Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
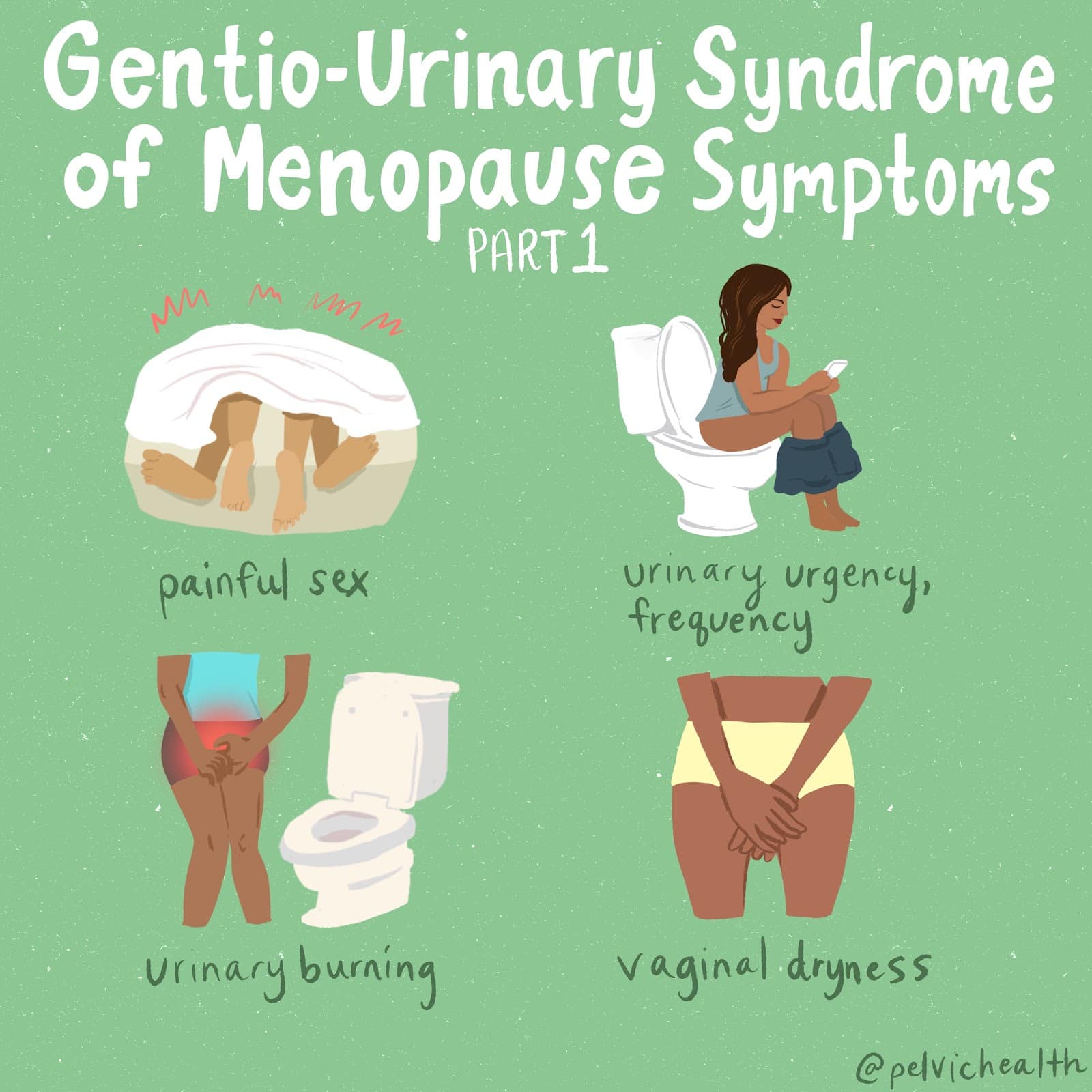
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
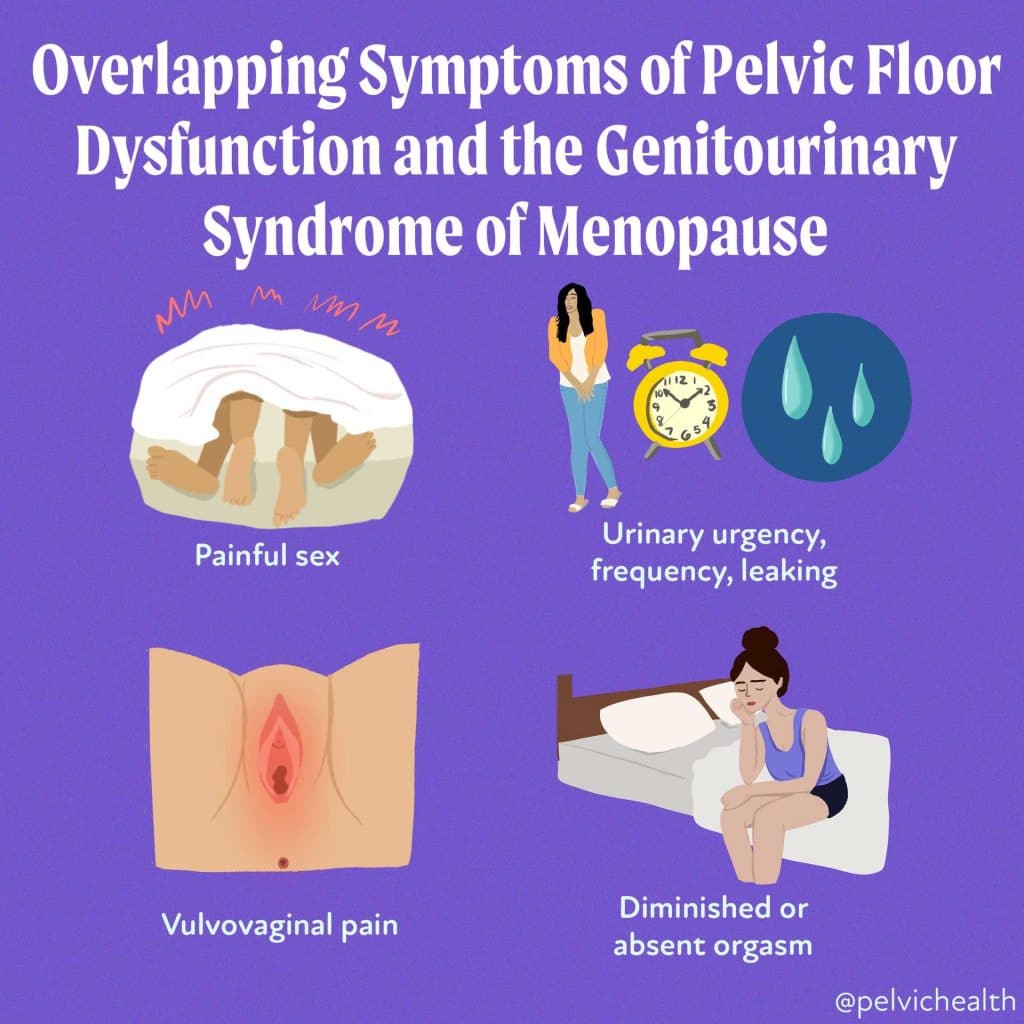
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting
An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.
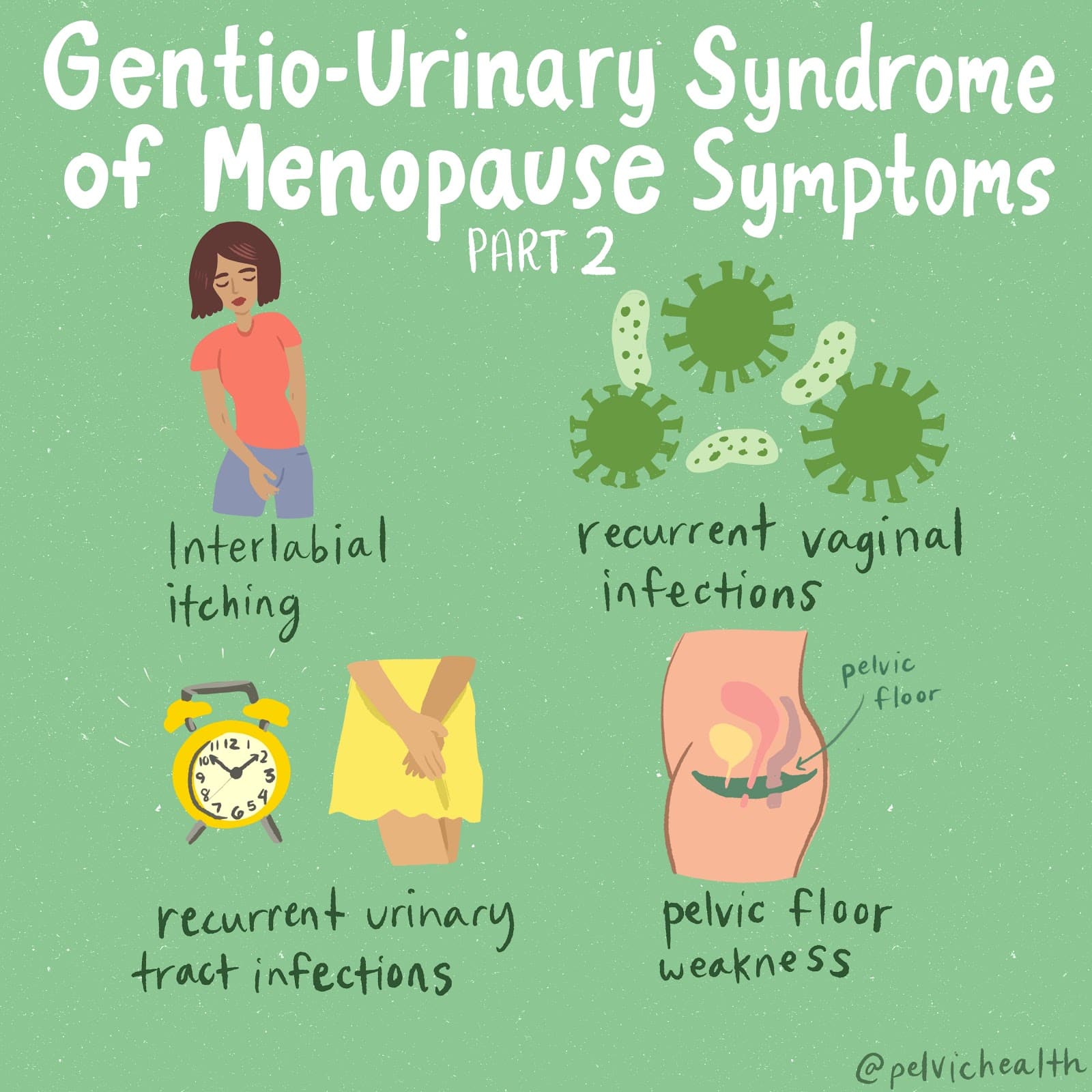
Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By admin
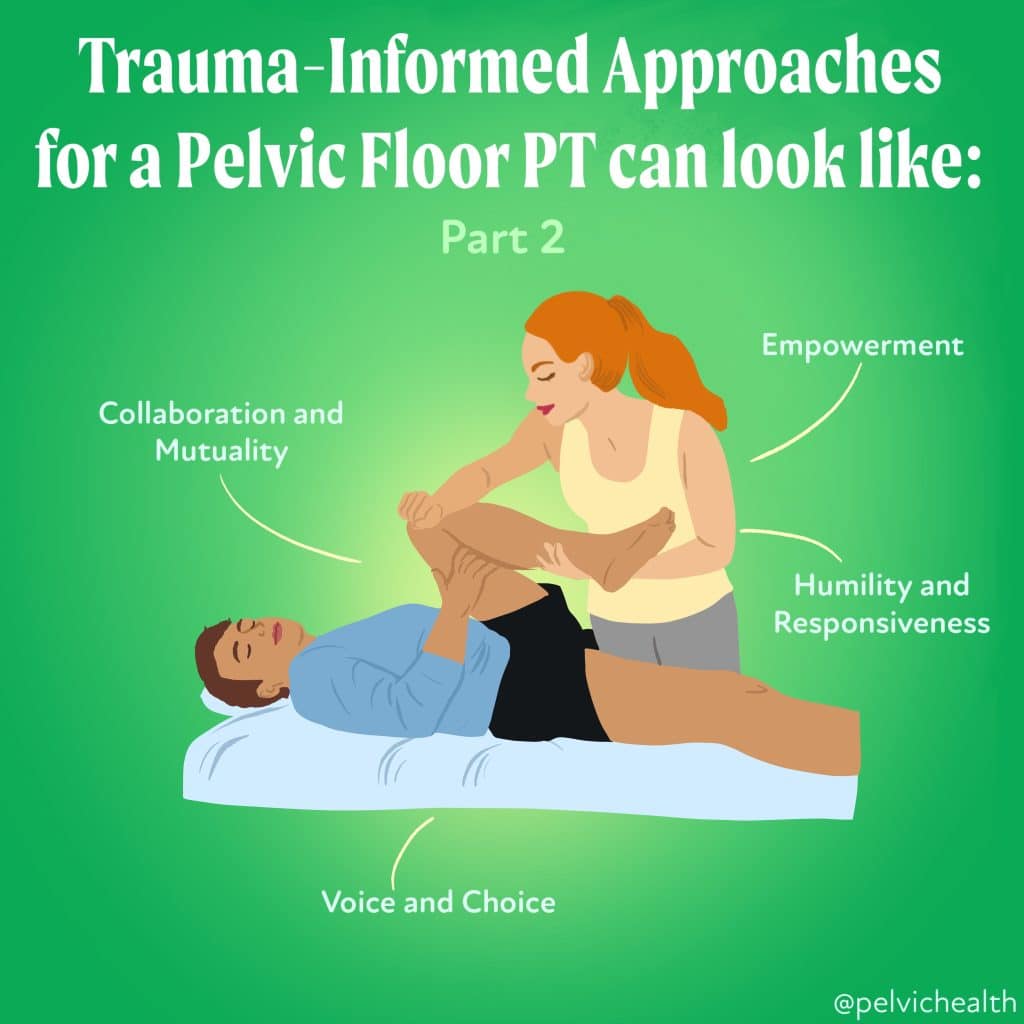
According to the Center for Health Care Strategies, “a trauma-informed approach to care acknowledges that health care organizations and care teams need to have a complete picture of a patient’s life situation — past and present — in order to provide effective health care services with a healing orientation.” In the image we have listed a few of the key principles of trauma informed care. Hopefully trauma-informed care just becomes known as the standard of care, and here are a few ways that a pelvic floor physical and occupational therapists can implement trauma-informed approaches.
- Asking for consent prior to any form of treatment.
