below.
And if you haven’t already, SUBSCRIBE to this blog (up top, to the right, under my photo!), so you can get weekly updates in your inbox, and follow us on Facebook and Twitter where the conversation on pelvic health is ongoing.
All my best,
Stephanie Prendergast, MPT

FAQ
What are pelvic floor muscles?
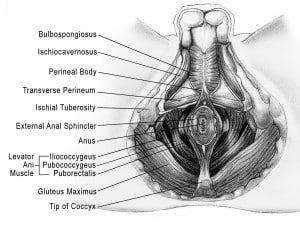
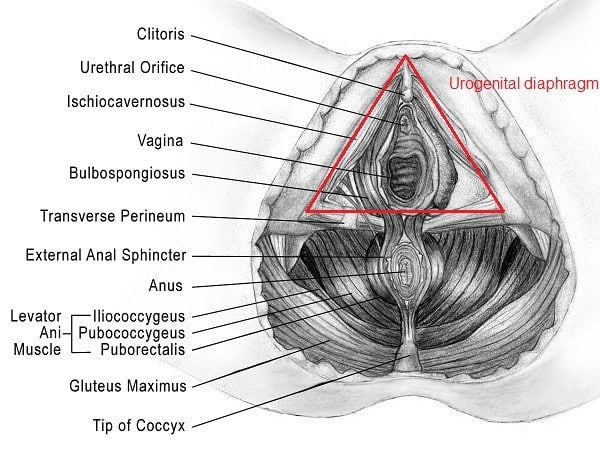
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
Chronic Prostatitis! It’s not something discussed at a baseball game or at a family gathering. However, it is estimated that between 2-14% of men worldwide are diagnosed with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS)1. But what exactly is CP/CPPS? According to the National Institutes of Health, CP/CPPS, also known as category III prostatitis, is characterized by pain in the pelvic area for 3 of the last 6 months without any signs of infection, malignancy, or structural abnormalities 2. In fact, it is the number one reason why men under the age of 50 visit a urologist. 95% of men with a “prostatitis” diagnosis actually have CPPS and in fact have NOTHING wrong with the prostate itself. Instead, there are almost always problems with the musculoskeletal system, including the pelvic floor muscles.
Men with CP/CPPS report genital and urinary symptoms including the following:
- Urinary frequency
- Urinary urgency
- Burning sensation with urination
- Hesitancy with starting stream
- Incomplete emptying of the bladder
- Pain in the perineum – region between the testicles and anus
- Pain in the genital region
- Pain in the lower abdomen and/or low back
- Pain with ejaculation
- Pain with bowel movements
- Erectile dysfunction
How is CP/CPPS Diagnosed?
Medical doctors will conduct a systemic workup to exclude other possible diagnoses, such as cancer, painful bladder syndrome, or bowel pathologies. An extensive workup may consist of a urinalysis and culture, PSA study, cystoscopy, different types of imaging, such as a transrectal ultrasound, and any other studies a doctor may deem necessary. He/she will also conduct a thorough history exam asking questions regarding symptoms, past medical history, psychosocial history, family history, and medication. It is best to report all of your medical history to your doctor, even the things you might not find significant, such as cardiovascular disease or irritable bowel syndrome (IBS). Researcher are finding a correlation between CP/CPPS and other systems in the body, such as the gut and cardiovascular system. It is necessary to address and treat all impairments found when treating a patient with CP/CPPS.
Men with CP/CPPS have varying causes of their symptoms and therefore one standard treatment protocol, such as antibiotics, does not work for everyone. Repeated courses of antibiotics without a positive infection is NOT acceptable treatment. Research shows CP/CPPS is multifaceted with varying presentations. It is important to acknowledge and treat all possible causes of the symptoms.
The UPOINT classification system was created to help guide multimodal therapy for CP/CPPS. UPOINT is an acronym for urinary, psychosocial, organ-specific, infection, neurologic/systemic, and tenderness of muscles. These are all areas that can contribute towards CP/CPPS symptoms and need to be addressed. Research has shown that pelvic floor physical and occupational therapy is the FIRST line of treatment for the musculoskeletal impairments commonly found with CP/CPPS.
A physical and occupational therapists’s evaluation consists initially of a subjective exam. A PT will ask questions similar to the doctor’s history exam. We will want to know more about the behavior of the urinary, sexual, and pain symptoms, such as the quality, location, frequency, and severity of the pain, history of the symptoms, such as when they began, past medical history including surgeries and/or other injuries, psychosocial history, and questions regarding medication.
