Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Stephanie Prendergast, MPT, Cofounder PHRC Pasadena
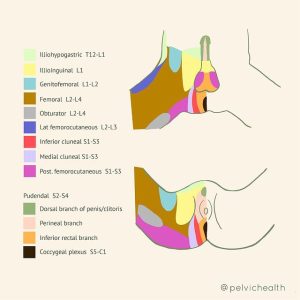
Many people experiencing burning in their pelvis or pain while sitting may google their symptoms and quickly arrive at a diagnosis of Pudendal Neuralgia. The pudendal nerve is an important pelvic nerve, however, the ilioinguinal nerve, the obturator nerve and the genitofemoral nerves can also cause pelvic pain and should not be overlooked. It is crucial to have a proper diagnosis in order to get relief and that starts with anatomy and physiology!
Starting with the basics, the term neuralgia simply means pain in the territory of the nerve. Any nerve can turn into neuralgia if it gets compressed, over stretched, or otherwise injured through surgery or trauma.
Peripheral nerves are responsible for sensation and movement. When injured, neuropathic pain can result. Symptoms of neuropathic pain include burning, tingling, shooting, stabbing, jabbing, itching, numbness, pain reaction to non-painful stimuli (allodynia), and exaggerated reactions to painful stimuli (hyperalgesia), and altered reactions to temperature.
It often surprises people to learn that most neuralgias are diagnosed simply based on the characteristics and locations of the pain. Electrophysiologic testing and imaging techniques are not as helpful as we would like them to be for making a diagnosis. The most important information our patients tell is their (suspected) mechanism of injury, exactly where the pain is and exactly what it feels like.
Let’s define the 4 important pelvic nerves to consider in order to differentially diagnose pelvic neuropathic pain. Please note there are more nerves to consider and some people can have multiple neuralgias at the same time.
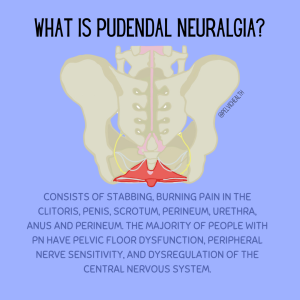
Pudendal Neuralgia
The pudendal nerve contains autonomic, sensory and motor fibers. The autonomic component of the pudendal nerve distinguishes it from the other three nerves in this blog post. The autonomic nervous system is designed to keep us functioning automatically without us thinking about it. The pudendal nerve contributes to urinary, bowels and sexual functioning in addition to its sensory and motor features. This nerve has a lot of pelvic responsibility!
Definition
Pudendal neuralgia consists of stabbing, burning pain in one, some or all of the areas the pudendal nerve nerve innervates. These areas include the vulva (clitoris, labia minora/majora, inner labial area, vestibule), penis, scrotum, perineum, urethra, anus and perineum. This nerve innervates the pelvic floor muscles and is reflexively involved with sexual arousal and orgasm, and urine and stool storage and release. Pudendal neuralgia pain tends to get worse when sitting, squatting, and with trunk or hip flexion. The majority of people with pudendal neuralgia also have pelvic floor dysfunction and pain, peripheral nerve sensitivity in other nerves such as the posterior femoral cutaneous and sciatic nerves, and dysregulation of the central nervous system.
