Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
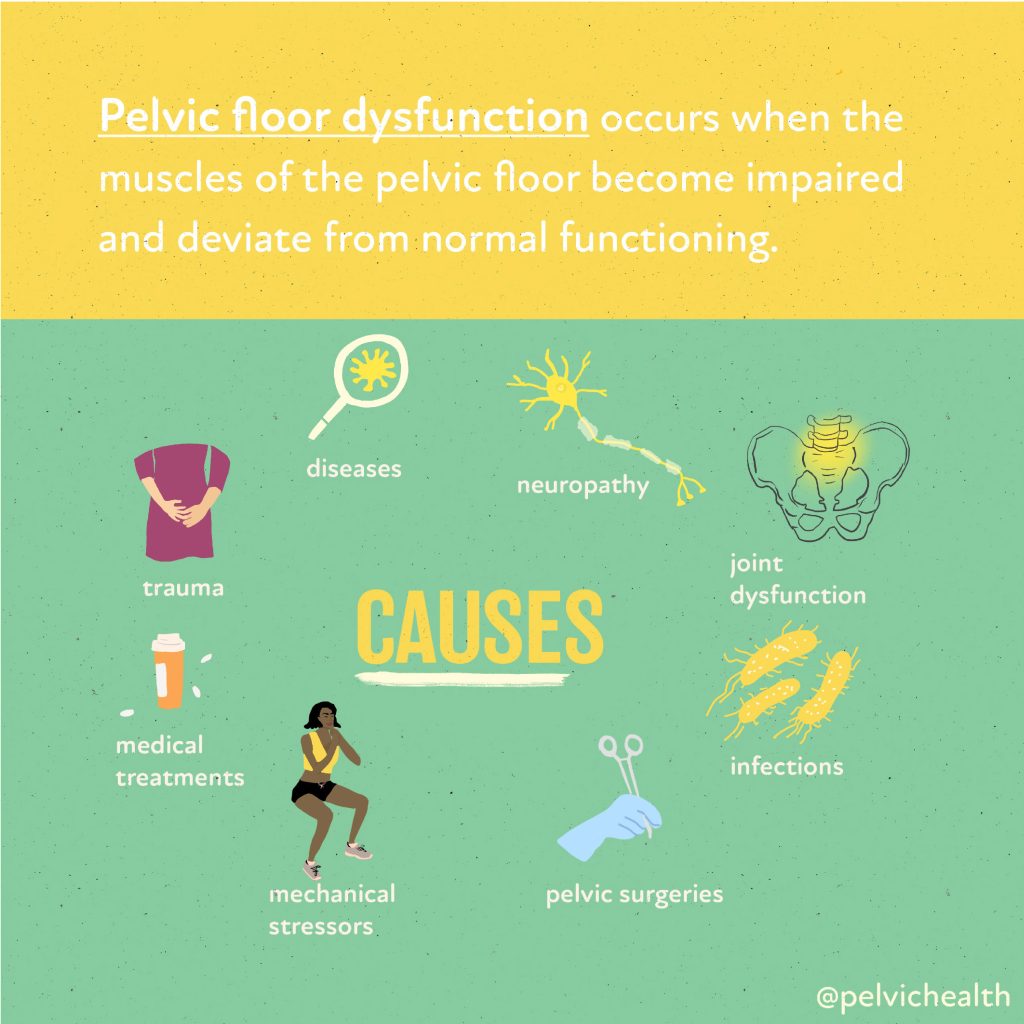
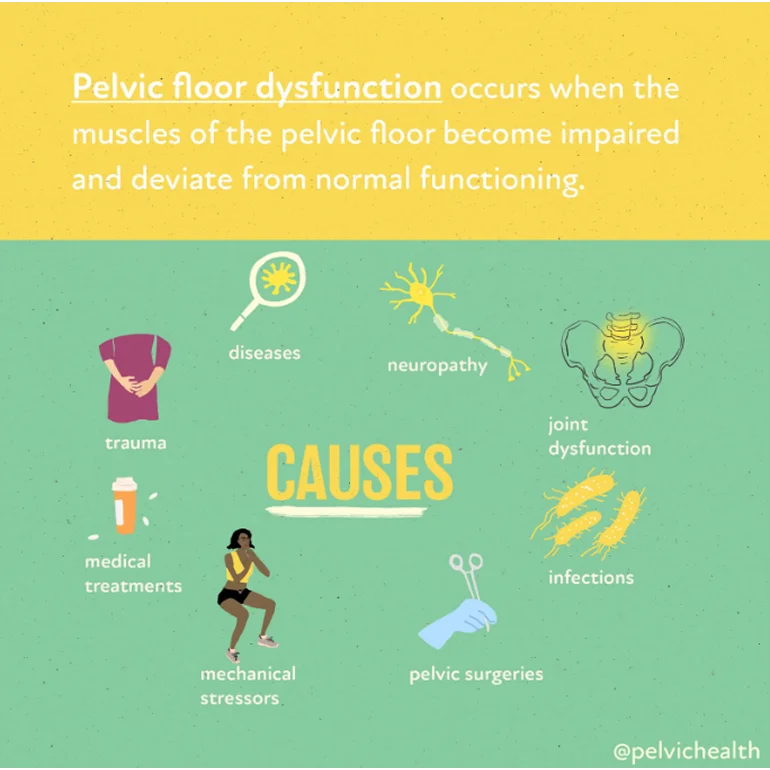
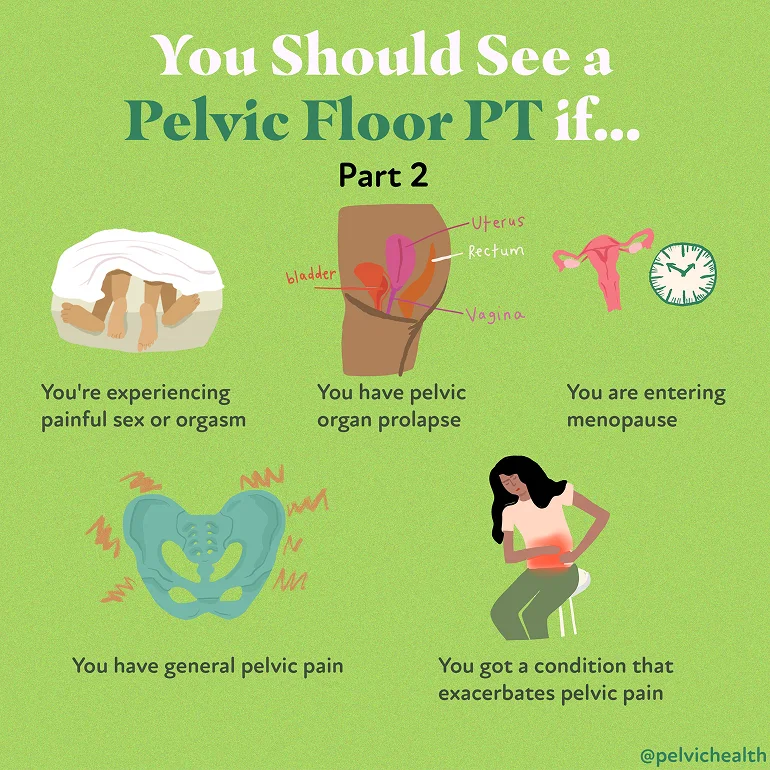
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
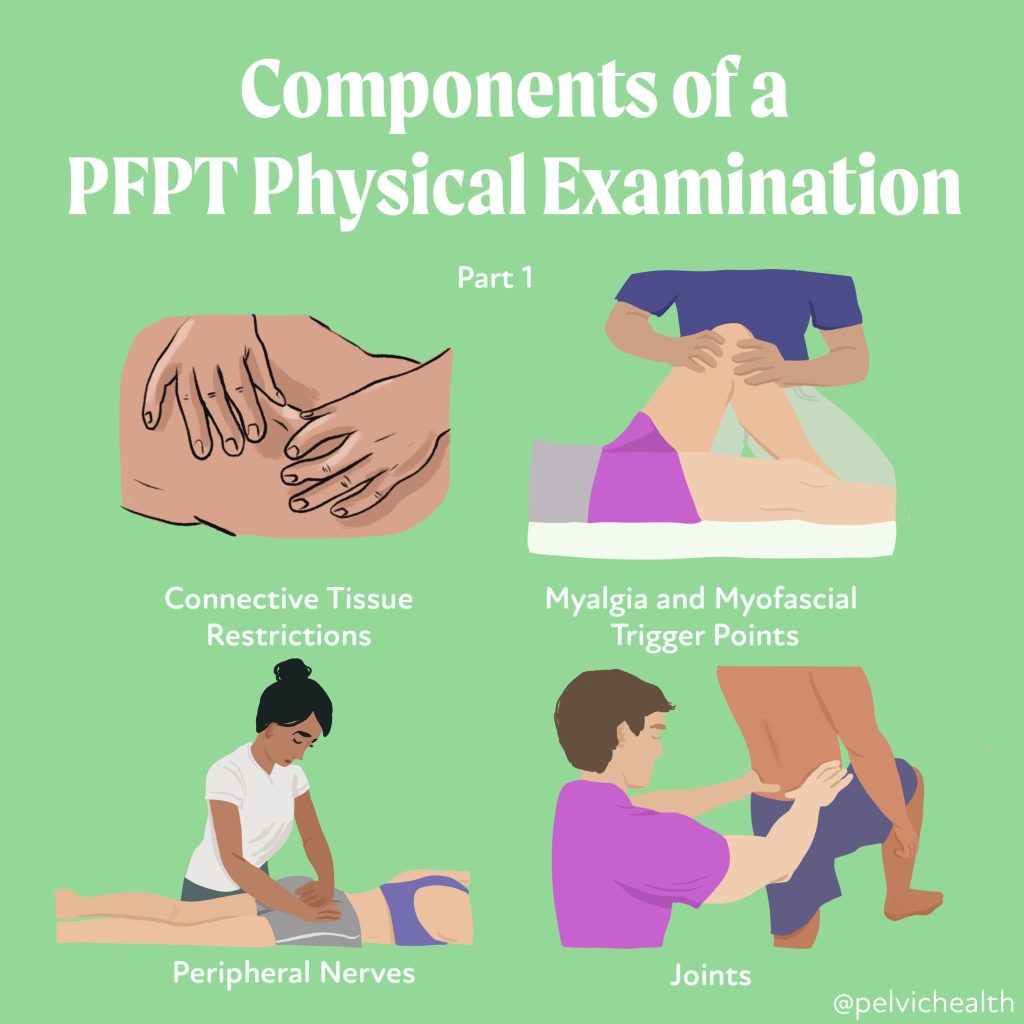
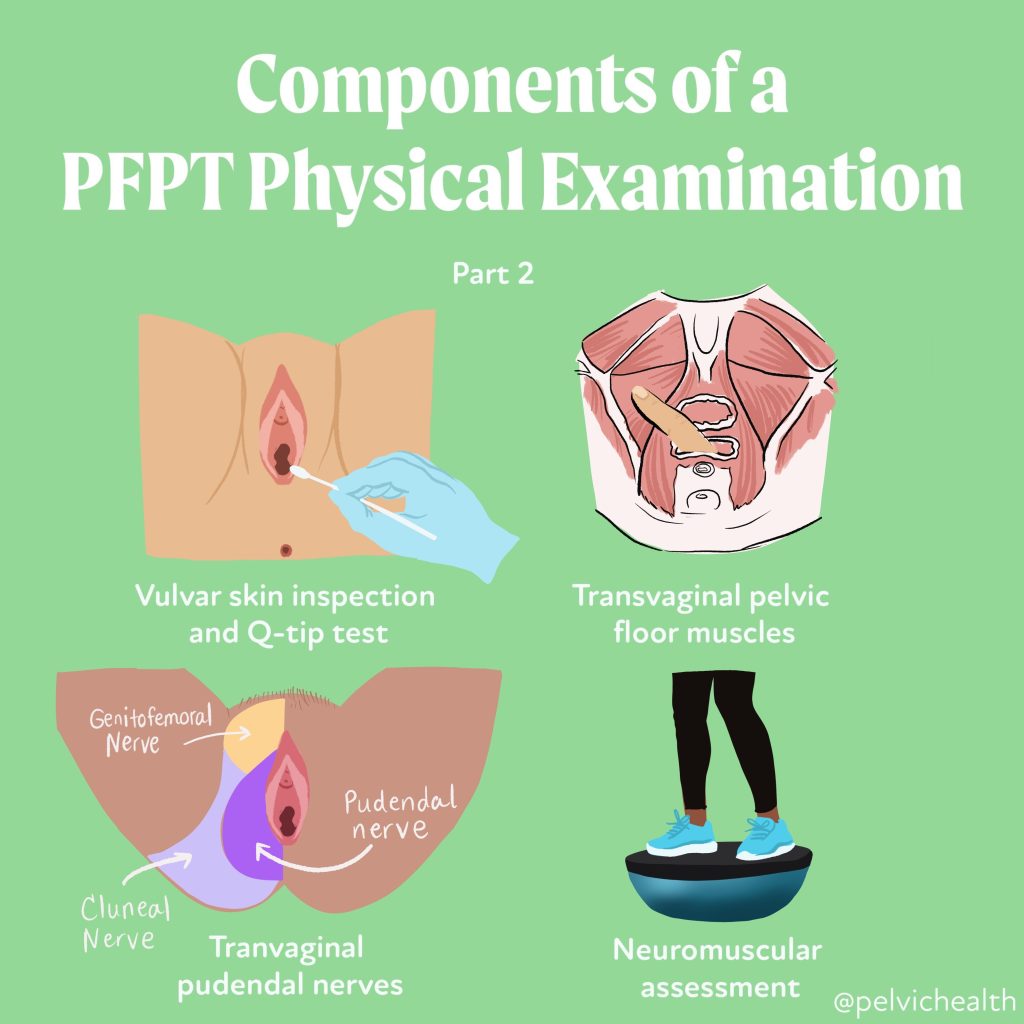
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Stephanie Prendergast, MPT, PHRC Pasadena
Have you ever felt an uncontrollable urge to move your legs when you’re trying to relax or fall asleep? If so, you may have experienced symptoms of Restless Legs Syndrome (RLS). This neurological condition affects millions of people, often disrupting sleep, causing distress, and sometimes connecting with other health issues, including pelvic floor dysfunction.
Understanding the Basics
Restless Legs Syndrome is a sensorimotor disorder, meaning it involves both the nervous system and movement. People with RLS describe sensations deep within their legs, sometimes in the calves, thighs, or feet; that create an irresistible need to move. These sensations are often described as:
- Tingling, crawling, itching, or “electric” feelings
- Deep ache or pressure inside the legs
- Restlessness that’s worse during periods of inactivity (sitting, lying down, or in the evening)
- Relief only when moving—walking, stretching, or massaging the legs
The hallmark feature is that symptoms are worse at night and improve with movement. This cycle often leads to difficulty falling asleep or staying asleep, contributing to fatigue, irritability, and reduced quality of life.