- When doing a technique telling the patient what you are doing, why and where.
- Showing support by validating their feelings and experiences.
- Creating a safe environment for patients: this can look like not being in between patients and the door, allowing them to be closer to an exit.
Trauma-informed approaches for a pelvic floor physical and occupational therapists continued. The images above are the core principles of trauma informed care by SAMHSA and CHCS. Below are some examples of ways we can implement these principles in the clinic.
- Providing options for patients and the space to allow them to collaborate in their treatments.
- Doing regular check-ins with patients throughout the session to allow continued opportunities to voice out if they’d like to discontinue.
- Biases and stereotypes (e.g. based on race, ethnicity, sexual orientation) and historical trauma are recognized and addressed.
- Asking patients about their preferred name and pronouns that they would like to be addressed with.
These are all referenced from the center for health care strategies (CHCS), SAMHSA, and CDC.
The Key Principles include:
Safety:
All that are involved in the organization including the clients or patients feeling physiologically and psychologically safe (e.g. Allowing employees the ability to provide feedback on how safe they feel in their work environment). Some other examples provided by the Center for Health Care Strategies (CHCS) include:
-
- Keeping common areas well lit like bathrooms, entrances, and exits.
- Easy accessibility to doors to easily exit whether in a treatment room or in the facility.
- Welcoming patients with respect and support.
- Having staff that understands maintaining healthy boundaries and that can manage conflict.³
Trustworthiness and Transparency:
The company or organization is transparent with employees and clients with decisions and operations (e.g. Being transparent with your patient about objective findings and decisions on the treatment plan).
Peer Support:
Supporting those who are trauma survivors with “establishing safety and hope, building trust, enhancing collaboration, and utilizing their stories and lived experience to promote recovery and healing.” This can help with burn-out that is common in health care settings, as well as, prevent secondary trauma. The CHCS provides some examples on ways to help prevent secondary trauma:
-
- Allowing “mental health days.”
- Recommend your staff to engage in various types of self-care like physical activity, yoga or meditation (Check out Tips for Managing the Stress of COVID-19 and Your Pelvic Floor that shares some great examples).
- Supporting regular meetings with clinicians and supervisors to discuss and address feelings about patient interactions.
- Trainings on awareness about secondary trauma.³
Collaboration and Mutuality:
Showing the importance of partnering and assessing the power dynamic between all the levels of staff and between staff and clients, so that healing can be promoted when power and decision-making is shared. (e.g. Having your patient play an active role in their treatment plan. Asking for the patient’s input and allowing space for more dialogue versus the practitioner dictating the set plan).