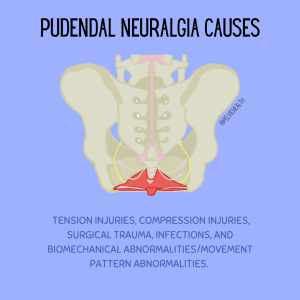
Causes
Pudendal Neuralgia can be caused by several different scenarios The most common include:
- Tension injuries: examples include constipation, childbirth, squatting exercises with faulty mechanics
- Compression injuries: examples include bike and horseback riding, prolonged sitting, faulty sitting mechanics
- Surgical trauma: examples include pelvic organ prolapse repair, obstetric injuries, hip surgeries
- Biomechanical abnormalities/movement pattern abnormalities of the lumbo-pelvic-hip complex and lower extremities
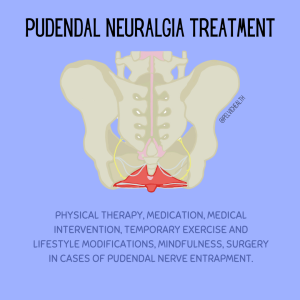
Treatment
Skilled pelvic floor physical and occupational therapy and medical management are the key to effective treatment of pudendal neuralgia, a successful treatment plan usually involves multiple interventions. The right medical team can help you determine which interventions will be most helpful and when to implement them. The entire team at PHRC specializes in the management of PN and frequently helps patients form the right medical team and decide on appropriate interventions.
Physical therapy involves manual therapy, pain science education, a home exercise program, modification to your current exercise program, and guidance with lifestyle modifications.
Because we treat a large volume of people with pudendal neuralgia at PHRC we have created a Resource List with blogs, videos, and reputable materials. PS – we are also working on a Pudendal Neuralgia e-book, make sure you subscribe to our newsletter and follow us on social media to get the e-book when it’s released!
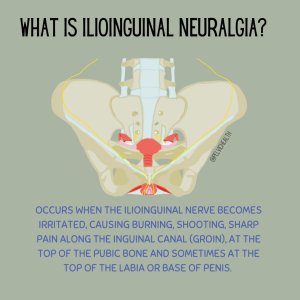
Ilioinguinal Neuralgia
The ilioinguinal nerve is a sensory and motor nerve. Ilioinguinal neuralgia can be confused with pudendal neuralgia because both nerves can cause nerve pain in the labia and penis. The primary difference between ilioinguinal neuralgia and pudendal neuralgia is that ilioinguinal neuralgia may cause pain in the inguinal canal (groin) whereas pudendal neuralgia will not. The pudendal nerve does not innervate the groin. People with ilioinguinal neuralgia may have (nerve) pain with sitting and this is one reason why people may understandably think they have pudendal neuralgia, however, if the anatomy does not match up it is likely not PN.
Want to see more images like this? Check out our Dermatome blog!
Definition
Ilioinguinal neuralgia occurs when the ilioinguinal nerve becomes irritated, causing burning, shooting, sharp pain along the inguinal canal (groin), at the top of the pubic bone and sometimes at the top of the labia or base of penis.
Causes
Inguinal hernia or inguinal hernia repairs, pubic symphysis trauma or separation, surgical trauma, scar tissue (ie Cesarean scars).
Treatment
Physical therapy, nerve blocks, medication, hernia repairs if present, neurectomy.
Obturator Neuralgia
The Obturator Nerve is a sensory and motor nerve. It can be confused with pudendal neuralgia because both will typically cause pain with sitting. However, the obturator nerve does not innervate the genitals and it can cause aching in the pubic area, groin, and upper medial thigh. Another difference between obturator neuralgia and pudendal neuralgia is that obturator neuralgia will also cause pain in the upper inner thigh whereas pudendal neuralgia will not.
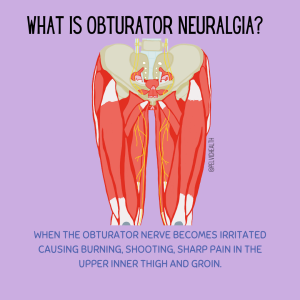
Definition
When the obturator nerve becomes irritated causing burning, shooting, sharp pain in the upper inner thigh and groin.
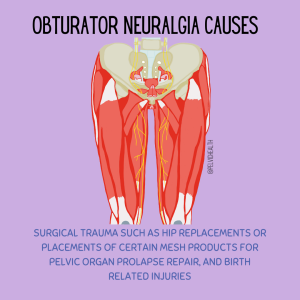
Causes
Surgical trauma such as hip replacements or placements of certain mesh products for pelvic organ prolapse repair, and birth related injuries
Treatment
Manual therapy, medications, nerve blocks, surgical removal of the mesh.