Who Gets Restless Legs Syndrome?
RLS can affect anyone, but certain factors increase risk:
- Genetics: Up to half of cases run in families.
- Sex: Women are affected nearly twice as often as men.
- Age: Symptoms often worsen with age, though they can appear at any time.
- Pregnancy: Many pregnant women experience temporary RLS, especially in the third trimester.
- Medical conditions: Iron deficiency, diabetes, peripheral neuropathy, kidney disease, and certain neurological disorders are associated with higher rates of RLS.
- Medications: Some antidepressants, antihistamines, and dopamine antagonists can worsen symptoms.
- Lifestyle factors: Caffeine, nicotine, and alcohol may intensify restlessness.
Why Does It Happen?
Although the exact cause is still being researched, studies point toward dopamine dysregulation and iron metabolism in the brain. Dopamine is a neurotransmitter that helps control movement; low dopamine levels in specific brain regions may trigger the uncomfortable sensations and motor restlessness typical of RLS.
Iron plays a role because it’s essential for dopamine synthesis. Even if blood tests show “normal” iron, the brain may not have enough iron stores for proper signaling. This is why iron supplementation (guided by a physician) can be an effective part of treatment for some individuals.
Other mechanisms under investigation include neuroinflammation, peripheral nerve hypersensitivity, vascular dysfunction, and autonomic nervous system dysregulation — all of which are also relevant in chronic pain and pelvic floor dysfunction.
Restless Legs Syndrome and Sleep
Sleep disturbance is one of the most common and frustrating consequences of RLS. People often toss and turn, unable to get comfortable. Many also experience periodic limb movements during sleep (PLMS) — involuntary leg jerks or twitches that occur repeatedly and disrupt rest. Over time, this can lead to chronic sleep deprivation, mood changes, and decreased concentration.
Improving sleep hygiene—consistent bedtime, stretching before bed, reducing screen time, avoiding caffeine late in the day—can reduce symptoms and improve rest.
Possible Connection to Pelvic Floor Dysfunction
While RLS primarily affects the legs, research and clinical observations suggest possible overlap with pelvic symptoms. Conditions like overactive bladder, pelvic pain, and restless genital syndrome have been found in some patients with RLS. These links point to shared neurological and sensory pathways that influence both the legs and the pelvic region.
For example:
- The spinal and peripheral nerves that regulate leg movement also communicate with pelvic floor and bladder control centers.
- Autonomic dysregulation (how the nervous system balances “fight or flight” vs “rest and digest”) can affect both sleep and pelvic muscle tone.
- Some patients describe “restlessness” or deep discomfort not only in their legs but also in the pelvic or genital region—a condition termed restless genital syndrome (RGS), thought to be a variant of RLS.
At PHRC, we see patients whose pelvic pain, urgency, or genital discomfort are intertwined with broader nervous system hypersensitivity or RLS-like features. Recognizing this overlap allows for more comprehensive, whole-body management that includes both the pelvic floor and nervous system regulation.
Diagnosis
Diagnosis is made clinically based on a patient’s history and symptom pattern. There’s no definitive blood test or imaging scan, but your clinician may check:
- Iron studies (especially ferritin levels)
- Kidney function
- Nerve health (if neuropathy is suspected)
- Sleep quality or periodic limb movements
A thorough history is essential, especially to rule out other conditions that can mimic RLS (such as leg cramps, arthritis, or neuropathy).
Treatment Options
Treatment depends on symptom severity, frequency, and underlying causes.
