Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Emerging Perspectives on Chronic Pelvic Pain and Sexual Health
By Jandra Mueller, DPT, MS, PHRC Encinitas
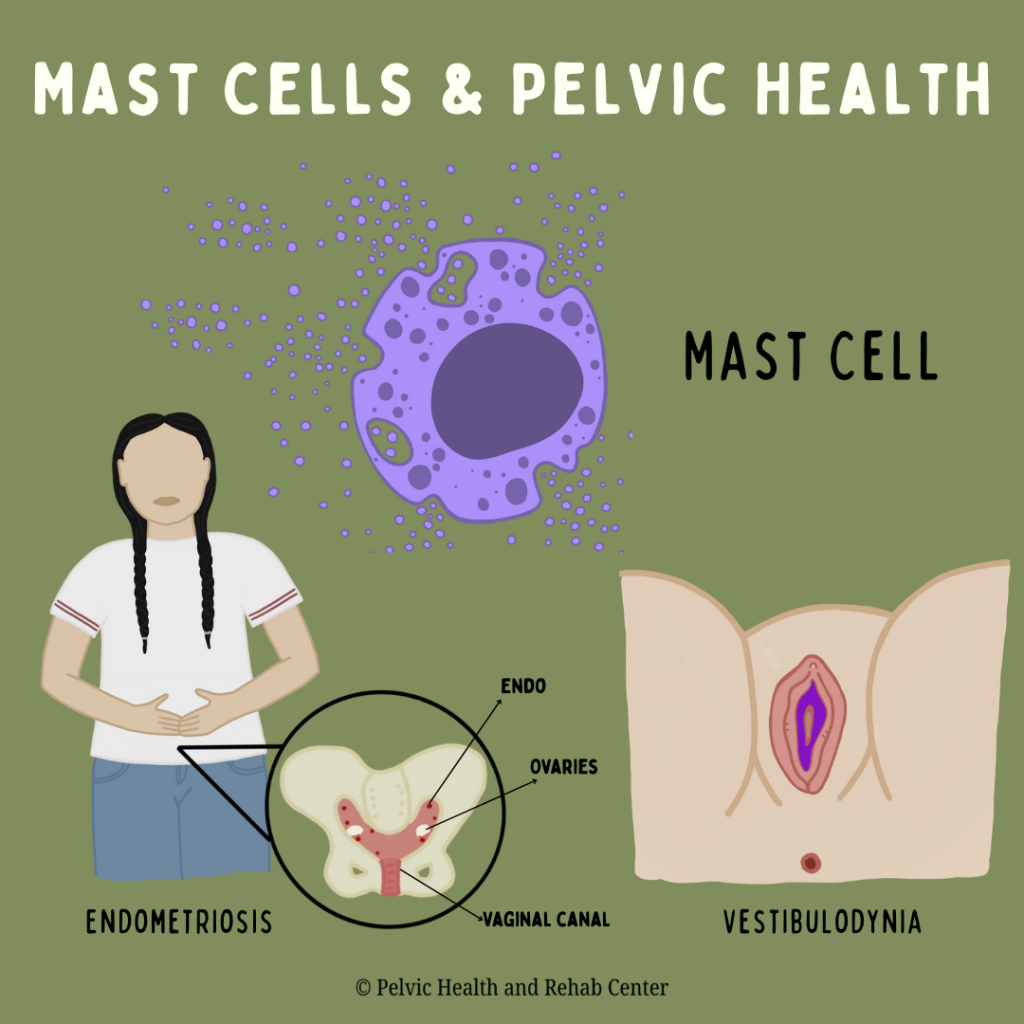
Last fall (2024), I attended a mast cell conference where my colleague Alyssa Yee, MD and I were invited to speak about the topic of pelvic pain conditions and the role of mast cells; specifically on the topic of endometriosis and neuroproliferative vestibulodynia (NPV) – a specific type of vestibulodynia characterized by excessive nerve endings and mast cells. Over the last few years, sexual medicine and pelvic health providers have been hard at work researching the involvement mast cells play in some of these more difficult, and very painful conditions causing debilitating pelvic pain and sexual dysfunction.
If you’re one of the many individuals dealing with chronic pelvic pain, painful periods, or discomfort with intimacy, you’re not alone—and you’re not imagining it. These symptoms are common, but they’re often misunderstood, misdiagnosed, or minimized. New research and clinical observations are shedding light on an overlooked contributor to this pain: mast cells.
In this blog, we’ll explore what mast cells are, how they relate to conditions like endometriosis and vestibulodynia, and why understanding their role could be the key to better diagnosis and treatment for many people, and ultimately, better treatment options.
What Are Mast Cells?
Mast cells are part of your immune system. Mast cells are commonly found in tissues that have exposure to the outside environment like the respiratory system, the gut, the genitourinary tract, our skin, and our connective tissue. When a substance comes into contact with a mast cell, the mast cell may be triggered and release a variety of substances like histamine, leukotrienes, and tryptase (and many, many more) in response to these triggers. Most people associate them with allergies, but recent findings show that mast cells can also play a role in chronic inflammation, pain, and even tissue remodeling.