Genitofemoral Neuralgia
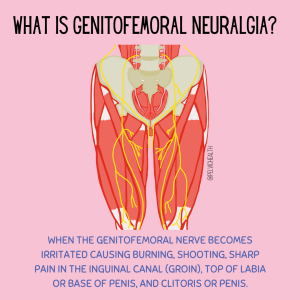
The genitofemoral nerve is a sensory and motor nerve. Genitofemoral Neuralgia can be confused with pudendal neuralgia because both nerves can cause pain in the clitoris and penis! The primary difference between genitofemoral neuralgia and pudendal neuralgia is that genitofemoral neuralgia is going to cause pain in the inguinal canal (groin) whereas pudendal neuralgia will not.
Definition
When the genitofemoral nerve becomes irritated causing burning, shooting, sharp pain in the inguinal canal (groin), top of labia or base of penis, and clitoris or penis.
Causes
Inguinal hernia or inguinal hernia repair, surgical trauma, scar tissue.
Treatment
Manual therapy, medications, nerve blocks, neurectomy.
Take Home Points!
- Any peripheral nerve can suffer injury and a neuralgia can develop
- A diagnosis for neuralgia can be made by understanding the character and anatomic location of the pain
- A physical examination by a doctor or physical and occupational therapists can help identify neuralgias in a clinical setting, sometimes imaging and/or electrophysiological testing may help the diagnosis
- A combination of skilled physical and occupational therapy and medical management leads to successful treatment!
If you are experiencing severe pain and you believe it is due to pudendal neuralgia, trigeminal neuralgia, or any type of pelvic pain, it’s time to check in with a pelvic floor physical and occupational therapists. Pain relief is possible with the right treatment plan and a multidisciplinary approach. Chronic pelvic pain is no joke! We understand the depths of severe pain at PHRC and pelvic floor physical and occupational therapy can be a part of your treatment plan.
Have more questions? Check out a short Q&A below!
Q: What can happen if Ilioinguinal neuralgia is left untreated? Should I be worried about my spinal cord or nerve pain?
A: If a neuralgia is left untreated, the pain could get worse and could also affect surrounding structures as your body tries to compensate due to the pain. We would recommend seeking treatment if you suspect that you have a neuralgia (whether it’s pudendal neuralgia or not).
Q: Is Ilioinguinal neuralgia common in pregnancy?
A: Ilioinguinal neuralgia can occur during pregnancy. We would recommend speaking with your OB/midwife if you suspect this and also working with a pelvic physical and occupational therapists.
Q: Is Ilioinguinal neuralgia hard to diagnose? What should I tell my doctors so they can test me extensively for it?
A: It can be difficult to diagnose and it is recommended to work with a pain management specialist to help further diagnose it as they are the ones most often prescribing the medication or performing the nerve blocks so they are more accustomed to common symptoms and ways to alleviate and treat the issue. Imaging may not show anything as this may be more functional versus an actual compression or entrapment. Nerve blocks can both be diagnostic and treatment. For example, if you have a nerve block and it reduces the pain that is important. Further treatment/ evaluation may be warranted if the pain returns, but it may be considered a positive diagnostic block.
Q: Can obturator neuralgia affect the hamstring as well? What nerve pain should I be looking out for?
A: Genitofemoral neuralgia primarily presents with pain in the genital region and sometimes the inner thigh, stemming from damage or irritation to the genitofemoral nerve. This pain can be sharp, shooting, or burning and may be accompanied by sensations like tingling or numbness, often triggered by activities such as walking or changing positions. On the other hand, obturator neuralgia is characterized by deep, aching pain in the inner thigh, occasionally radiating to the knee, caused by compression or injury to the obturator nerve. This condition may also lead to difficulties in adducting the thigh (bringing the thigh towards the midline of the body) and a sensation of tingling or numbness along the inner thigh. Both conditions share some overlapping symptoms, such as (nerve) pain and altered sensations, but they differ mainly in the location of the pain and the specific activities that exacerbate it.