Lifestyle and behavioral changes:
- Regular moderate exercise and stretching
- Good sleep hygiene
- Reducing caffeine, nicotine, and alcohol
- Massage, warm baths, or heat before bed
Medical therapies:
- Iron supplementation (if ferritin <75 µg/L)
- Dopamine agonists (e.g., pramipexole, ropinirole)
- Alpha-2-delta ligands (e.g., gabapentin, pregabalin)
- In refractory cases, other medications under medical supervision
Integrative approaches:
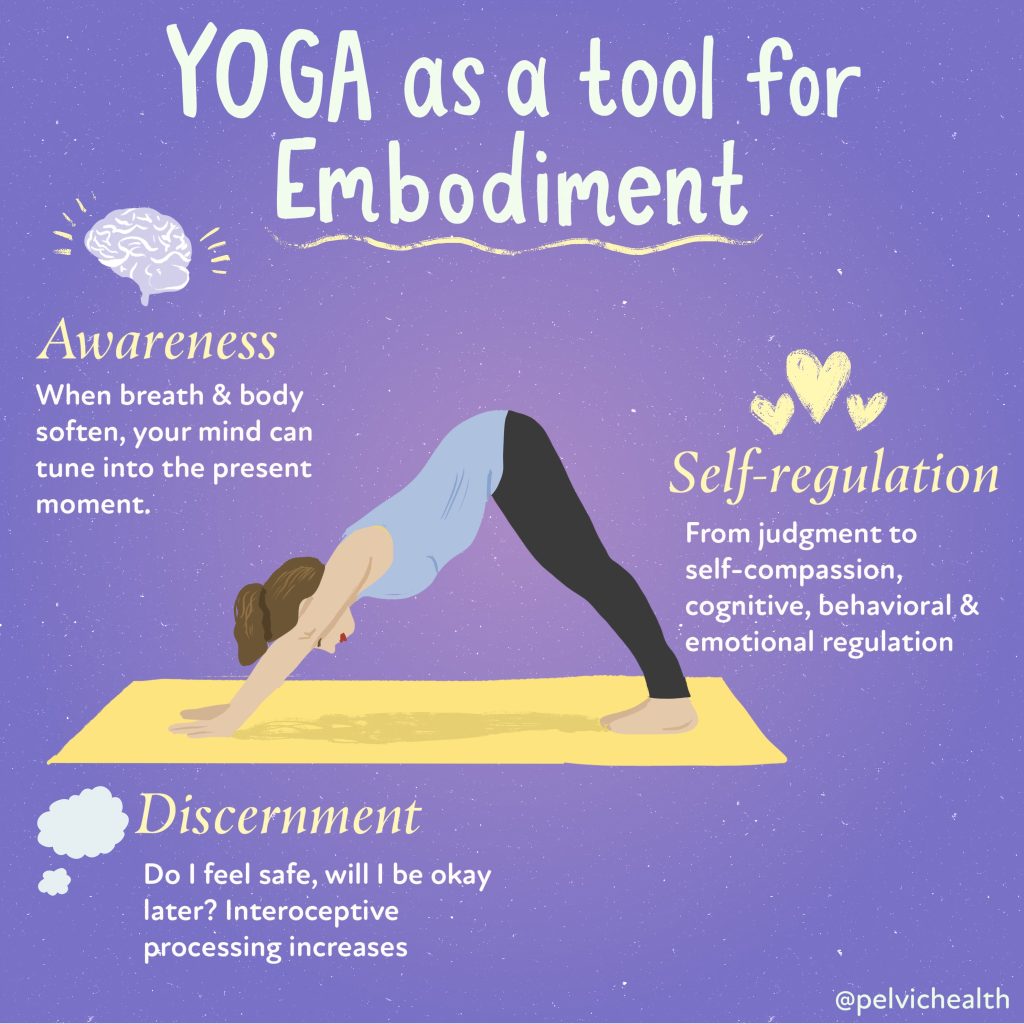
- Yoga, mindfulness, and breathing exercises to regulate the nervous system
- Physical and Occupational therapy to address lower-limb tension, circulation, and body alignment
- For those with overlapping pelvic floor dysfunction, targeted pelvic rehabilitation may improve muscle balance and relieve secondary discomfort
Living Well with Restless Legs Syndrome
Restless Legs Syndrome is real, and for many, it’s disruptive—but it’s also manageable. Understanding the triggers, treating underlying causes like iron deficiency, and supporting your nervous system through movement, stress management, and healthy sleep routines can dramatically improve symptoms.
If you or someone you know experiences RLS-like sensations, discuss it with your healthcare provider. Identifying it early helps avoid unnecessary distress and opens the door to effective, personalized treatment.
At PHRC, we believe the body’s systems are deeply interconnected—what affects your legs, nerves, and sleep can influence your pelvic health, and vice versa. Recognizing those links helps us treat the whole person, not just isolated symptoms.
Stay tuned to the blog, next week we will do a deeper dive into the connections between restless Leg Syndrome and pelvic floor disorders.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
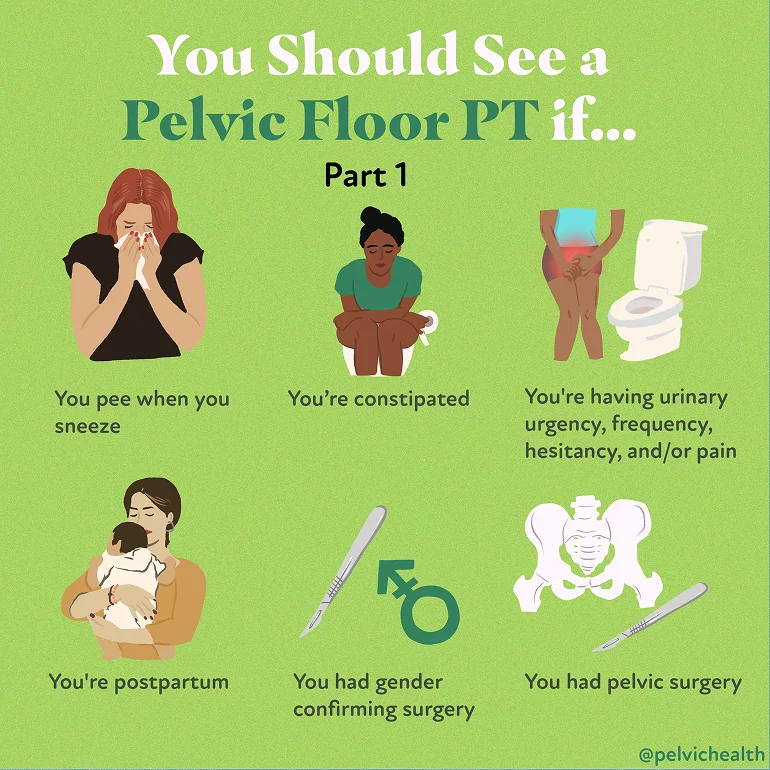
Pelvic floor physical and occupational therapy is one of the most effective yet underutilized approaches for treating pelvic health conditions. Many people who could benefit from therapy hesitate to start, often because they don’t know what to expect or feel unsure about what pelvic health rehab really entails. At the Pelvic Health & Rehabilitation Center (PHRC), our mission is to educate, empower, and provide compassionate care so patients feel confident taking the next step.