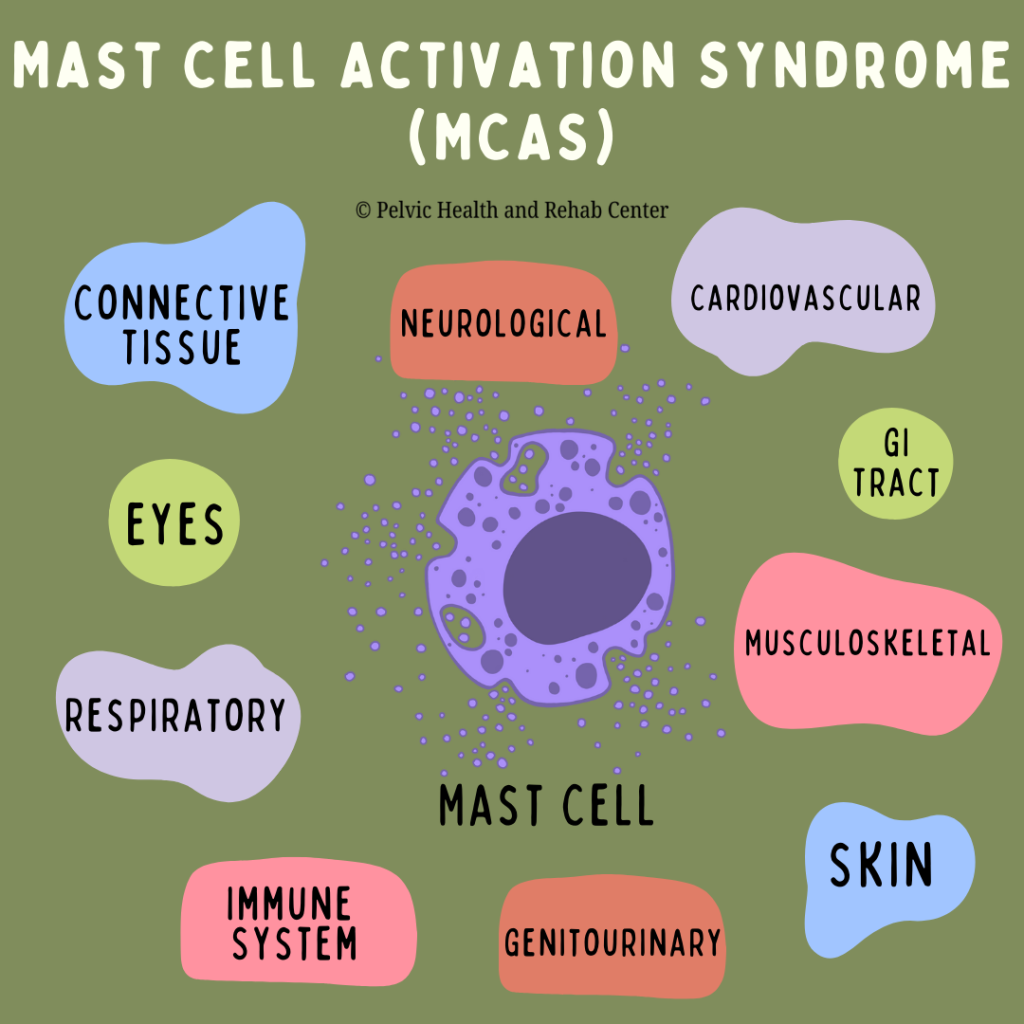
What is Mast Cell Activation Syndrome?
Mast cell activation syndrome is a condition where mast cells become over reactive and inappropriately release too many of their mediators (often inflammatory) and typically involve a wide range of symptoms and typically involve multiple body systems. This syndrome was defined and distinguished from a more rare condition, mastocytosis (increased number of mast cells) and allergic reactions.
Mast Cells and the Body Systems They Affect
A very thorough article by Dr. Lawrence Afrin and colleagues (2020) reviewed the diagnosis of MCAS, and we’ve summarized various symptoms specific to each body system below. Mast cell activation syndrome (MCAS) can affect nearly every organ system in the body. Chronic activation of mast cells results in a wide range of symptoms, making the condition hard to identify. Here are some of the key systems impacted:
- Skin: Flushing, itching, rashes, dermatographism (skin writing), and hives.
- Eyes: Irritated or often dry eyes, episodic difficulty focusing, lid tremors/tic
- Gastrointestinal: Nausea, abdominal pain, bloating, reflux, constipation, or diarrhea.
- Genitourinary: Bladder pain, urinary frequency, interstitial cystitis, vaginal pain (vulvodynia), and menstrual irregularities.
- Neurological: Headaches, dizziness, nerve pain, brain fog, memory issues, and sensory hypersensitivities.
- Cardiovascular: Heart palpitations, blood pressure swings, and lightheadedness or fainting.
- Respiratory: Shortness of breath, wheezing, cough, and sinus congestion.
- Musculoskeletal/Connective tissue: Muscle and joint pain, hypermobility (especially in conditions like Ehlers-Danlos Syndrome).
- Endocrine and Immune: Hormonal imbalances, thyroid dysfunction, and increased susceptibility to allergies and infections, hypersensitivity reactions, impaired healing
Understanding this broad impact helps explain why so many patients experience a long diagnostic journey—MCAS often mimics or overlaps with many other disorders.
Mast Cells, MCAS, and Pelvic Pain
Many people with chronic pelvic pain have conditions such as endometriosis, irritable bowel syndrome (IBS), vulvodynia, or painful sex (dyspareunia). While each of these conditions has its own unique features, what they often have in common is inflammation (and pelvic floor dysfunction!)—and for some people, mast cells may be a key factor in driving this inflammation.
A few years ago, Dr. Paul Yong, a sexual medicine OBGYN and researcher, presented a novel concept: Neuroproliferative Dyspareunia. Based on his research, he compared endometriosis and neuroproliferative vestibulodynia, demonstrating similarities in demographics, inflammatory factors, and the role of mast cells. In addition to the work of Dr. Irwin Goldstein and colleagues in NPV pathology over the last few years, along with many of us seeing individuals presenting with both endometriosis and NPV, further research to support Dr. Yong’s theory has begun; looking at both the pathology of the endometriosis lesions and vestibule in individuals with both conditions.
Let’s break it down with two key conditions where mast cells are now being studied more closely: endometriosis and vestibulodynia.
Endometriosis and Mast Cells
Endometriosis is a condition where tissue similar to the lining of the uterus grows on tissues and organs throughout the abdominopelvic cavity as well as distant sites throughout the body. These lesions have many different appearances, are often innervated, and respond to hormones which lead to inflammation, scarring, and pain.
A study by McCallion et al. (2022) demonstrates that endometriosis lesions can actually attract mast cells. These mast cells then release inflammatory substances that contribute to the pain and worsen the disease. In fact, mast cells and estrogen appear to work together, creating an environment that supports ongoing inflammation and nerve growth—both major sources of pain.
This means treatments that only target hormones (like birth control) might miss a key piece of the puzzle. Addressing immune and inflammatory responses, including mast cell activity, could offer new relief.
Vestibulodynia and Mast Cells
Vestibulodynia is simply defined as pain at the entrance of the vagina, often described as burning, stinging, or sharp discomfort, especially with touch, tampon use, or intercourse. Many people are told “nothing is wrong” or are misdiagnosed for years.