Q: Is it possible to have both Pudendal Neuralgia and Genitofemoral Neuralgia? Do you have resources for nerve pain? I know pelvic pain can be tricky to diagnose (nerve pain being so close together).
A: Yes, it is possible to have both pudendal neuralgia and genitofemoral neuralgia.
Q: Many people have benefited from a TMS/ mind-body approach to PN, myself included. Do you aim patients towards those resources? (Mindfulness is only a small part of it.)
A: For anyone dealing with chronic pain, exploring the TMS/MindBody approach can be a worthwhile step. While mindfulness is an important component, the comprehensive strategies include identifying stressors, journaling, cognitive behavioral therapy (CBT), and sometimes engaging in physical activity against the instinct to avoid movement due to pain. We work with our patients through a multidisciplinary approach, so any referrals for other aspects of care are always given (when deemed appropriate for their case).
Stay tuned for a more in depth Q&A coming next month! Drop your nerve pain or pelvic pain related questions in the comments to have your questions answered in future Q&As!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Jandra Mueller, DPT, MS, PHRC Encinitas
We are back with an update on so many more cool products and tools to help you along your pelvic health journey. In case you missed it, part one of this series focused on some fun tools to help with improving pleasure and sexual health. Today we will present you with tools that can help you live your life with less discomfort, and improve your bowel and bladder habits.
Save this page so you can share it later- it’s the pelvic health information you need to know about! If you don’t see the pelvic health products you wanted to see, send us a note and we will check it out next round! From pelvic wands to premium products, we will cover it all!
Products for Urinary Dysfunction
Urinary incontinence (leaking pee when you have an urge, cough or sneeze), dysuria, or pain with urination, or even just difficulty going pee are very common symptoms that we treat here at PHRC. Going camping, hiking, or just don’t want to go in those nasty toilets? There are devices that can help that! Also, for more information on the importance of not hovering over the toilet please read our blog “Sit yo’ a$$ down! The importance of sitting on the toilet” .
 GoGirl
GoGirl
While not a new product, as it was featured in our blog a few years back, this device is used for people with vulvas so that we may be able to avoid those dirty porta-potties or less than ideal public bathrooms and not have to strain our pelvic floors by trying to gracefully balance ourselves over the seat of a toilet and strain our pelvic floor. These devices are available through Amazon, Target, Walmart, etc.
Poise Impressa
Even after so many years, I still love these and recommend them often! These look similar to tampons but they are for a different purpose, bladder leakage, and can help with some prolapse symptoms. Whether you are postpartum, an athlete, or you’ve suddenly noticed your panties have become wet (and not in the good way). There are devices known as pessaries that you need to be fitted for by a medical doctor or qualified nurse that are reusable. Poise impressa offers an alternative to this and are available over the counter so women can buy them and see if they are right for them. They are inserted into the vagina similarly to a tampon and provide support to the tissues that support our pelvic organs. These tissues can become lax after pregnancy and as a result of age-related changes and the hormonal insufficiencies of menopause. If you are using a bladder support or a pessary, you should ALSO be in pelvic floor physical and occupational therapy. These devices should be used as an aide to rehab to optimize the function of their pelvic floor muscles, not the solution.
Regain Urinary Leakage Belt
We now have options for our patients with penises! Leaking is never ideal and utilizing these in our patients who have undergone prostatectomies have been a game changer! This simple device is comfortable, safe, and easy to use. Used externally, this device is discreet and compact, making it simple to conceal. It can be applied or removed in seconds, using gentle pressure under the urethra to prevent urine leakage. Offered in three sizes – small, regular (fits most men), and large – it caters to diverse needs.
