Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Stephanie & Liz
Next week, the Pelvic Health and Rehabilitation Center will turn NINE. In 2006, Liz and I wanted to be more involved in the field than our current work situation permitted. So, we quit our jobs, hoped we could pay our mortgages and started the Pelvic Health and Rehabilitation Center. We wanted to provide the highest quality of care to our patients, form better relationships with the local medical community, raise awareness about pelvic floor disorders, and teach courses. Initially, PHRC consisted of just Liz and me, no staff. As we got busier and began to hire administrative staff and physical and occupational therapistss, we realized our next and equally important goal was to create a work environment where our employees would never be treated as poorly as we were previously. As we all know, managing pelvic floor disorders is hard on the people recovering from it and for those of us trying to help. We began hiring motivated, compassionate, independent, fun people. Nine years later, PHRC is now a company: 5 clinics, 15 employees, uncountable courses, lectures, textbook chapters, and soon a book. Liz and I are grateful to have the team and company culture that we wanted, so this week we all answered a few questions about the day-to day inner workings of PHRC.
Every team member of PHRC works closely with each other, but their duties are different depending on if they have administrative responsibilities or therapeutic responsibilities.
Our administrative staff is essential to our operations, ensuring that the day-to-day flows smoothly, helping with social media and marketing outreach, and being the face of PHRC.

Allison & Casie
What do you like about working at PHRC?
Sara: My favorite thing about working at PHRC is being able to help people every day! Whether I’m helping patients by answering questions and scheduling appointments or helping the PTs manage their schedules, I’m always excited to help.Learning is one of my passions and I enjoy working at PHRC because I learn something new everyday.
Jenni: I truly enjoy helping people and I think that PHRC helps many people though direct patient care and through advocacy. I like the collaborative spirit at PHRC. I truly learn something new everyday.
Gabriella: I get to be a part of PHRC’s collaborative efforts to help people, educate, and increase awareness about pelvic pain. Most importantly, I get to witness women and men being empowered everyday as they take control of their health and their lives.
Connie: I like the fact when I wake up in the morning I get to work with a great group of people. I really look forward to coming to work.Becoming part of PHRC has been a great experience not only do I get to be a part of a great group but we all work together to help improve the quality of life for so many people, to see the look on peoples face when they come in & when they are D/C is amazing.
Our physical and occupational therapistss are some of the best in the world. Their endless dedication to their patients shows in every aspect of their demeanor and care. All of the PHRC physical and occupational therapistss recognized in one way or another that there was a gap to fill in the field of pelvic floor physical and occupational therapy. Here is some more insight into their drive to be pelvic floor physical and occupational therapistss.

Liz, Rachel, Malinda, Casie, & Stephanie
What do you like about working at PHRC?
Allison: I love the team mentality. We have meetings every week that give us an opportunity to bounce questions/ideas off of each other and ensure that we are able to give the best care possible.
Melinda: I enjoy everyone’s commitment to learning, critical thinking, and staying up to date.
Stephanie: I love the collaborative atmosphere at PHRC. Every person working here is committed to their job, to helping each other, our colleagues, and our patients. From a clinical perspective, I enjoy helping people who think they will never get better, I am from NJ after all and welcome this challenge. It is amazing to watch people regain their lives and to transition from the nervous new ‘patient’ in the waiting room to the healthy person that they were before they developed a pelvic floor disorder.
Rachel: I love how supportive everyone is and that I am always learning something new everyday!
Casie: I love knowing that I work with a group of the most talented clinicians who truly care about getting their patients better. I feel lucky that by working here my access to so many invaluable resources is within such close reach.
Elizabeth: I am grateful for the collaborative environment with caring, smart, and engaged therapists. Being able to talk through a very complex patient with pelvic pain with 7 other therapists is irreplaceable. Our administrative staff is simply the best of the best. Barely a day goes by that one of my patients do not comment on the knowledge, empathy, and responsiveness of our admin staff. Without them none of us would be able to do our job well.