There are several causes and associated factors related to vestibulodynia, often related to a reduction in hormones from the use of birth control pills or certain stages of life such as menopause and breastfeeding. Another type is neuroproliferative vestibulodynia, either lifelong or acquired, that does not necessarily involve hormones. Neuroproliferative vestibulodynia is characterized by:
- Higher nerve density in the vulvar tissue (more nerves = more pain signals).
- Increased mast cells in the tissue, contributing to both inflammation and nerve growth.
This is not psychological—it’s a real biological process that can be seen under a microscope.
Why It Matters: A New Way to Look at Old Problems
Traditionally, pelvic pain has been explained through hysteria, psychological blocks, trauma, hormones or mechanical issues. Patients were often told to ‘it’s all in your head’ or to just manage their pain with birth control, surgery, or even a hysterectomy. While there may be a role for some of these interventions in certain cases, they don’t address the underlying immune system activity—like the involvement of mast cells.
By understanding that mast cells are active in both endometriosis and vestibulodynia, along with a wide range of symptoms in patients with chronic pelvic pain, our hope is that more research results in more understanding and more treatment options.
Chronic pelvic pain is rarely caused by a single issue. It often involves the immune system, neuromuscular system, hormones, and emotional well-being. That’s why the best care usually includes a team approach and persistence.
How PHRC and Pelvic Floor Physical and Occupational Therapy Can Help with Mast Cell-Mediated Pelvic Pain
If you’ve been dealing with ongoing pelvic pain, painful sex, bladder discomfort, or vulvar burning, and haven’t gotten clear answers, you’re not alone. At the Pelvic Health and Rehabilitation Center (PHRC), we specialize in helping people with complex pelvic pain.
Pelvic floor physical and occupational therapy (PFPT) is more than just exercise, it’s hands-on, expert care for the muscles, nerves, and tissues of the pelvic region. At PHRC, we’re trained to understand how all of these pieces are connected and interact to cause pain and disrupt your life. Conditions that are mediated or impacted by mast cells aren’t new to us, but our understanding of the condition is constantly evolving.
Our work focuses on:
- Manual therapy directed towards restrictions in the fascial and muscular system impacting the pelvic floor
- Calming down overactive nerves and reducing pain signals
- Improving blood flow and tissue healing
- Teaching you how to manage flares and avoid triggers
- Addressing posture and movement patterns that may be worsening symptoms
- Collaborating with your other healthcare providers (like pelvic pain specialists, allergists, or endometriosis surgeons)
Our evaluations and follow-up sessions are an hour long, one-on-one with an actual physical and occupational therapists – no aides or assistants, and very comprehensive.
Our therapists are very familiar with the very complex cases and diagnoses, not only are we trained to help address the myofascial implications, we can help screen for, and direct you, to the various professionals that can help with medical management.
Even if your condition hasn’t been formally diagnosed, we can help you start feeling better through targeted pelvic floor therapy and whole-body strategies; we will also help to facilitate the appropriate referrals and can provide helpful resources. We understand that seeing provider after provider is overwhelming and exhausting. We work with an extensive network of specialists and can help you navigate this journey, get a proper diagnosis, and an effective treatment plan.
If you’ve been struggling with pelvic pain, painful sex, or unrelenting vulvar discomfort and haven’t found relief, don’t give up. There is growing awareness and research into mast cell-mediated pain, and perhaps mast cells will be a key factor in managing some of these more complex conditions. We understand and we can help. At the Pelvic Health and Rehabilitation Center, we offer both in-person physical and occupational therapy in the Bay Area, Southern California, and New England, as well as virtual consults. If you are struggling with finding help, please reach out or visit our website for more information.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: immune cells, mast cell mediators, blood vessels, mature mast cells, other immune cells,
By Emily Tran, AMFT
By definition, mental health relates to our emotional, psychological, and social well-being. It influences how we think, feel, and behave in everyday life. But what really is mental health? For many of us, mental health might be seen only as a clinical concept; however, it is far deeper and much more personal. It is the underlying framework that allows us to process our realities, cope with challenges, and build resilience.
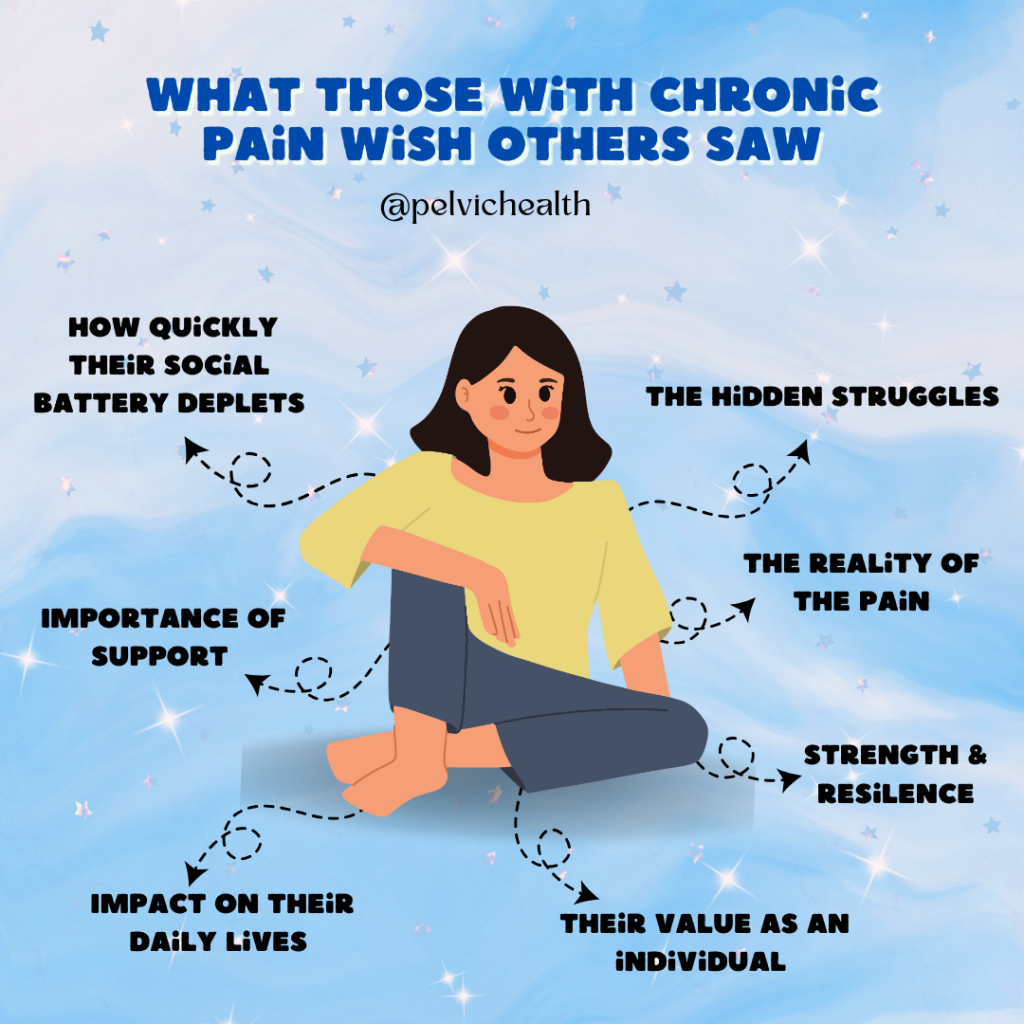
When we talk about chronic pain, particularly pelvic and vulvovaginal pain conditions such as endometriosis, vulvodynia, and pelvic floor muscle dysfunction, the role of mental health becomes indispensable. These chronic conditions go beyond physical discomfort and often bring with them a tangle of emotional and psychological challenges. Acknowledging and addressing our mental health in the context of these experiences is not only crucial but can be a transformative part of healing.