Pelvic Floor Trainers/Biofeedback Devices
So, Kegels. Well, these devices are pretty handy when you ACTUALLY do need to do Kegels, because yes, your pelvic floor should move – contract, relax and bulge. Studies show that given verbal instruction alone women cannot properly do a kegel. We advise seeing a pelvic floor physical and occupational therapists to assess if you need to do kegels and how to do them properly.
Since we last introduced these tools, a few new players have come on the market, and we love them! Previously, the Elvie was exclusively for people with vaginas and then KGoal came along and now we have an external device that can be used for all genders to benefit from! These upgraded biofeedback devices will tell you if you are doing what you are supposed to be doing, eliminating the mystery of if you are doing the exercise correctly or not. You can link it to your smart phone and based on your strength, it will create a program for you to help strengthen. It is definitely one of the more “fun ways” to do these exercises. There’s even pinball!
Elvie Pelvic Floor Trainer |
KGoal Classic |
Boost: Sit-On-Top |
| Using biofeedback, the gold standard of Kegel training, Elvie Trainer helps you visualize your pelvic floor while guiding you through each exercise. Simply insert Elvie Trainer and connect to the app. As you squeeze your pelvic floor muscles, your contractions move the gem through a targeted workout. | kGoal Classic is the original smart Kegel exerciser for women. It’s an interactive training system (device + app) that measures pelvic floor muscle function from inside the vagina and offers a unique combination of guidance, tracking, biofeedback and personalized workouts. Whether you’re just discovering your pelvic floor or are a seasoned Kegel workout warrior, kGoal Classic will help you get the most out of your exercise. | Boost™ is a revolutionary, interactive training system for your pelvic floor muscles. It consists of a sit-on-top device that measures pelvic floor muscle activation (you can leave your clothes on) and a smartphone app. It is designed to help with both strengthening (Kegel) exercise and relaxation (Downtraining). Boost provides a unique combination of workout guidance, exercise tracking, biofeedback, and games to help you get more out of your pelvic floor exercise and build consistent routines. |
Products for Bowel Dysfunction
These remain to be some of the foundational tools we will likely never stop recommending!
Squatty Potty
It is old news that American toilet seats are not optimal heights to allow the needed pelvic floor relaxation for stool evacuation. The squatty potty is a stool that fits around your toilet. When you prop your feet up on it the squatty potty puts your pelvic floor in the optimal position to do your business and limits the unwanted pushing and straining that some experience. EVERYONE SHOULD HAVE ONE! They also come in travel folding ones as well as fancy bamboo too!
Natural Calm
To go with your squatty potty, if you’re one that tends to have a harder time going to the bathroom or harder stools, this is a great, natural remedy you can use at night. Magnesium is a micronutrient that honestly, many people are lacking in their diet. It is used to relax smooth muscles (like your anal sphincter), helps you sleep, and also helps regulate your bowels. The type of magnesium in this is magnesium citrate.
Finding you need to splint to help eliminate? There are now two products on the market to help you with this (and not strain your shoulder to reach).
Femmeze Vaginal Trainer
This product was designed for individuals that suffer from prolapse, specifically a rectocele (where the rectum protrudes into the back wall of the vagina), and causes difficulty with evacuating stool, requiring them to use their fingers to help evacuate stool. This device inserts in and puts pressure to help realign the anatomy to make pooping much easier!
Releve
This device is similar to the Femmeze; however, it has some key upgrades and differences. For those that need a little more help, the Releve offers an inflatable piece that you can pump up after insertion into the vagina if you need a little more (or less) pressure and doesn’t require you to manually press into the tissue to realign the anatomy. After successful evacuation you can deflate and pull it right out!
The products listed next can be used for general pelvic health throughout and/or after your treatment and are more focused on pain relief!
These tools are some of our favorites here at PHRC and they may become a life-long companion or may offer short-term relief to make your healing journey more comfortable.