On our YouTube channel, we’ve created a library of educational videos that answer the most common questions about pelvic floor therapy. On our Instagram, we have an infographic library of educational images/graphics/carousels designed to breakdown everything you need to know about pelvic health. Throughout all our spaces, we aim to spread the knowledge of pelvic health, making it accessible to all. Below, we summarize five of our most popular and useful topics to help you understand what pelvic floor therapy is, what happens during an evaluation, and why it might be the right choice for you.
1. What to Expect With Pelvic Floor Physical Therapy
For many, the idea of pelvic floor therapy feels intimidating at first. This video walks through what typically happens when you come in for your first visit.
You’ll start with a conversation, not an exam. Our therapists ask about your medical history, current symptoms, and personal goals. This is your chance to tell your story and help us understand what matters most to you. From there, we’ll explain the evaluation process and answer any questions before moving forward.
The goal of this video is reassurance: pelvic floor therapy is professional, respectful, and patient-centered. Our team explains every step so you feel comfortable and in control.
2. Pelvic Floor Therapy: What Is It and How Can It Help Me?
This video introduces the basics of pelvic floor therapy in plain language. The pelvic floor is a group of muscles that support your bladder, bowel, and reproductive organs. When these muscles are too tight, weak, or uncoordinated, people may experience pain, urinary or bowel dysfunction, or sexual difficulties.
Pelvic floor therapy targets these issues directly. Through a combination of manual therapy, guided exercises, relaxation strategies, and education, patients can regain strength, reduce pain, and restore normal function.
This video emphasizes that pelvic floor therapy is not just for women—it benefits men and people of all genders across the lifespan. Whether you’re recovering after childbirth, managing endometriosis, coping with painful bladder syndrome, or experiencing chronic prostatitis, the Pelvic Health and Rehab Center can help.
3. What to Expect During Your First Pelvic Floor Therapy Visit
One of the most common barriers to treatment is the unknown: “What exactly happens when I show up?”
This blog breaks the process down step by step, What is a good pelvic PT session like. After the initial conversation, your therapist may assess posture, movement, and core muscle function. With your consent, they may also perform a gentle pelvic floor exam to evaluate muscle tone, strength, and coordination.
Nothing happens without your permission, and you’ll have the chance to ask questions along the way. The therapist will then explain findings and outline a personalized treatment plan, including frequency and expected duration of therapy. Make sure to read both parts, as we spend time breaking down the components of working with a pelvic floor therapist.
This transparency helps ease anxiety and shows that pelvic floor therapy is collaborative—you and your therapist work as a team.
4. Pelvic Floor Dysfunction Rehab: What You Should Know
In this blog, our cofounder highlights the signs, symptoms and treatment that comes along with pelvic floor dysfunction. This include:
- Stress Incontinence, which is the involuntary leaking of urine when coughing, laughing, sneezing, or during exercise, this is also common after pelvic surgeries, including prostatectomy
- Urge Incontinence, which is the involuntary urinary leaking when the urge strikes, such as putting the key in the front door to head to the bathroom
- Mixed Incontinence, which is a combination of both stress and urge incontinence
- Bladder pain, involves discomfort or pain in the bladder region, upon bladder filling or without bladder filling
- plus more
This blog is particularly helpful for people who are not sure whether PFPT applies to their situation. Many patients assume these problems are “just part of getting older” or “something to live with.” The message here is clear: pelvic floor dysfunction is common, but it is not normal—and there are effective treatments available.
5. The Role of Pelvic Floor Rehabilitation in Sexual Health
Sexual health is often overlooked in conversations about physical therapy, yet it is central to quality of life. In this video, we address how pelvic floor therapy can improve function and reduce pain for people experiencing conditions such as vaginismus, vulvodynia, erectile dysfunction, or painful intercourse after surgery or trauma.
By restoring healthy muscle activity and reducing nerve hypersensitivity, pelvic floor therapy supports both physical comfort and emotional well-being. Patients often describe feeling hopeful again after struggling for years with symptoms that impacted intimacy.