The Invisible Burden of Chronic Pain
Living with chronic pelvic pain means enduring more than just the pain itself. For many, it includes the ripple effects that impact every aspect of life.
- Symptoms dismissed by medical professionals can leave patients feeling invalidated and unheard.
- Painful sex, secondary to conditions like pelvic floor dysfunction or vulvodynia, not only causes physical distress but can strain intimate relationships, leading to feelings of shame or alienation.
- Infertility tied to conditions like endometriosis can deeply affect one’s sense of self and lead to grief or isolation.
- Challenges at work or even leaving a job due to pain and disability can cause financial stress and undermine one’s professional identity.
- Medical trauma from years of misdiagnoses or invasive procedures may lead to anxiety or PTSD.
These experiences aren’t just physical; they take a mental toll that often remains unspoken. Chronic pain sufferers may wrestle with feelings of inadequacy, frustration, and fear about their future. Navigating this landscape requires more than medical interventions for physical symptoms. It necessitates a compassionate and intentional focus on mental well-being.
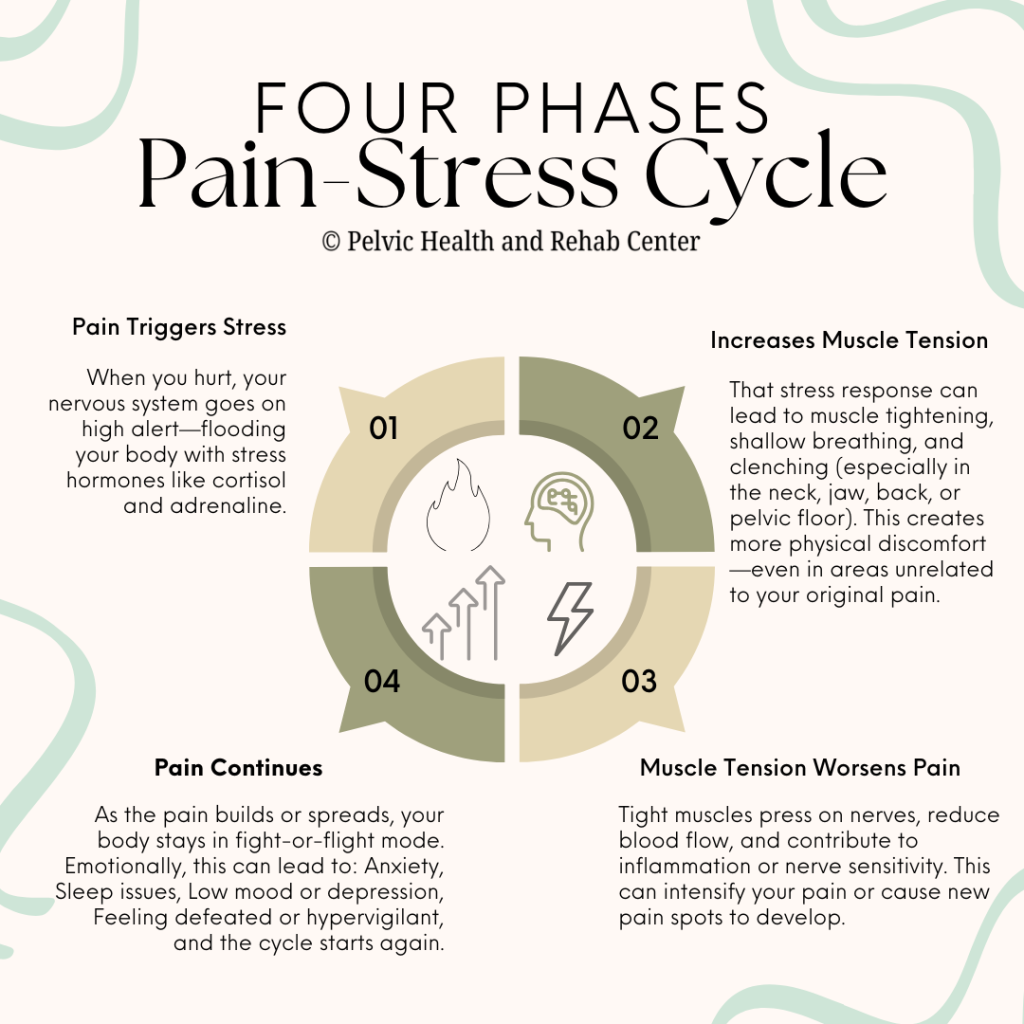
Why Mental Health is Crucial for Chronic Pain Management
The connection between chronic pain and mental health is undeniable. Numerous studies have shown that people with chronic pain are more likely to experience anxiety and depression. Pain doesn’t live in a vacuum—it affects mood, sleep, social engagement, self-esteem, and overall quality of life.