Empowerment, Voice, and Choice:
The organization develops and services to “foster empowerment for staff and clients alike. Organizations understand the importance of power differentials and ways in which clients, historically, have been diminished in voice and choice and are often recipients of coercive treatment.” Some examples include:
-
- Allowing patients or employees to have a voice and choice.
- Prior to a specific treatment explaining what you will be doing and asking the patient or client if you can precede can be a way of allowing them to have a voice and choice.
- Employees having the ability to share their voice while still feeling safe to do so.
- Not pushing a survivor to disclose their trauma history and allowing it to be their choice.
Cultural, Historical, and Gender Issues:
Also adopted as humility and responsiveness by the CHCS. Active movement “past cultural stereotypes and biases (e.g. based on race, ethnicity, sexual orientation, age, religion, gender identity, etc.)…and recognizes and addresses historical trauma.” Implementing policies that would respond to any racial, ethnic, and cultural needs of staff and clients. (e.g. Asking an individual what their pronouns are and calling the individual by the selected pronouns without judgment or biases).²
This is just a brief explanation of SAMHSA’s trauma-informed approach with some adaptations and examples from the CHCS to help bring more awareness and to hopefully start the conversation around this topic. If you would like to dive further into their concepts and educational materials check out SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach and Video: What is Trauma-Informed Care?.³
Resources:
Treating the Whole Person: Trauma-Informed Care Part 1
Treating the Whole Person: Trauma-Informed Care Part 2
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
Did you know that your foot can affect your pelvic floor?
Foot and ankle positioning has an effect on the pelvic floor by influencing changes in muscle activation up the legs ultimately resulting in changes with pelvic tilt positioning. There are biomechanical changes from the ground up.
The connection in brain mapping of motor and sensation- the genitals and foot are mapped right next to each other.
There are also fascial connections from the foot to the spine.
Both the pelvic floor and feet are shock absorbers.
Assessing foot and ankle positioning and utilizing strategies to affect the pelvic floor can be helpful for some people looking to improve their pelvic floor muscle motor control. A pelvic floor therapist is a great person to help with this!
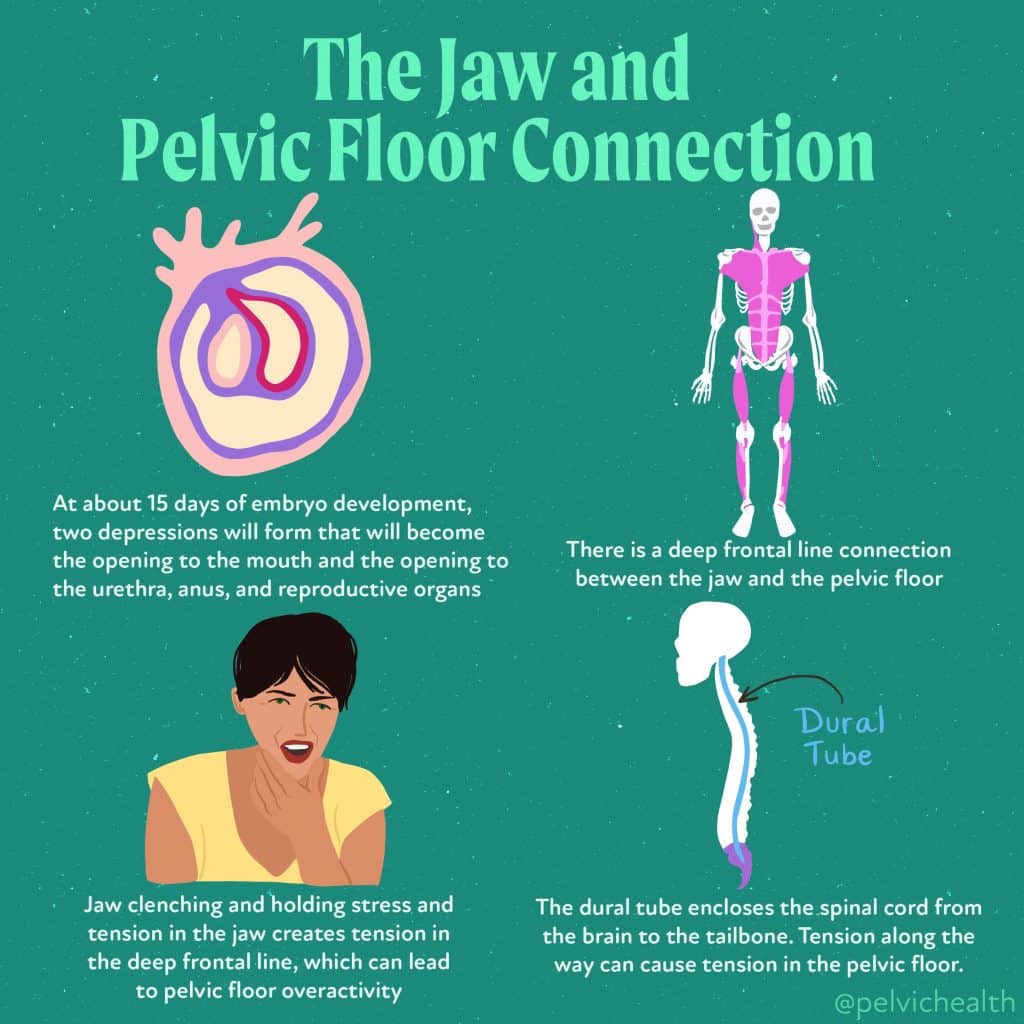
Did you know that the jaw and pelvic floor are connected?!