Theraseat
This foam cushion is meant for those that suffer with pain while sitting down. They offer a variety of options for cut outs, as well as a DIY cutout for those that can’t quite find the exact right fit. They can be used in the car, at home, work, or restaurants and have a nice handle so it’s easy to carry around!
IntelliRoll
This is by far our favorite foam roller – yes, there is actually a difference! This roller meets all the requirements, the dense foam which is important, the grooves improve the comfort around the spine and contours the body. Interested in learning more about foam rolling? You can check out our previous blog here.
The Stick Roller –
A good follow-up to the product above. The stick roller is handheld and is a little better when needing to get to some awkward body parts, like your inner thigh at the very top of your leg! Sometimes we have to get in weird positions to get those spots on the foam roller so this makes it a little easier, it also allows you to control the pressure a bit more for those extra sensitive spots.
Check out our videos about using the Stick Roller below:
Cupping Sets
Last but not least, cupping sets. At home cupping is one way you can independently perform myofascial release and mimic to some degree what we are doing with you in the clinic! There are different sets available, we love both! Check out our video here to understand the differences between the various types.
If you have ever been a patient here at PHRC or visited our office, you may recognize these products because we really do use them all the time! If you have feedback about these products we’d also love to hear so feel free to comment below and share some of your favorites!
______________________________________________________________________________________________________________________________________
Did you hear? We recently launched our new e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Chances are you or someone you know is dealing with vulvar pain and urogenital concerns. This book serves as a comprehensive guide to navigating these issues. Urogenital pain is prevalent in people with vulvas, and there are solutions.
Despite extensive research and endorsement from top medical experts and leadership societies, not everyone is aware of the benefits of the strategic combo of medical management & pelvic floor PT. We’ve developed this e-book to provide reliable information, practical tips, and solutions for those struggling with urogenital pain.
By combining physical and occupational therapy and medical treatment, you can overcome these challenges and regain control over your pelvic health. Look no further for the your pelvic health information! We’re here to help with your pelvic pain.