Next, a physical exam is conducted, which consists of an observation of the body looking for any abnormalities from the head down to the feet, an assessment of the pelvic girdle alignment (checking to see if the hips are in alignment), an assessment of the range of motion of the hips and low back, as well as palpation of the muscles in the abdomen, low back, hips, buttocks, thighs, and pelvic floor. When we palpate muscles, we are looking for tenderness, tightness, and myofascial trigger points in the muscles. Here at PHRC, we also assess for connective tissue restrictions throughout the abdomen, thighs, buttocks, low back, and bony pelvis. Please see our blog The Role of Connective Tissue Manipulation to learn more.
During the physical exam, an intrarectal exam is also performed to assess the pelvic floor muscles. We once again are looking for tightness, tenderness, and myofascial trigger points as well as pudendal nerve hypersensitivity. It is also important to assess motor control of the pelvic floor. Can our patient contract, relax, and lengthen the pelvic floor muscles when we ask him to? A primary goal of physical and occupational therapy is to teach our patients how to regain control of their muscles in order to reduce their symptoms and improve muscle function.
What is physical and occupational therapy treatment?
Physical therapy treatment focuses on the neuromuscular impairments. It is very common for men experiencing CP/CPPS to present with increased muscle tone and myofascial trigger points, connective tissue restrictions, and altered peripheral nerve function throughout the pelvic girdle area, abdomen, pelvic floor muscles, and thighs. Manual therapy, especially intrarectal manual therapy, is often necessary to normalize these impairments. Training patients to voluntarily relax and lengthen the pelvic floor is also a must. It is common for patients experiencing pain to guard, which contributes towards pelvic floor tightness and trigger points. Men suffering from CP/CPPS benefit from learning to relax their pelvic floor muscles since these muscles play such a large role in their pain. We call this exercise “Pelvic Floor Dropping” and we teach our patients how to do this early on in their treatment plan. To learn how to do a pelvic floor drop please click here.
More often than not, the symptoms of CP/CPPS are associated with tight muscles rather than weak muscles. Therefore, the majority of men suffering from CP/CPPS will likely NOT need to perform Kegels as part of their treatment program.
How long is this going to take?
Typically, men with CP/CPPS have physical and occupational therapy 1 -2 times per week, usually for 3 – 6 months. The timeline will vary based on the chronicity, severity, and other contributing factors.
Men with CP/CPPS may have multiple impairments contributing towards the pain, such as inflammation, stress/anxiety, gut pathology, infection, systemic pain, for example chronic fatigue syndrome. A multidisciplinary approach is the most effective strategy when confronted with multiple causes of pain. Part of our job as a PHRC physical and occupational therapists is to coordinate the overall treatment plan with other providers that our patients are being treated by. Other treatments may include acupuncture, pharmaceutical management, procedures such as trigger point injections, botox injections, nerve blocks, and psychological services such as cognitive behavioral therapy.
Will prostatitis ever go away?
YES! Physical therapy involves developing an assessment as to how the symptoms developed and what impairments need to be treated. This open discussion between the physical and occupational therapists and the patient leads to the development of reasonable short term and long terms goals and a strategy for achieving these goals. Although improvement does not happen overnight, it does happen!
CP/CPPS may not be a common subject spoken about at the water cooler, however for millions of men around the world it is a part of their daily life. These men do not have to live with the symptoms. Treatment is available!
Readers we want to hear from you! If you have any questions regarding CP/CPPS, please do not hesitate to leave them in the comment section below.
And if you haven’t already, SUBSCRIBE to this blog (up top, to the right, under Stephanie’s photo!), so you can get weekly updates in your inbox, and follow us on Facebook and Twitter where the conversation on pelvic health is ongoing.
- Konkle, K. and Clemens, J. New Paradigms in Understanding Chronic Pelvic Pain Syndrome. Curr Urol Rep. 2011 Aug; 12 (4): 278-83.
- Pontari, M. and Giusto, L. New Developments in the Diagnosis and Treatment of Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Curr Opin Urol. 2013 Nov; 23 (6): 565-9.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
I recently had the opportunity to get together with a group of moms through the Holistic Moms Network (HMN) in Fremont, CA. I had put together a talk on what I thought were the most common issues moms of any age might be facing, but I wanted to spend some time asking them what they felt they needed more information about, specifically.
The answer was a resounding question, “How, exactly, am I supposed to do a kegel?”
This answer was not surprising to me. Most women are instructed by their obstetrician (OB) to ‘do your Kegels’ without much direction. This is because an OB’s focus is to keep moms and babies safe, not to teach women how to properly do a kegel. Unfortunately, because musculoskeletal questions associated with pregnancy arise, OBs are put in a position to provide information that lies outside their area of expertise. This is where pelvic floor physical and occupational therapistss can step in and help out.