Malinda: The minute I met Liz and Steph, I knew I wanted to work for PHRC. I wanted to be a part of a supportive team with weekly staff meetings, journal club, awesome administrative staff, and a common goal to help people with pelvic pain. I tell people I feel very fortunate to love my job and the people I work with.

Melinda
What inspired you to get started in pelvic floor physical and occupational therapy?
Allison: I actually heard about it from my gynecologist. I was having some pelvic floor issues myself and when she referred me to physical and occupational therapy I was like-I think this is something I can help other people with.
Melinda Fontaine: I heard an alumni talk about it when I was in PT school, and I liked the idea that I could help with really basic life functions, like peeing, pooping, and having babies.
Stephanie Prendergast: I worked in orthopedics my first year out of physical and occupational therapy school. I hated it. I either quit or was fired from 6 jobs within one year. I answered a job ad in the SF Chronicle (a NEWSPAPER!): Pelvic Floor PT wanted. Will train. When I heard that people, who were my age, could not sit down, wear tight pants, have sex, I knew I had to work in this field.
Rachel Gelman: There were two PTs who did pelvic floor at my first full time rotation in PT school. I thought it seemed cool, so I googled it and found PHRC! I contacted Liz and Steph and after spending a day here observing I knew this was what I wanted to do!
Casie Danenhauer: I’ve had my fair share of pelvic floor issues and had the opportunity to become a patient and shadow a therapist while I was in physical and occupational therapy school. I was lucky enough to have an elective course where we did our first internal exam and it was then that I realized what an incredible opportunity I had to help people on such basic quality of life issues.
Elizabeth Akinicilar: My desire to stop treating straight orthopedic patients and get into a specialty where I could really develop my manual skills in an environment I felt I could actually make a difference in peoples’ lives.
Malinda Wright: In my last year of PT school, the instructor responsible for placing students in clinical placement wanted to place me in a 2nd round of respiratory therapy. I baulked at this, because in the US we have respiratory therapist and I really wanted to learn about pelvic health. Fortunately, she placed me in a hospital treating women’s health and my interest in this field bloomed. I have never looked back.
How do you explain to people what you do?
Malinda Wright: I tell people I’m a physical and occupational therapists and I specialize in the pelvis. Most people mistakenly think I’m talking about the hips. I typically correct people and say I specialize in urinary, bowel, and sexual dysfunction as well as pain and prenatal/postpartum impairments. I also mention that I treat both men and women with these dysfunctions. Majority of the time people will ask me to explain what urinary, bowel, and sexual impairments are. When I explain, I always explain both sexs’ symptoms. I think it’s important for the public to realize men can have these symptoms too.
Melinda Fontaine: At a social gathering, I like to throw out that I’m a pelvic floor PT to see the reaction. People are either caught off-guard or totally interested in it. When someone asks me what that means, I usually say it’s mostly about the four P’s: Pee, Poop, Pregnancy, and Pain.
Rachel Gelman: My best friend and boyfriend call me the vagina whisperer, but I typically tell people I am a pelvic floor physical and occupational therapists and that I treat men and women with pelvic floor dysfunction, which can be pelvic pain, pain with sex, urinary or bowel dysfunction. This is usually followed by looks of confusion and lots of questions and usually ends up with me having to be blunt and say I work on the pelvic muscles internally via the vagina or the rectum
Casie Danenhauer: Two ways- either they drop the topic completely or have A LOT more questions. I try to use telling people about what I do as an educational opportunity because so many people aren’t even aware of what the pelvic floor is, even if they have dysfunction themselves! The conversation usually ends with, “Ya, so I basically have my finger in a vagina or a rectum for at least 50% of my day…”
Stephanie: I tell them that my degree is in physical and occupational therapy and I describe the symptoms: burning vaginal pain, UTI and yeast infection like symptoms constantly and in the absence of infection, post-ejaculatory pain, penile pain, inability to sit and wear pants. There is always confusion and often a later conversation because they themselves or someone they know may ‘have something that sounds like that’. I tell people the therapists at PHRC are Masters of Pelvic Disaster and direct them to the right office.