Our goal is to lead you towards a reasonable path to feel yourself again. We are here to help people find their individual solutions and to provide hope that full recoveries are possible and this book will tell you how!
Snag a copy for $10USD via our website.
______________________________________________________________________________________________________________________________________
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Amanda Stuart, PT, DPT, PHRC West Los Angeles
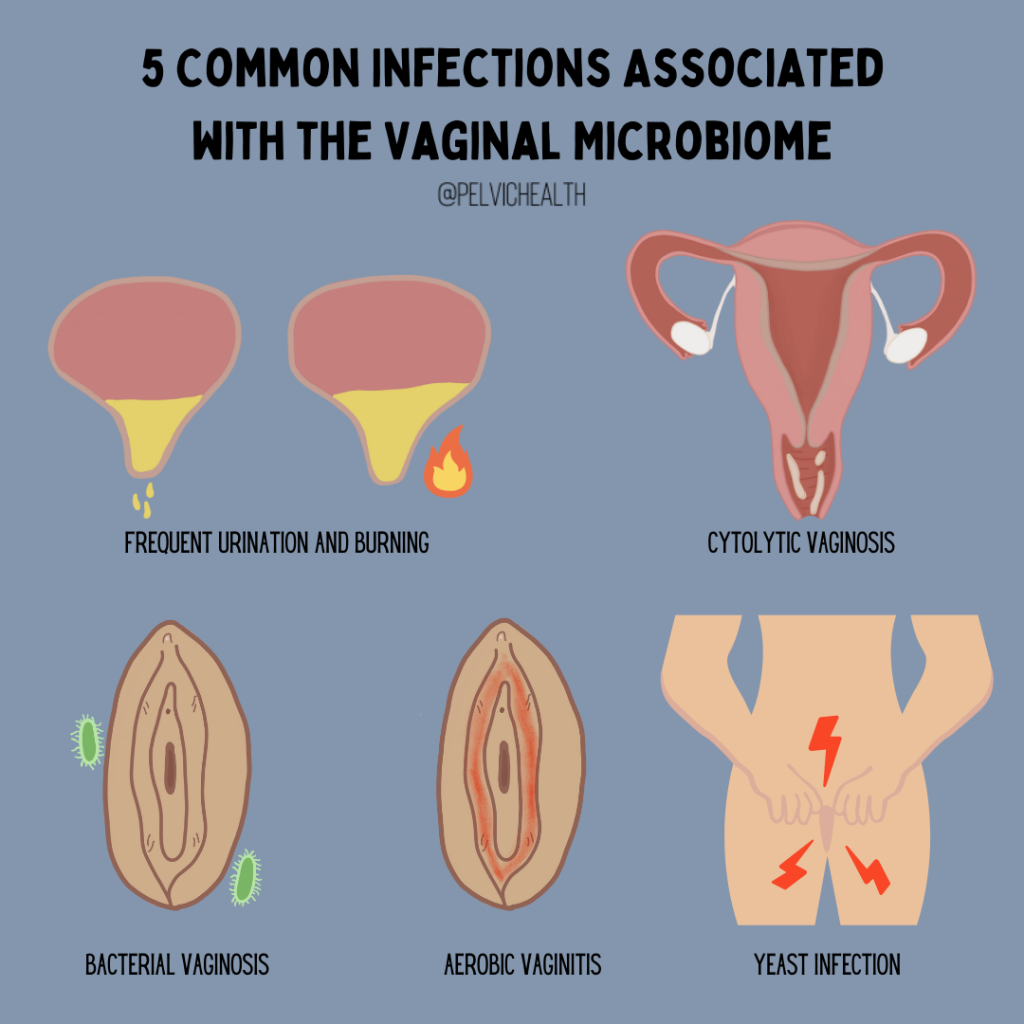
The vagina, like the gut, hosts its own ecosystem of microorganisms, known as the Vaginal Microbiome (VMB). When there’s a disruption in this ecosystem (dysbiosis), it can lead to various infections affecting genital and reproductive health. These infections may include bacterial vaginosis (BV), aerobic vaginitis (AV), cytolytic vaginosis, vulvovaginal candidiasis (yeast infections), and sexually transmitted infections (STIs). In this week’s blog, we will discuss how imbalances in the microbiome play a role in these conditions and the latest evidence.
Recently, the human microbiome has been the focus of several areas of research, while it is in its infancy, we are starting to learn more about the role these invisible organisms have on our health. Before diving into changes, we need to understand what a ‘healthy’ environment looks like.
Oftentimes people initially associate the word “microbiome,” with gut health or maybe even the skin’s ecosystem. In this instance, the vaginal microbiome is just as important to overall well-being and deserves equal acknowledgment. This complex community of microorganisms plays a crucial role in maintaining vaginal health, preventing infections, and supporting reproductive and sexual health.
Composition of a Healthy VMB:
- Dominated by lactobacillus bacteria, which produce lactic acid and bacteriocins, this maintains a healthy acidic pH which reduces risk of these conditions.
- Studies show that lactobacilli and the resulting acidic pH of the vagina promote a healthy epithelial barrier, inhibiting the colonization of harmful microbes.
Host Factors affecting the VMB:
- Genetic factors, including racial background, can influence the composition of the VMB.
- Different Lactobacillus species, like L. crispatus and L. iners, have varying effects on the VMB and susceptibility to infections.
- L. crispatus is associated with lower risks of infections like bacterial vaginosis and vulvovaginal candidiasis, while L. iners may coexist with bacteria linked to dysbiosis.
Bacterial Vaginosis (BV):
- BV involves the displacement of Lactobacilli by anaerobic bacteria like Gardnerella vaginalis.
- BV-associated bacteria produce biofilms that disrupt the vaginal mucosal and epithelial barriers, increase the vaginal PH and produce enzymes that enhance their ability to colonize.