One of the most critical aspects of managing chronic pain is understanding the concept of the pain-stress cycle. Pain leads to stress, which in turn exacerbates the perception of pain. Addressing mental health can break this cycle, offering relief on both the emotional and physical fronts.
For example, those navigating chronic pelvic conditions often find themselves emotionally drained after years of advocating for their health, explaining their pain to dismissive doctors, or having their symptoms minimized by specialists. Focusing on mental health allows patients to rebuild their energy and resilience for moments like these.
Ways To Strengthen Your Mental Health
Improving mental health while managing chronic pain is not an overnight process, but small, intentional steps can make a significant difference.
1. Recognize and Validate Your Feelings
It’s okay to feel overwhelmed, angry, or even hopeless on certain days. Acknowledging your emotions is the first step towards addressing them. Remind yourself that these feelings are valid, and you are not alone in this experience.
2. Practice Self-Advocacy
Seasoned chronic pain people will know that advocacy is essential if you are wanting to get anywhere in the world. Not only can it help you regain a sense of control over your life (and body), it can help you prepare for navigating doctor’s appointments, speaking openly about your pain, and ensuring that you get the proper care and treatment that you need/deserve.
A few tips for practicing self-advocacy:
-
- Track Your Symptoms; This will help build your history and foundation for medical conversations. You may consider keeping a journal (physical or digitally) of your pain levels, triggers, treatments, etc).
- Be Prepared for Your Appointments; bring your own questions in, notes about previous treatments and symptoms. You may also bring your journal into your appointment so you can refer back to notes or timelines.
- Speak Up; this includes asking your provider to note in your chart when you feel your requests aren’t being taken seriously or followed through with.
- Ask for a referral; if the provider you are seeing does not specialize in the pain/area you are needing care in, asking for a referral to someone who does (like a pelvic PT, endo specialist, or pain psychologist) can make a huge difference. Sometimes a multidisciplinary team approach is best!
3. Strengthen Support Systems
Easier said than done, right? Building your network and ensuring it is a strong one can elevate the quality of your mental health. Support systems can include as many or as few people as you like. Whether it is your partner, family, friends, or even an online community of people navigating similar conditions, talking to others who understand and support you can alleviate feelings of isolation and loneliness.
4. Don’t be Afraid to Seek Professional Help
Finding a therapist, let alone actually going to see a therapist can be a challenging task! Add in (chronic) pelvic pain and it makes it that much more difficult. However, therapy can truly be a valuable resource for those suffering with any form of chronic pain or chronic illness. For example, Cognitive Behavioral Therapy (CBT), is proven to help patients reframe the way they view pain and reduce its emotional intensity. If therapy isn’t accessible, consider integrating mindfulness practices or utilizing a meditation app to help you manage stress.
5. Educate Yourself About Your Condition
Empower yourself by deepening your understanding of your condition so that you can make informed decisions about your care. Knowledge is a powerful tool for managing both your pain and the emotions surrounding it. Having a better grasp about your physical condition can help mentally understand its impact on your mental health while also broadening your ability to advocate for your own physical needs/treatment.
6. Cultivate Joy
This can be the most difficult portion of strengthening our mental health. While balancing mental and physical health can be outright exhausting, let alone challenging, it can be done! Amidst the sea of appointments, treatments, and other obligations you may have, it is important to challenge yourself to continue to find moments that bring you joy, no matter how small they may seem. This could be a good book, a favorite treat or meal, listening to music or even spending time with loved ones (or furry animals) can offer a mental reset.
Breaking the Stigma Around Mental Health and Chronic Pain
One of the most challenging barriers for many sufferers is the stigma surrounding both chronic pain and mental health. Stories of pain dismissal can discourage people from seeking help, while societal attitudes often equate mental health challenges with weakness.
But addressing your mental well-being is an act of courage and strength. By openly discussing the mental toll of chronic conditions like endometriosis or vulvodynia, we pave the way for a more empathetic and supportive environment. No one should have to choose between their physical and emotional health; both are equally deserving of care and attention.
A Holistic Approach to Healing
The interconnectedness between chronic pain and mental health highlights the importance of a holistic approach to wellness. By focusing on both the body and the mind, those suffering can create their own space for healing, growth, and empowerment.
If you’re navigating the complexities of chronic pelvic pain or other related conditions, know that your struggles are valid, and your mental health matters. Reach out, seek community, and never stop advocating for yourself!
A Call to Action for those Struggling with either Mental Health and/or Chronic Pain
I encourage you to take the first step toward reclaiming your narrative. Consider connecting with a chronic pain therapist (and/or a trauma informed therapist), joining local/online support groups, and/or explore techniques to nurture both your physical and emotional health.