This video underscores that pelvic floor rehab is not only about treating pain or leakage—it’s also about restoring confidence, connection, and pleasure.
View this post on Instagram
Why These Resources Matter
Each of these sections has become a patient favorite because they speak directly to common fears and questions. Together, they provide a comprehensive picture:
- Clarity about what pelvic floor therapy is
- Reassurance about what to expect during a visit
- Education about the symptoms PFPT can treat
- Hope for those struggling with intimate or sensitive concerns
By watching and reading, patients gain a sense of familiarity before ever walking into the clinic. This makes the first appointment feel less daunting and sets the stage for successful outcomes.
Taking the Next Step
If you’ve been wondering whether pelvic floor therapy is right for you, we encourage you to explore our YouTube channel for more resources. These videos are just the beginning—our clinicians share insights on conditions ranging from interstitial cystitis to postpartum recovery, chronic prostatitis, and beyond.
At PHRC, we know that knowledge is power. The more patients understand their condition and treatment options, the better they can advocate for themselves and actively participate in recovery.
If you’d like to learn more or schedule an appointment at one of our 8 clinic locations across the U.S., please visit our website. Whether you’re in the SF Bay Area, the LA region, or New Hampshire or Massachusetts, our team is here to help you heal.
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual
physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
-
.
When Should I See a Pelvic Floor Physical and Occupational Therapists?
-
.
When it comes to pelvic floor physical and occupational therapy, cost is often one of the first things people ask about. However, the cost for an appointment is simply one piece of the bigger picture. While “in-network” Physical and Occupational Therapy might initially seem to have a lower cost, the type of care you receive and the frequency of which you can receive it, the expertise of the provider, and the overall time it takes to see results can be very different.
At the Pelvic Health and Rehabilitation Center (PHRC), pelvic health is our specialty. Our team consists entirely of licensed pelvic floor physical and occupational therapists with advanced training in pelvic floor therapy, and we are recognized leaders in this highly specialized field. From treating complex pelvic pain conditions to collaborating with top physicians across the country, our focus has always been on delivering the highest level of care and lasting results for our patients.
This guide will help you understand what sets PHRC apart, what’s included in the cost of care, how we compare to in-network clinics, and why so many people choose us for their pelvic health needs.
What is Pelvic Floor Physical and Occupational Therapy?
Pelvic floor physical and occupational therapy focuses on treating the muscles, tissues, and nerves in your pelvic region that support your bladder, bowel, and reproductive organs. These muscles also play an important role in controlling urination, bowel movements, and sexual function. When they become too tight, too weak, or uncoordinated, it can lead to pain, pressure, or difficulty with everyday functions.
Pelvic floor dysfunction affects people of all genders and identities. Tight muscles can cause sharp, burning, or aching sensations that might radiate to the hips, low back, or tailbone. Weak or uncoordinated muscles can create a feeling of heaviness, pulling, or even issues like leakage or constipation.
In pelvic floor physical and occupational therapy, your pelvic floor physical and occupational therapist will assess how your pelvic floor is working by examining muscle strength, coordination, and any areas of tension. Treatment often includes:
- Exercises to relax or strengthen the pelvic floor
- Manual therapy to release tight muscles or trigger points
- Guidance on improving movement patterns and posture
- A customized home program to support your progress
At PHRC, we customize therapy to your needs and coordinate with your other providers when necessary. The goal is to help you restore pelvic function, reduce pain or pressure, and regain confidence in how your body works—whether that’s in daily routines, exercise, or intimacy.
Do You Accept Insurance?
Yes, we accept various forms of a few insurances, depending on your location. We’ve outlined below how PHRC works with different insurance providers.
Brown and Toland Physicians
The Pelvic Health and Rehabilitation Center is part of the Brown and Toland Physicians network serving our patients in our Bay Area locations (San Francisco, Berkeley, Los Gatos, and Walnut Creek).
Kaiser Permanente (Northern and Southern California)
The Pelvic Health and Rehabilitation Center is an out-of-network, contracted provider with Kaiser Permanente of Northern California serving our patients in our Bay Area locations (San Francisco, Berkeley, Los Gatos, and Walnut Creek) and our Southern California locations (West LA and Pasadena).
Harvard Pilgrim Health Care
The Pelvic Health and Rehabilitation Center is now part of the Harvard Pilgrim Health Care network, serving our patients in our Merrimack, New Hampshire and Lexington, Massachusetts locations.
Medicare
The Pelvic Health and Rehabilitation Center (PHRC) is a non-participating Medicare provider. Non-participating providers accept Medicare but do not agree to take assignment in all cases. This means PHRC accepts Medicare insurance but does not consider Medicare’s approved amount as full payment for services.
As a non-participating provider, PHRC may charge up to 15% above Medicare’s approved amount for services (referred to as the “limiting charge”). This means patients are responsible for up to 35% of the Medicare-approved amount:
- 20% coinsurance
- 15% limiting charge
Patients are required to pay the full cost of their care upfront. However, PHRC will submit a bill to Medicare on the patient’s behalf. Once processed, Medicare will issue the patient a Medicare Summary Notice (MSN) and reimburse them for 80% of the Medicare-approved amount.