Buddy Cruiser & Abbie
What is your favorite tip to give your patients?
Allison: Sit on the toilet (even in public restrooms).
Malinda: Most of the world squats to poop, but Americans insist on pooping in toilets. Get a Squatty Potty. And stop peeing just in case.
Stephanie: Pee squatting in the shower. It makes the first void of the day less painful.
Rachel: Bowel mechanics and to look at your vagina!! That kegels are not always the answer and to decrease the amount of time you sit, the human body was meant to stand/move!
Casie: Breathe and indulge in self-care!
Elizabeth: Don’t hover above the toilet seat!!!!
Melinda: How to sit properly on the toilet with a squatty potty, and that Dr. Google is not always right.

Casie, Stephanie, & Sara
What advice do you have for patients?
Allison: Try to stay in a healthy mental space.
Melinda: You are your own best advocate. Stay informed. Ask questions.
Stephanie: You can and will get better, because you will. 15 years of experience has taught me that more often than not, certain treatment plans fail and need to be reworked. This can happen over the course of one treatment or several, but there is ALWAYS another option if something is not working or you cannot tolerate it. Stay committed and patient and know that you are not broken if something is not helping right away. Use your local medical providers to help you figure out what will help you.Do not be afraid of medications, when used properly medication can be a therapeutic part of the treatment process. Online forums are often scary and not reflective of the true landscape of healing from pelvic pain. Watch John Oliver. Humor helps everything.
Casie: Know that you are not alone. It can feel very isolating to have pelvic floor dysfunction because it’s not talked about in our society, but there are a lot of people out there with issues similar to yours.
Malinda: Stay informed and write your questions down so you don’t forget them when you walk into the provider’s office.
Elizabeth: Remain hopeful that your medical team will help you reach your goals.
What advice do you have for other pelvic floor PTs?
Allison: Take continuing education classes to build a strong network and community with your peers.
Rachel: Take classes and join any journal clubs/social networks to be able to stay current on the research and discuss cases. Having another set of eyes to look at a case can help you recognize something that you didn’t consider in treating a patient. Plus, this work can be mentally challenging so it is helpful to have a support network of providers who can relate to you.
Casie: Be open to incorporating as many “schools of thought” as you can into your approach for treating patients. For me a strong focus on the mind -body connection feels very important, but I also always have research articles to support what I’m doing from a more scientific perspective.
Malinda: Build a support network to bounce treatment ideas off of and to discuss more difficult cases.
Elizabeth: Work in a practice with other pelvic floor specialists who can mentor you. Make an effort to learn as much as possible about all the medical interventions related to pelvic pain, even if they are not within your scope of practice. Think of yourself as a colleague within the multidisciplinary team and nothing less.
Stephanie: When first starting treatment with a new patient, people do not always tolerate or immediately respond treatments. Think critically to troubleshoot through this. Promise that if you cannot help your patient you will help them find someone who will.
We hope this gave you a glimpse into our company as a whole. We are honored to have helped many people on their journey to wellness and we look forward to helping many more people the upcoming years! To learn more about our team, please visit our PHRC team page.
Kindest Regards,
The PHRC Team

Jenni & Nez
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
Every year over 70,000 American women are diagnosed with gynecological cancer, according to the CDC. A diagnosis of gynecological cancer can be devastating, but, as medical technology and research advances, more and more women with this diagnosis are becoming cancer survivors. Although surviving cancer is an amazing feat, many of these women are left with a decreased quality of life due to adverse side effects of the cancer treatment. It is common for gynecological cancer survivors to report one or more of the following: urinary dysfunction, bowel dysfunction, sexual impairments, pelvic pain, cancer related fatigue, and lymphedema. What many women – and sometimes their medical practitioners – do not realize is that their pelvic floor impairments and lymphedema can often be treated by a physical and occupational therapists.