By having tough conversations, spreading awareness and building our community, we can normalize and build a future where mental health is an integral part of every healing journey.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: acute and chronic pain, chronic pain syndrome, mental health conditions, mental health needs, persistent pain, pain management, mental health promotion, early intervention, , overall well being, daily lives, key facts, diagnosis
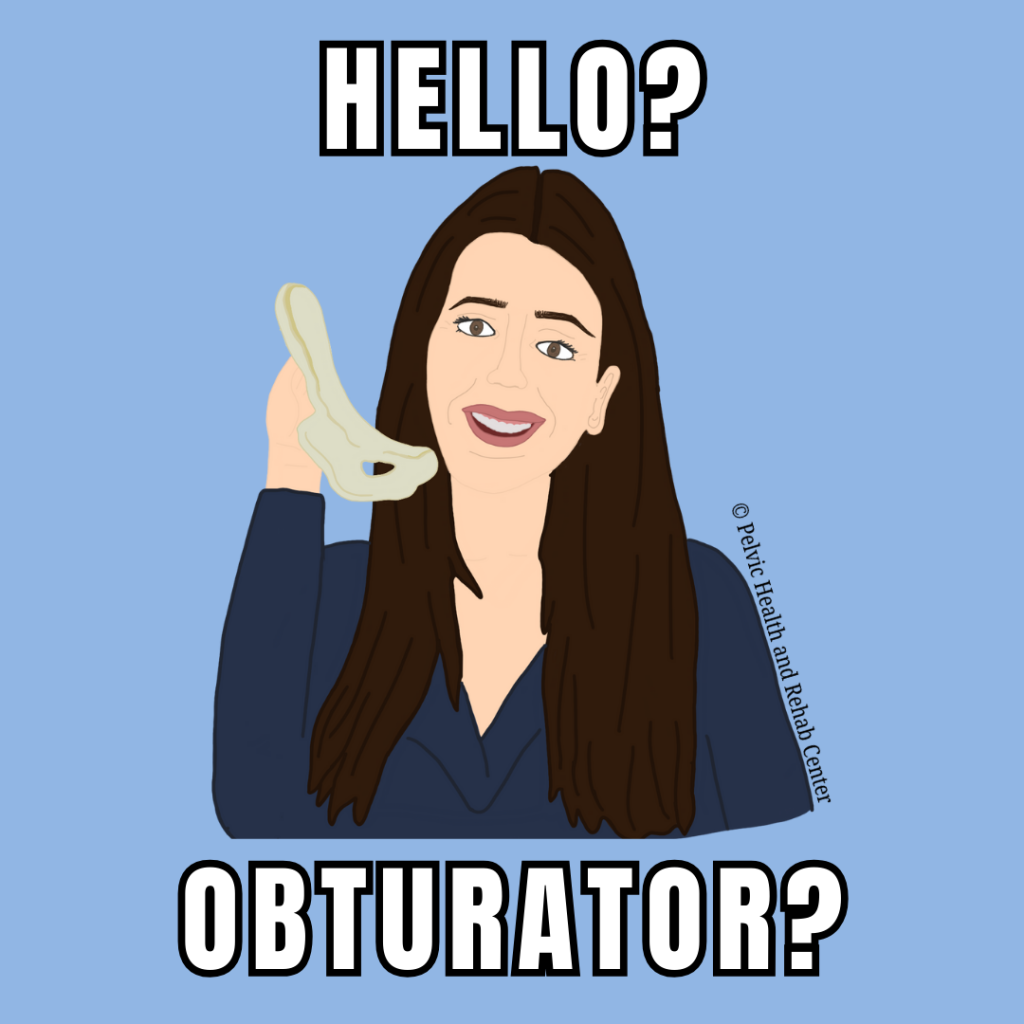
By Stephanie Prendergast, MPT, PHRC Pasadena
Comprehensive pelvic floor physical and occupational therapy includes much more than examination and treatment of pelvic floor muscles. Many factors contribute to normal and abnormal pelvic floor functioning, this post and series will focus on muscles of the pelvic girdle and how they influence the pelvic floor.
The pelvic girdle refers to our pelvic bones – the ilium, ischium, and pubis. Any muscle attaching to the pelvic girdle qualifies as a pelvic girdle muscle!
Today’s post is all about the small but mighty obturator internus muscle. While it’s not technically part of the pelvic floor muscle group (also known as the levator ani), it plays a crucial role in pelvic stability, comfort, and function. Because of this distinction, this little beast is often overlooked — and that’s a clinical oversight worth correcting. Here’s why.
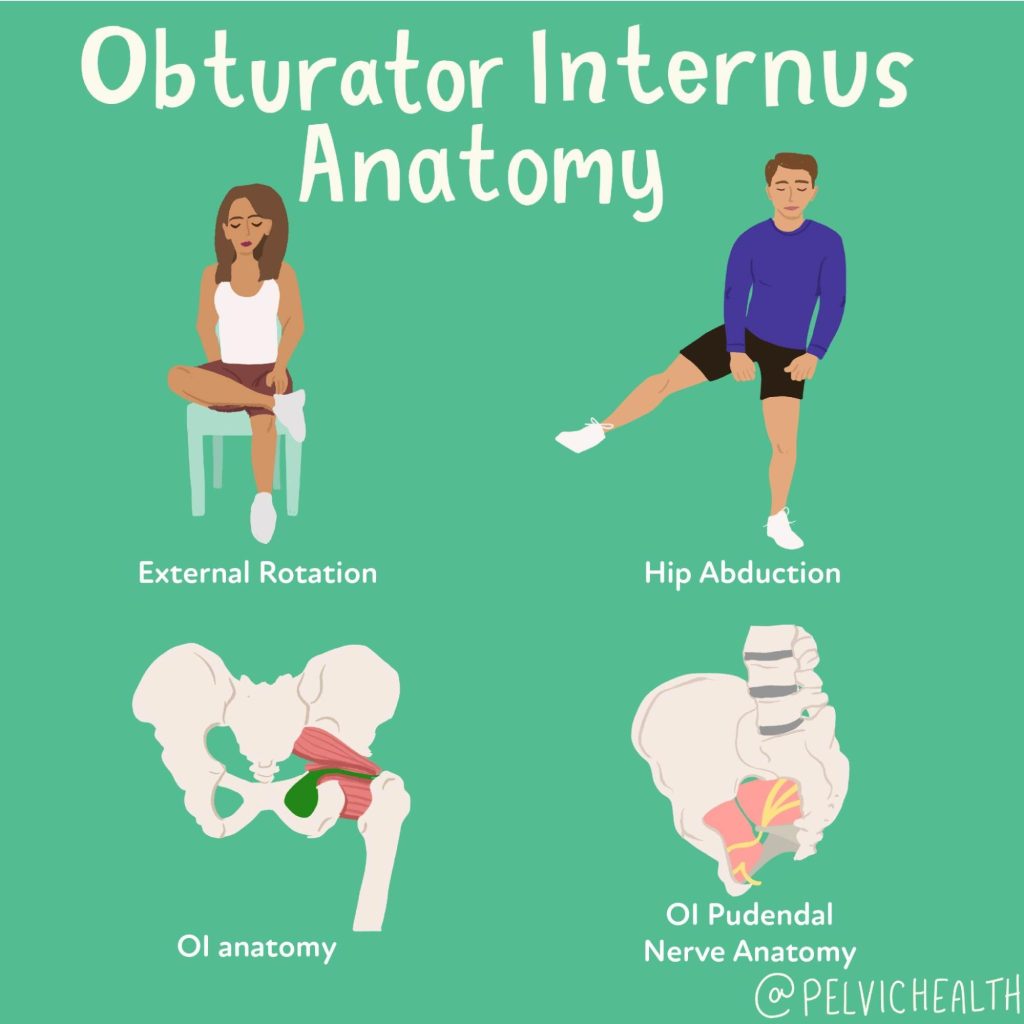
Obturator Internus Anatomy
The obturator internus (OI)originates inside the pelvic girdle and inserts into the greater trochanter of the femur. It is an external rotator of the hip, it contributes to hip abduction, and it is a stabilizer of the hip joint. This muscle makes a 90 degree turn and exits the pelvic via the lesser sciatic notch. This sharp angle renders this muscle to biomechanical compromise and dysfunction. It is innervated by the obturator internus nerve from roots L- S2. It is very closely tied to the piriformis and the other short rotators.