If you have jaw pain and/or pelvic pain they are closely linked. They’re connected through early development of the embryo, dural tubing surrounding the spinal cord, and through fascial connections. Let’s discuss:
Embryologic connection:
At about 15 days of embryo development will form two depressions that will become the opening to the mouth and then the opening to the urethra, anus, and reproductive organs as development of the spine occurs.
Fascia:
There is a deep frontal line connection between the jaw and pelvic floor.
Stress:
Jaw clenching and holding stress and tension in the jaw creates tension in the deep frontal line, which can lead to pelvic floor overactivity.
Dural Tubing:
The dural tube encloses the spinal cord from the brain to the tailbone. Tension along the way can cause tension in the pelvic floor.
Stress and daily holding patterns in the jaw can tension the fascial connection and create overactivity in the pelvic floor muscles. Now is your opportunity to check in and unclench your jaws!
Fischer MJ, Riedlinger MD, Gutenbrunner C, Bernatek M. Influence of the temporomandibular joint on range of motion of the hip joint in patients with complex regional pain syndrome. J Manipulative Physiol Ther. 2009; Jun;32(5):364-71. doi:10.1016/j.jmpt.2009.04.
Foster SN, Spitznagle TM, Tuttle LJ, et. al. Hip and Pelvic floor muscle strength in women with and without urgency and frequency predominant lower urinary tract symptoms. J Womens Health Phys Therap. 2021; 45(3): 126-134. doi:10.1097/jwh.
Garstka AA, Brzozka M, Bitenc-Jasiejko A, et. al. Cause-effect relationships between painful TMD and postural and functional changes in the musculoskeletal system: a preliminary report. Pain Res Manag. 2022: Feb 28;2022:1429932. doi: 10.1155/2022/1429932. eCollection 2022.
Van der Velde J, Laan E, Everaerd W. Vaginismus, a component of a general defensive reaction. An investigation of pelvic floor muscle activity during exposure to emotion-inducing film excerpts in women with and without vaginimus. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(5): 328-31. doi: 10.1007/s001920170035.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Jandra Mueller, DPT, MS, PHRC Encinitas
The recent study titled “Fusobacterium infection facilitates the development of endometriosis through the phenotypic transition of endometrial fibroblasts” by Muraoka et al. has generated significant attention and frenzy in the media.
The media coverage of this article has been intense, with headlines highlighting the potential breakthrough in understanding the pathogenesis of endometriosis, the role of bacterial infection, and how antibiotics may just provide us with the answer we’ve been searching for! If it were only that simple…
Numerous news outlets have covered the study’s results, emphasizing their own interpretation of the research findings and potential treatment approaches. However, it is worth noting that due to the article’s restricted access,* a considerable portion of the media coverage has led to misleading or incorrect interpretations of the actual research findings. Similar to the childhood game of telephone, the dissemination of this partially accurate information has resulted in its continuous circulation among numerous popular social media platforms.
*Restricted access: meaning that the research article in full-text is only available for purchase and is not available to the public for open access. In order to obtain a copy, you will have to pay money for access or you can always email the author and oftentimes, they will give you individual access.
While this study has proposed another potential factor for the development of endometriosis, it’s important to note that the findings of this study are preliminary, and further research is necessary to confirm and expand upon these results, which the authors clearly state in the publication as well as an interview that you can find online.