- Treatment with Metronidazole is initially successful but recurrence is common at a rate of 50% within as little as 12 weeks to 12 months.
- Introducing L. Crispatus following Metronidazole treatment has been shown to decrease recurrence by 15% at week 12.
Vulvovaginal Candidiasis (Yeast):
- Vulvovaginal Candidiasis often occurs when the vaginal environment is altered by antibiotic treatment, hormonal changes, metabolic disease, immunological incompetence, sexual activity or other conditions that permit yeast, mainly Candida species (spp.), to colonize the female reproductive tract.
- L. Crispatus dominance is associated with lower risks of Candida colonization.
- Treatment involves antifungal medication such as Fluconazole, Nystatin, etc.
Aerobic Vaginitis:
- Aerobic Vaginitis is typically associated with purulent discharge, vaginal itching, dyspareunia and an inflamed vaginal wall.
- Similar to BV, this condition presents with a reduction of vaginal Lactobacilli.
- The bacteria most frequently encountered in aerobic vaginitis include group B streptococcus (GBS), E. coli and Staphylococcus aureus.
- A combination of antibiotics and probiotics are commonly used for treatment.
Closing Thoughts:
Now that I’ve discussed certain characteristics of both a healthy and unhealthy vaginal microbiome, let’s conclude with talking about how to address the dysbiosis that can occur:
- Low-dose transvaginal topical estrogen has shown to be effective at engendering a more optimal Lactobacillus-rich microbiome while not increasing the risk of estrogen-sensitive cancers.
- Probiotics, combined with antibiotics or antifungals and estrogen therapy, may improve the vaginal microbiome balance and vaginal health.
- It is important to note that Cytolytic Vaginosis would be the exception in that probiotics would not be warranted as this is caused by an overgrowth of Lactobacilli.
- Other treatments like Statins and vitamin D may also be beneficial.
- Vaginal Microbiome transplants from healthy donors have shown promise in treating recurrent BV but come with risks and challenges.
Composition of the Vaginal Microbiome in Vaginitis
Condition Vaginal Microbiome Features
Cytolytic vaginosis |
Overgrowth of Lactobacillus spp. |
Bacterial vaginosis |
Enrichment of Atopobium vaginae, BVAB1, BVAB2, BVAB3, Gardnerella vaginalis, Mobiluncus spp., Mycoplasma spp., Porphyromonas spp., Prevotella spp., Sneathia spp., and Ureaplasma spp.; depletion of Lactobacillus spp. |
Vulvovaginal candidiasis |
Normal to BV-like vaginal microbiome; colonization by Candida albicans, Candida glabrata, Candida parapsilosis, Candida tropicalis, or Candida krusei. |
Trichomoniasis (STI) |
BV-like vaginal microbiome; invasion by Trichomonas vaginalis |
Aerobic vaginitis or desquamative inflammatory vaginitis |
Depletion of Lactobacillus spp.; frequent detection of aerobic, enteric bacteria, e.g., E. coli, Enterococcus spp., Staphylococcus spp., and Streptococcus spp. aBVAB1, “Candidatus Lachnocurva vaginae”; BVAB2, Lachnospiraceae BV-associated bacterium 2; BVAB3, Mageeibacillus indolicus. |
Understanding the intricacies of the microbiome extends beyond just gut health—it’s a holistic view of the human body’s interconnected systems, including those critical to pelvic health. The vaginal microbiome, for instance, plays a pivotal role in preventing infections and maintaining overall reproductive wellness. Incorporating prebiotic foods into your diet can support these beneficial microorganisms, fostering a balanced and healthy microbiome throughout the body. By raising awareness and promoting education on this topic, we can empower individuals to make informed decisions about their health and recognize the importance of a balanced vaginal microbiome. Understanding this often-overlooked aspect of health is essential for holistic wellness.
_____________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!