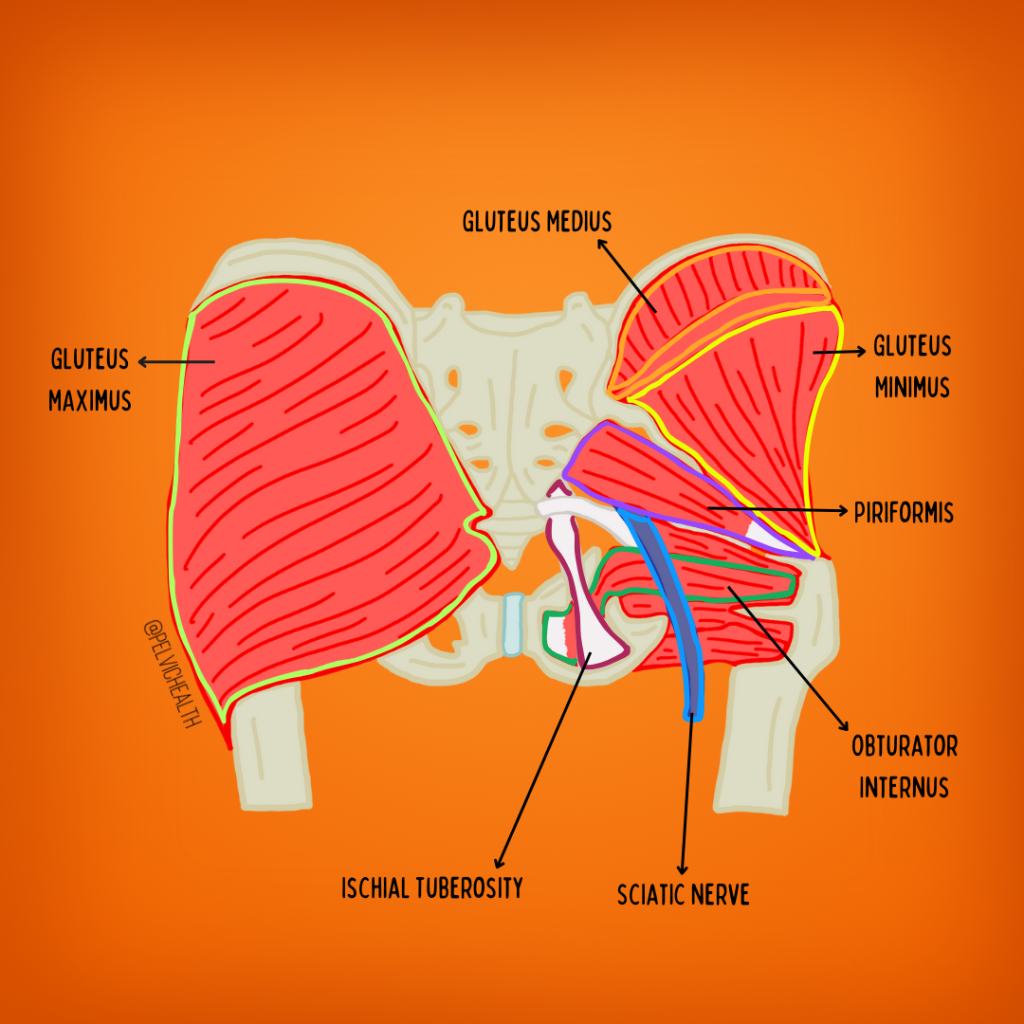
The obturator internus contains a facial canal called alcock’s canal, this is made up of the obturator internus muscle and fascia and houses the very important Pudendal Nerve. The pudendal nerve is a mixed nerve that has autonomic and voluntary functions, it innervates the majority of the pelvic floor muscles and directly manages urinary, bowel and sexual function. It also is responsible for sensation to the genitals, perineum, and anus. For more information about the pudendal nerve check out our popular pudendal nerve resource guide. The pudendal nerve is a big deal for our comfort and function and can be directly compromised by obturator internus dysfunction!
Causes of Obturator Internus Dysfunction
The obturator internus muscle can become tight/short, painful and dysfunctional for a number of reasons. Any muscle in our body can become impaired if it is taxed beyond its physiological capabilities. The physiologic threshold varies from person to person, the categories listed below may be the cause of someone’s impairments, they may not be relevant for other people atall.It all breaks down to individual anatomy and physiology. These include:
- Mechanical stressors
- Resisted external rotation or abduction during exercise
- Examples include clam shells, fire hydrants, monster and crab walks, sitting ‘outer thigh’ machines in gyms
- Prolonged sitting
- Sitting lengthens and compresses the muscle
- Piriformis Syndrome
- The piriformis and the obturator internus are both lateral rotators of the hip, dysfunction in one often means dysfunction in the other
- Hip pathology
- This includes labral tears, arthritis, impingement, etc
- Hip surgeries
- Examples include labral repairs, total or partial hip replacements, laparoscopic surgeries and repairs
- Sacroiliac joint and lumbar spine pathology
- Both sacroiliac joint dysfunction and lumbar pathology can cause impairments in the OI muscle
- Resisted external rotation or abduction during exercise
- Pelvic Floor Dysfunction
- The levator ani muscles and the OI muscles are closely connected via the tendinous arch. Dysfunction in one often means dysfunction in the other, but not always as dysfunction in one group vs both does occur but less frequently than dysfunction in both occurs
- Postural Dysfunction
- Posterior pelvic tilt
- Dis-coordinated core muscles
- Leg length discrepancies
- Pregnancy-related pelvic girdle changes
- During pregnancy circulating hormones result in ligamentous laxity and an increase in muscle tone in pelvic girdle muscles
- Neuralgias
- Pudendal neuralgia
- Irritation of this nerve can sensitize the OI muscle due to their close anatomic relation. This is bidirectional, OI dysfunction can also cause PN
- Sciatica
- The sciatic nerve also has close anatomic connections and OI dysfunction can cause sciatic symptoms and sciatic symptoms can cause OI dysfunction
- Pudendal neuralgia
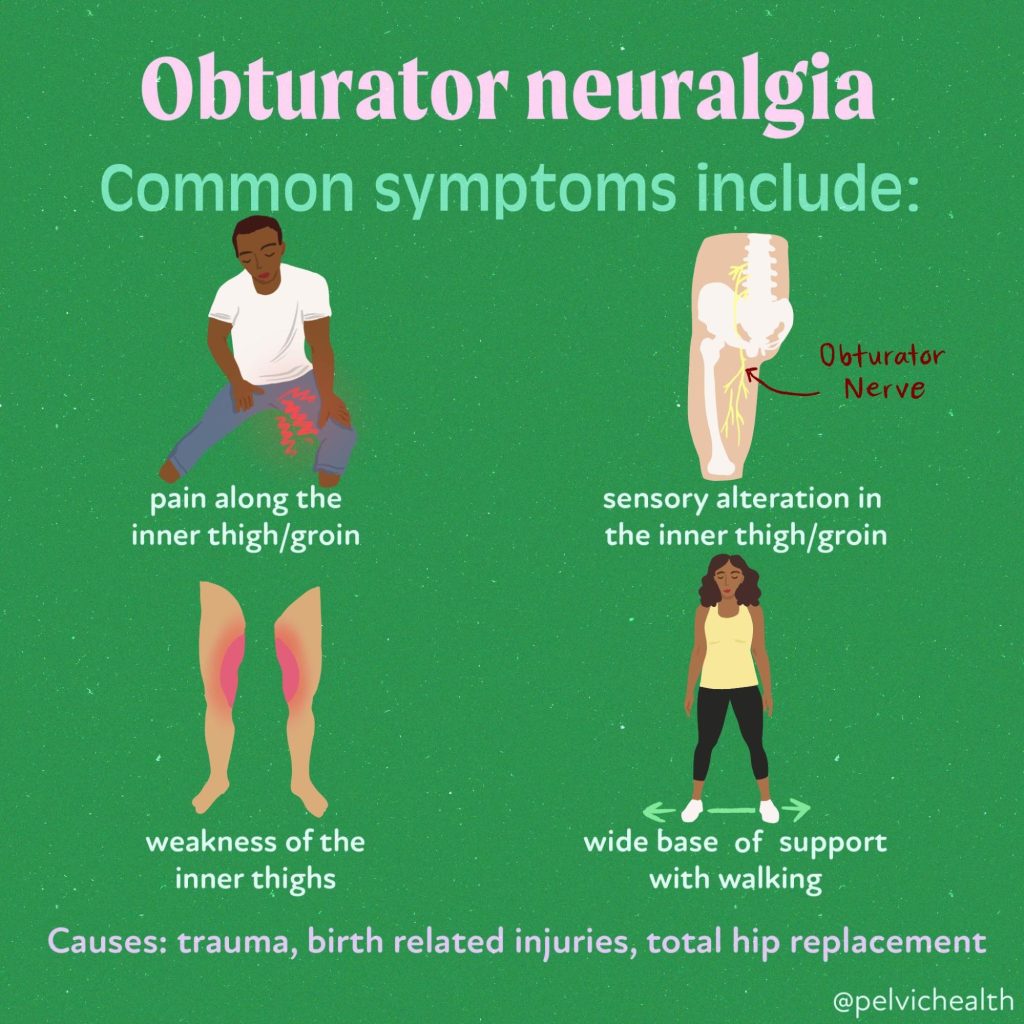
Symptoms of Obturator Internus Muscle Dysfunction vs Symptoms of Obturator Neuralgia