However, the media frenzy surrounding this article highlights the significance of addressing endometriosis, a condition that affects many individuals worldwide, and the potential impact of novel research findings on improving the understanding of this disease and potential treatment options that offer more than just hormonal suppression. To have more people talking about endometriosis is not a bad thing, but the viewpoints and what is often stated in news and media outlets may become problematic, especially when we are making conclusions and assumptions without all of the information.
As with any scientific study, it is crucial to approach the findings critically, consider the study’s limitations, and await further research and validation before drawing definitive conclusions. It is clear that the interpretation of this article has created a clear division among those that truly understand the complexity of this disease, and those that do not. These interpretations may seem very exciting to those who do not understand the complexity of this disease, but are “insulting and condescending to suffering patients and expert providers who have dedicated their life to studying the disease.“
On the other side are those that have prominent voices in this community and naturally, this media coverage likely did not sit well. It has been disappointing to see opinions voiced as fact, when in fact, many of the statements that were made also lacked understanding of the actual research, and just opposed the views of the news outlets. This may also pose risks and create barriers for future research endeavors in the field.
There were a number of claims from those of us in the community that were disappointing and unfair to say. We absolutely need to be critical when looking at new information, and we encourage everyone to do that. The beautiful thing about this population is that often, patients with endometriosis know so much more about their disease than many providers, because they have to. A few things that were consistently stated are important to highlight and break down.
The Problem:
News media outlets are often purposely framed to meet a certain narrative meant to report focusing on exciting and attention grabbing details of the study. These reporters are not medical providers and want to report on key findings and highlight what they feel will often create engagement, whether that is positive or negative, engagement is viewership.
The Washington Post was heavily criticized by some in the endo community for reporting on a “flawed study,” and they should be more rigorous about posting or publishing “careless information” because the “researches did not have the basics of endo correct and endo could only be stopped by removing organs.” While the WaPo article does make the claim that the only cure for endo is removing a person’s organs, the authors did not. Aside from this, these claims are far-reaching and overall, the WaPo coverage otherwise did a decent job in reporting what this study means: a starting point to look further very clearly, also reporting on the limitations of the clinical applicability of the findings. As far as the claims of “flawed” or “trash research” this is simply false. Below, we have laid out guidelines in assessing quality of the research, which this study meets at every point.
Aside from the WaPo coverage, other media outlets have reported on the study, some less accurately. Remember, these reports are often brief, and misrepresent the actual research findings, offering highlights of very complex topics which are compiled into summaries limited by a word count. This leads to frenzy and evokes emotion from those passionate about the disease, some of which have a loud public voice. This in turn can either fuel the fire to those that have been dismissed and gaslit causing reactive posts which also have their own limitations and are not being objective, though often well meaning.
What is most important is that you learn to be critical of information from third parties, and make your own opinion based on the actual data from the source. Of course, as non-medical providers, and even if you are in the field, this can be a daunting task. Relying on these outlets for true information is hard, especially if generally they are a trusted source, it is still important to approach these topics with a critical mind. Very extreme viewpoints almost never provide accurate facts and are loaded with personal bias.
A few reminders:
- Extreme viewpoints and statements are almost never accurate, there is usually another perspective to consider
- If you cannot engage with others on these topics and better understand their reasoning, there is a reason for that, be critical
- Ask questions, be open minded, if they do not provide a reasoning for their claims or an option to have a conversation and open discussion, this may be a big red flag.
Level of evidence vs. Quality of evidence – these terms are not synonymous
The next issue are the major claims that this research was extremely flawed and was low quality. Level of evidence and quality of evidence are two very different things to be aware of. You may have low level evidence that is high quality, and high level evidence that is low quality, the two are not synonymous.
The level of evidence refers to the hierarchy or classification of different types of studies based on design and potential for bias. For example: systematic reviews and meta-analysis are the top of the chain followed by randomized controlled trials, cohort studies, case reports, etc. The level of evidence helps to determine the strength of the conclusion and often-times how clinically useful it may be.
The quality of evidence refers to the overall methodological soundness and reliability of the study looking at several variables which determine how flawed or biased the study may be and what limitations it may have based on these factors. Both of these factors are important in utilizing the findings of the research.
This study was not a high level of evidence due to the nature of what was being studied, but was actually very high quality. Overall, we can utilize the findings for further research, but the findings are limited and not clinically applicable until higher level studies are performed. To give a more detailed breakdown of the quality of this study, to give more specific information on this statement.