Our team is here to answer any questions you might have related to insurance coverage.
What You’re Really Paying For with PHRC
When you choose PHRC, you’re investing in more than just physical and occupational therapy sessions. You’re paying for:
- Specialized expertise from pelvic floor physical and occupational therapists who focus solely on pelvic health
- Extended one-on-one sessions with your dedicated pelvic floor physical and occupational therapist at every visit
- Comprehensive evaluations that go beyond quick, surface-level assessments
- Personalized treatment plans designed for your unique symptoms and goals
- Hands-on manual therapy to address muscle tension and trigger points directly
- A guided home program to help you stay on track between visits
- Collaborative care where we communicate with your other providers as needed
- In-person and virtual appointments available to make access to care seamless and easy
- Supportive, private environments where your comfort and progress come first
At PHRC, we combine focused expertise with a whole-person approach so you can achieve lasting results and regain control of your pelvic health.
Cost Comparison: PHRC vs In-Network Physical and Occupational Therapists
At first glance, in-network physical and occupational therapy appears less expensive because insurance often covers a larger portion of each visit. However, many patients discover that those savings come with trade-offs in the quality, time, and focus of care they receive.
In-network clinics often operate on volume. This means appointments are very short (typically only 20 to 30 minutes). This model leaves little time for hands-on treatment or meaningful conversation with your pelvic floor physical and occupational therapist—and often results in slower progress and more total visits.
PHRC takes a very different approach. Every visit is a full one-on-one session with a highly trained pelvic floor physical and occupational therapist. We dedicate time for a thorough assessment, hands-on manual therapy, exercise instruction, and plan adjustments. We listen carefully, tailor your care, and move at a pace that prioritizes real, lasting improvement. We have deep and close connections with medical professionals in our local areas and pride ourselves on ‘quarterbacking’ care for our patients so they no longer have to navigate care themselves.
What truly sets PHRC apart, though, is our depth of specialization. Every pelvic floor physical and occupational therapist at PHRC has residency-level training in pelvic floor therapy. This exclusive focus allows us to integrate pelvic floor and pelvic girdle physiology in a way that restores function across the entire body. We draw from a deep well of experience that only comes from treating complex pelvic health conditions day in and day out.
We also embrace an interdisciplinary approach. Many people with pelvic floor dysfunction benefit from collaborative care with gynecologists, urologists, gastroenterologists, orthopedists, psychologists, and others. We’ve built strong relationships with providers across the country so we can easily loop in trusted partners. Once your care team is in place, we act as the “CEO” of your treatment—coordinating care, leading communication, and making sure all providers are aligned and working toward your goals.
PHRC has also become a recognized leader in pelvic health education. Our team frequently speaks at hospitals, universities, and international medical conferences. Stephanie Prendergast, one of our founders, became the first physical therapist to serve as President of the International Pelvic Pain Society in 2013. We regularly teach community classes, mentor students, and write an award-winning blog, As the Pelvis Turns. In 2016, we published our first book, Pelvic Pain Explained.
Our commitment to staying at the forefront of pelvic health research, combined with the hands-on, individualized care we provide, is what makes PHRC different. While our services are often an out-of-pocket investment, our patients consistently tell us it’s worth it—for the results, the attention, and the expertise they couldn’t find anywhere else.
How To Know If PHRC is Right For You
If you’ve been struggling with pelvic health issues and haven’t found the answers or relief you need, you’re not alone. At PHRC, we specialize in treating a wide range of pelvic conditions with personalized, one-on-one care that meets you where you are. Whether your symptoms are new or you’ve been dealing with them for years, we’re here to help.
If you experience any of these symptoms or conditions, we can help:
- Pelvic pain
- Clitoral pain
- Male pelvic pain
- Hard flaccid
- Sexual dysfunction
- Bowel dysfunction
- Bladder dysfunction
We also provide specialized care for:
- Endometriosis
- Interstitial cystitis
- Pudendal neuralgia
- Pelvic organ prolapse
- Pregnancy and postpartum
- Menopause and perimenopause
- Post-surgical rehabilitation
- Pediatric pelvic health
- Transgender pelvic health
At PHRC, we create treatment plans tailored to your specific needs and goals, so you feel supported every step of the way.
How Long Does it Take To See Results?
The timeline for improvement varies because every person’s condition and goals are unique to them. Some patients begin to notice changes within just a few sessions, while others with more complex or long-standing symptoms need several months of consistent care to see meaningful progress.
At PHRC, we draw on our deep experience treating a wide range of pelvic floor conditions to create a plan that’s realistic and effective. Because our sessions are longer, highly focused, and one-on-one with a pelvic floor physical and occupational therapist, many patients experience faster results compared to shorter, generalized in-network visits.
We continually reassess your progress and adjust your treatment as needed. Our goal is not just temporary relief, but lasting improvements in your function, comfort, and quality of life.