Before we dive into physical and occupational therapy treatment, I want to first talk about what gynecological cancer is. Gynecological cancer refers to cancer within the female reproductive system. There are 5 main types of gynecological cancer: vulvar, vaginal, cervical, uterine, and ovarian. The signs and symptoms for each of these cancers differ; the CDC has put together an information booklet to help distinguish them. Medical treatment for gynecological cancer may include surgery, radiation therapy, chemotherapy, and/or hormonal therapy. Studies have shown that these treatments can have an adverse side effect on the pelvic floor. However, research has also shown that physical and occupational therapy can help ease these adverse side effects.1
One of the things we treat most often here at PHRC is muscle tension. Since gynecological cancer assaults our most private and vulnerable areas, muscle guarding during medical treatment is very common. Guarding occur when we tense up, and when we draw everything in to protect ourselves. Although it is a natural response to pain, guarding can increase pain and discomfort over time by causing muscle tension and spasms, as well as myofascial trigger points. Additionally, even after medical treatment has ended, muscle guarding may still continue as a response to discomfort such as with post-op surgical pain. Radiation therapy can also contribute towards muscle tightness, as there can be changes to the elasticity of the muscles that have been exposed to radiation. If these complications occur, patients may complain of tightness within the pelvis, abdomen, inner thighs, hips, and buttock muscles. Once present, the increased muscle tone and myofascial trigger points can also contribute towards pain with sexual intercourse, urinary and bowel impairments such as difficulty emptying the bladder, urinary and bowel frequency and urgency, and constipation. This is where therapy comes in. At PHRC, we can treat muscle tension by using manual physical and occupational therapy to release any muscle tightness and myofascial trigger points, and thus help ease discomfort within the pelvic region.
Another adverse side effect common with gynecological cancer treatment is scar tissue restriction. The development of scar tissue is a biologic response; scar tissue forms to heal the body from a wound. Surgery, such as hysterectomy or vulvectomy, naturally creates scar tissue as a part of the healing process after the surgical procedure. Scar tissue can commonly cause pain and discomfort due to lack of mobility or hypersensitivity along the scar. Pelvic radiation therapy can also create scar tissue. Radiation therapy, such as external beam radiation and brachytherapy, affects all tissues within the field of treatment, including muscles, tendons, ligaments, and skin. It is not uncommon for women to experience vaginal stenosis, narrowing of the vaginal canal, due to scar tissue forming from pelvic radiation. This can cause pain with sexual intercourse. Manual physical and occupational therapy helps to stretch, mobilize and desensitize the scar tissue, making the patient feel better.
Chemotherapy and radiation therapy are gruelling ordeals, inducing cancer-related fatigue in the vast majority of cases. Cancer-related fatigue can be described as extraordinary exhaustion disproportionate to one’s activity or exertion. It is not relieved by rest or sleep and disrupts quality of life. The keys to managing cancer-related fatigue are energy management, frequent rest breaks, and a well-designed and individualized exercise program. It may be hard for patients with cancer-related fatigue to be motivated to exercises, however research shows that physical activity is important with reducing the risk of cancer recurrence and mortality.2 Exercise is important for increasing strength and mobility, reducing pain and helping to prevent osteoporosis. Bone density can decrease when we go through menopause and many gynecological cancer patients go through abrupt menopause due to having their ovaries removed. A decrease in bone density can lead to osteoporosis and an increased risk of fractures. Physical therapy helps patients to maintain strong bones, mobility, balance, and everyday function all the while being cognitious of cancer-related fatigue.
Another risk to be mindful of is lymphedema. Lymphedema is when excess fluid collects in tissue causing swelling, also known as edema. Depending on the stage of the cancer, some gynecological cancer patients may have lymph nodes removed, mainly from the groin area. Lymph nodes are important for carrying lymph fluid, nutrients and waste. When lymph nodes have been removed from the groin, fluid may collect and cause swelling in the pelvis, abdomen, and/or leg. This swelling is called lymphedema. Not all gynecological patients develop lymphedema, however if lymph nodes have been removed, then the patient has a lifetime risk of developing lymphedema. Physical therapy intervention consists of patient education on how to prevent lymphedema and to decrease lymphedema if it has occurred through manual lymphatic drainage therapy.