The problem with just telling someone to ‘do your Kegels” is that, according to recent research, 51% of women could not perform a Kegel properly with verbal cueing alone. And 25% of the women in the study were actually performing the attempted-Kegel in a manner that could promote incontinence and pelvic organ prolapse – the very issues kegels are suppose to help! Kegel confusion has been confirmed through my own clinical experience and conversations with new moms. Most women reading this are probably nodding their heads, yes!
In order for readers to get the full picture of how to Kegel, let’s start with the anatomy:
There are two layers of pelvic floor muscles.
The most superficial (closest to the skin) are known as the urogenital diaphragm. These are the muscles that are primarily responsible for helping to close the urethra and anus so that we don’t leak urine/gas/stool when we don’t want to. i.e. laughing, coughing, sneezing, or jumping on the trampoline. When performing a kegel properly you may be able to bias these muscles by concentrating on closing the urethra or anus, and the vaginal opening.
The deeper layer of muscles (closer to the organs) are called the levator ani. These muscles are largely responsible for supporting our pelvis, bladder, uterus and rectum throughout our lifetimes as the forces of gravity, childbearing/rearing, respiratory issues, constipation weigh us down.
Here is a good video of the pelvic floor anatomy and if you haven’t yet become familiar with your vulva read Rachel’s blog.
The basic idea to keep in mind when trying to perform a pelvic floor muscle contraction (kegel) is to squeeze the urethra/vagina/anus closed and lift up. It is an “in and up” motion. When I am palpating someone’s pelvic floor muscles to assess for strength-I am looking for the muscles to squeeze my finger and gently pull it up (toward the head). It is the exact thing that we do if we stop our urine mid-stream. This is not something to get in the habit of doing during urination, due to the risk of urinary tract infections, however it is ok to try one time if it can help you isolate the correct muscles.
Over the past several years at PHRC, I’ve discovered clever cues to help patients find and contract their pelvic floor muscles. Here is my list, but I am sure that there any many other tips/tricks out there. Please share yours in the comments section:
-pull your pubic bone and tailbone together
-bring your sits bones together
-stop the flow of urine
-wink the anus
-nod the clitoris
-pull in like you are putting on a tight pair of jeans
-sit on a chair and pull your perineum up and away from the surface
-think of the muscles as an elevator and “lift” up towards your head
-pull the underwear in
-hold back gas
-like you’re holding a tampon in
If you still feel lost you can try inserting a finger into the vagina or anus and actually FEEL the muscles. C’mon just do it.
You can also try curling your toes while attempting to kegel. (Check out this picture of the homunculus to see how closely related the pelvic floor muscles and feet are.) Also, stay tuned for an upcoming blog on toe curling orgasms!
If you have made it this far and are still shaking your head in confusion/frustration here’s what you can do:
There are many different products out there that claim to be pelvic floor strengtheners. I strongly recommend checking with a physical and occupational therapists before choosing one, so you get the one that’s right for you. One tool that I have found to be pretty effective and harmless is this pelvic floor educator from Current Medical Technologies. It works like this: you insert it into the vaginal canal and if you are doing a kegel correctly, it gives you visual confirmation.
At PHRC we will sometimes use biofeedback or neuromuscular electrical stimulation (NMES) to help find and isolate these muscles. Biofeedback works by projecting the electrical signals from your pelvic floor muscles on to a screen so that you can see when you are contracting properly. NMES works by supplying electrical signals directly to the muscles making them contract.
Kegels alone are rarely a solution for overall musculoskeletal health but rather one component of an individualized exercise regime for new moms. It is important to learn to do them properly if they are part of your fitness regime (Read here for more info on postpartum rehab). However, not everyone needs to be doing a kegels on a regular basis. In fact, for some people it might even cause dysfunction. Read here to learn why kegels are not right for all of us.
Hopefully this post validates why you might feel confused about how to perform a Kegel, they are definitely an acquired skill! When in doubt, consult with a pelvic floor physical and occupational therapists. They can provide you with an individualized program that is right for you and ensure you know how to do each exercise right. To find a pelvic floor PT: click here.
*Men: I haven’t forgotten about you. Because we are focusing on what mom’s want to hear about I did not talk about the male pelvic floor. But FYI kegels can be really important for you too! Check out these past blog posts for relevant info: here and here.
Readers we want to hear from you! Are you confused about kegels? Please share in the comments section below!
And if you haven’t already, SUBSCRIBE to this blog (up top, to the right, under Stephanie’s photo!), so you can get weekly updates in your inbox, and follow us on Facebook and Twitter where the conversation on pelvic health is ongoing!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.