What makes good research?
Quality of research: the level of evidence for this article is naturally low, because of the type of study they conducted. They used animal models, which is often done in preliminary research to prove your hypothesis before you can ethically study humans, especially if there is a treatment involved. Many types of studies start this way, to build a foundation for future research, not meant to be clinically relevant immediately. Low level evidence can still be good research. All that means is that there is a long way to go before being able to clinically apply the findings.
Study design: the methodologies and techniques to address the research question or hypothesis effectively.
- The authors did this very well, they did appropriate techniques and explained in great detail how and why they did what they did. This is called reproducibility, and is marked higher if the methods are well documented for others to replicate the work, which is important if there is meaning in the outcomes, so that others can validate these findings.
Sample size and selection: there should be a predetermined number set so that they ensure the results are statistically meaningful and representative of the target population.
- The authors in this study did not do a statistical analysis to find the sample size; however, they note in the study that the sample size was based on estimates from pilot experiments and previously published results. Ideally, they should do their own, but they had a method and they explained that, which is also important.
Control groups and comparisons: You need a group to make a comparison too, ideally with minimal variables to control the experiment and compare results to make sure findings were not just by chance, or for some other unknown factor.
- This study did have a control group in both their human tissue samples as well as their animal studies. That being said, one of the issues people had with this study is that they compared tissue samples from women undergoing hysterectomies that did not have endometriosis, but had other issues such as fibroids, cancer, and adenomyosis. The gold standard would of course be tissue samples from uteri that do not have any sort of disease, but that would just be unethical – ask women to undergo a hysterectomy for no reason just to study their tissues? In my opinion, this was a feasible option.
Data collection methods: Studies should use appropriate tools to collect data in a consistent and systematic manner.
- The researchers not only did this, but a significant amount of their research paper is discussing and describing these methods, this also plays into reproducibility. They are transparent every single step in their methods.
Data analysis: Proper statistical analysis should be used, certain statistics are necessary to run depending on the type of data you have.
- Since I am not a statistician, though as a healthcare provider we do take classes on how to do this, it is less important for what we are discussing. What is important is that the authors are transparent about the statistical analysis used, which means anyone interested can double check that they did the correct work. Despite transparency, researchers use the wrong analysis and this can contribute to a lower quality of study. In general, if they are being transparent and an error is found, it is less likely they intentionally ran the wrong analysis.
- Considering this article has strict guidelines on data and statistical analysis, it is fair to say that these standards were met, in-line with the above point that it is very easy for someone to verify their statistics.
Peer Review and Publication: prior to publication, studies often go through a rigorous peer-reviewed process, especially in reputable scientific journals. These studies generally have a higher level of quality. This process ensures that the study has undergone critical evaluation by experts in the field thus improving the overall validity and reliability of the findings.
- This publication was in the Science Translational Medicine journal, which has very strict guidelines in regards to all of the above areas mentioned which you can find in detail on their website. This study meets this guideline.
Ethical considerations: this includes obtaining informed consent from participants, maintaining participant confidentiality, and adhering to ethical guidelines. This protects the rights and well-being of study participants and contributes to the overall integrity of the study. This is true not only for human participants, but animals as well.
- The authors meet this criteria and describe their process for these experiments within the research study.
Furthermore, the authors fully disclose the limitations of their research in the research article itself, and in several of the interviews covering this topic. The ideal of bacteria playing a role in the development of endometriosis is not a new topic and there have been other studies investigating this. This offers information about a correlation, not a causation, of the origin of endometriosis. The bottom line and takeaway from this study is that they found a bacteria that caused a cascade of inflammatory responses and gene expression that grew endometriosis lesions in mice. Because there was significant differences in the human tissues in regards to this bacteria, along with other studies finding similar results in regards to other bacteria, future studies looking into why those with endometriosis are more susceptible to opportunistic pathogens and further studies exploring the role these pathogens play in regards to endometriosis is warranted based on the findings of this, and other studies on this topic.
Looking for more information about Endometriosis or wanting to stay up to date on the latest research? Head over to Instagram to follow our friends at iCareBetter, or their website which has an Endometriosis Specialist Directory! We encourage you to also subscribe to their podcast, iCareBetter: Endo Unplugged, with their host (our physical and occupational therapists) Jandra Mueller, DPT, MS!
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.