Obturator neuralgia is different from obturator internus muscle dysfunction. Obturator Neuralgia is less common and less frequently associated with pelvic floor dysfunction and pelvic pain.
 Symptoms of Obturator internus dysfunction can include some or all of the following:
Symptoms of Obturator internus dysfunction can include some or all of the following:
- Pudendal Neuralgia
- OI muscle dysfunction directly causes pudendal neuralgia by compression of the nerve at Alcock’s Canal. OI dysfunction also impairs the ability of the PN to slide, glide and move normally and therefore can trigger PN symptoms during all movements the muscle controls such as hip abduction and external rotation. Seemingly benign exercises can trigger a cascade of symptoms that leave patients confused and in pain.
- Pelvic floor dysfunction
- Pelvic floor dysfunction is often associated with discoordination of the pelvic floor muscles and the core muscles which compromise stability and can lead to Obturator Internus dysfunction.
- The close relationship of the levator ani and the Obturator Internus muscle is another mechanism rendering this muscle impaired
- ‘Deep’ pain in the buttock, pain at the ‘sit bones, pain at the tailbone
- Obturator Internus muscles commonly refer pain to these three areas
- Hip pain during or after exercise and/or sitting
- Pain with internal hip rotation
Diagnostic Considerations
Pelvic floor physical and occupational therapist should always include an examination of the Obturator Internus muscle during the transvaginal or transanal physical examination. The muscle is easily accessed by inserting a gloved, lubricated finger internally while the patient is lying on their back. The examiner can place the palmer aspect of the examining finger at 3 or 9 o’clock depending on the side of the body being examined. The examiner can place the non-examining hand on the lateral aspect of the knee and ask the patient to push into their hand, eliciting a contraction of the Obturator Internus muscle under their gloved finger. If the patient reports pain greater than a 3 out of 10 on a Verbal Analog Scale the muscle is considered to have myalgia and to be impaired.
A clinical test called Tinel’s Sign can be performed by angling the examining finger towards the ischial spine to palpate the Pudendal Nerve at Alcock’s Canal. The canal is located just distal to the ischial spine and the junction where the Obturator Internus connects to the tendinous arch which separates the Obturator Internus from the Levator Ani muscles. Applying light pressure, the sign is considered positive if light palpation elicits shooting stabbing pain in the territory of the nerve.
Conclusion
Including screening of the Obturator Internus muscle will improve a clinician’s understanding of their patients impairments and create a more effective treatment plan. Because this little beast is not part of the official levator ani group it may not be examined and as a result a therapeutic target may be missed!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: hip joint, obturator artery, obturator membrane, obturator internus muscle originates, pelvic surface