Accepting a decreased quality of life after surviving gynecological cancer is not obligatory. Physical therapy treatment is available to ease the discomfort commonly associated with cancer treatment. Surviving cancer warrants a happy and celebratory life.
If you have any questions or comments regarding this topic, please do not hesitate to leave them in the comment section below.
Warmly,
- Yang, E.J., et al. Effect of a pelvic floor muscle training program on gynecological cancer survivors with pelvic floor dysfunction: A randomized controlled trial. Gynecology Oncology 2012; 125:705-711.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
I remember coming of age as a hormonal teen- before the days of google (believe it), hearing whispers about “orgasms”. It was like I went home for summer break with all of my childhood intact and when I came back to school in the fall, my peers were suddenly obsessed. I was bombarded with comments (from both sexes) of orgasms and boners and what “your O face” looked like. I remember the secretive giggles while referring to the Herbal Essences commercials and that scene with Meg Ryan in When Harry Met Sally. Or that time in Friends when Monica drew up a map of erotic zones for Chandler (and seemed to orgasm herself while saying the number 7). One of my friends even told me that 8 sneezes was equal to 1 orgasm…I anxiously awaited allergy season just to see if I could experience one of these orgasms by perfectly timing my pollen intake with my sneeze pattern to see if I could nail 8 in a row, and thus reach ORGASM (never, happened by the way).
I was certainly a late bloomer. I was still watching cartoons while others were getting into MTV. I didn’t have any older siblings, my friends were all my age or younger. But seriously, among all of the Cosmo articles with the tips, tricks, and advice about how to make orgasms better- I just had two questions; what are these glorious, yet elusive things? And why are there so many different definitions?
In the Clinical Psychology Review there are 26 different definitions listed for orgasm. Urban dictionary, listed 122 definitions! Here is one of my favorites: “Repetitive ‘Happy Moans’ indicating you have reached the peak of pleasure.” And they used it in a sentence: “Oh! Yes! That’s it! Ah! I’m having an orgasm!” (I even found one definition about the sneezes.) So, in the this week’s blog post I will attempt to give my best explanation of an orgasm. I realize that orgasms can be a combined experience of mental, physical, spiritual, and emotional components. But, since I am a pelvic floor physical and occupational therapists and an expert in the musculoskeletal system, I will focus on the physical aspects of an orgasm.
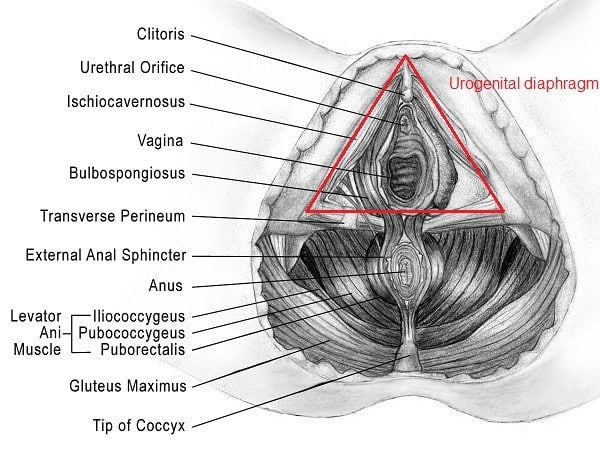
Before I get too clinical let’s talk about the anatomy. Some of you may remember Rachel’s blogs on penis and vulvar anatomy, which I highly suggest reading at some point. But today, I want to look a little bit closer at what as known as the urogenital diaphragm, the clitoris, and the Gräfenberg “G” spot.
The urogenital diaphragm aka urogenital triangle are the most superficial muscles of the pelvic floor, comprised of the bulbospongiosus, ischiocavernosus, transverse perineum and external anal sphincter. These are the most important muscles during arousal and orgasm.
The clitoris is located above the urethra at the intersection of the labia minora and extends vaginally to a point behind the pubic bone. The clitoris comes from the same cells that form the penis in a male.
The G-spot is typically described as being located 2-3 inches inside the anterior vaginal canal near the intersection of the urethra and bladder and may be of the same cells that go on to become the prostate in men. The G-spot is somewhat controversial between experts in the field because, though it has been studied since the 1940s, scientists have neither been able to prove its location nor its existence in women.
Also, the majority of women report that they need clitoral stimulation in order to orgasm, however this is totally variable from person to person. Research suggests that it is pretty common for women to report that they do not orgasm with penetrative sex alone.
Ok now let’s get to some of the more ahem…dry stuff regarding orgasm:
There are 4 phases of the sexual response cycle:
- excitement/arousal: in this phase the bulbospongiosus, ischiocavernosus, and pubococcygeus contract in order hold blood in the erectile tissues. In men this will present as an erection of the penis and in women there will be swelling of the clitoris and labia minora.
- plateau: pelvic floor muscle tension increases and prepares for orgasm
- orgasm: for both men and women an orgasm will produce rapid muscle contractions of primarily the superficial pelvic floor muscles (bulbospongiosus, ischiocavernosus, and pubococcygeus). Masters and Johnson found through direct observation that a male orgasm lasts approximately 10 to 30 seconds while a female orgasm lasts about 13 to 51 seconds. Interestingly, the interval of contraction is exactly the same for men and women-once every 0.8 seconds. So, you do the math-it’s a lot.
- resolution: phase in which further sexual stimulation does not produce excitement; varies between male and females
There are obvious differences between male and female orgasms, the most obvious being that male orgasms often culminate in ejaculation; however, there are some sex experts that say that men can learn to separate orgasm and ejaculation. Females can experience ejaculation as well, but it is not as common. Most of the research on this topic is incredibly old and outdated but just last month a study came out of France that explained the some of the mystery of the female ejaculation-turns out that it’s mostly urine coming out of the urethra….thanks France!
Because the superficial pelvic floor muscles are integral to achieving an orgasm, it is important that are functioning well. But what about when these muscles aren’t working as best they can? Here are some examples of issues we come across at PHRC:
- Pelvic/abdominal pain with arousal, orgasm, or afterward
- Sudden or gradual decrease in intensity and/or increased difficulty in achieving orgasm, or possibly aorgasmia; men may also describe decreased force of ejaculate
- Some of us have never been able to orgasm also called aorgasmic
- Persistent genital arousal disorder (PGAD): this is a complex issue that physical and occupational therapy can be very helpful in treating. Please click on the link to read Stephanie’s blog for more information
- Some people will report that they may have “over-masturbated”. While on the topic of orgasms, we should clarify this point. If pain/symptoms are occuring after masturbation and/or orgasm, it is logical that the two seem linked. However, it is not uncommon for the underlying problem to be due to tight pelvic floor muscles rather than masturbation itself.
All of the above issues can be caused by hypertonic pelvic floor muscles and potential trigger points. Think about it, if we need those superficial pelvic floor muscles to maximally contract and maximally relax once every 0.8 seconds for 10 to 51 seconds, that’s a big deal for those muscles. It’s like a major workout; and if they are already in a tightened state then getting them to further tighten, or relax for that matter, is going to be a problem. People with tight pelvic floor muscles often notice difficulty achieving orgasm or diminished orgasm intensity. This change often precedes the appearance of pelvic pain.
If you are experiencing any of the above symptoms consult with your physician and a pelvic floor physical and occupational therapists to address potential issues. All of the issues mentioned in this blog are highly treatable with PT intervention. If you need some help finding a pelvic floor specialist in your area, check out some previous posts on this matter here and here.
*Public service announcement: Can everyone please stop listening to Cosmo when they tell us to do Kegels for improved orgasm? If we are having issues, it is often because these muscles are too tight and trying to strengthen them only causes risk of more problems.*
Ok let me get off of my soap box now. My hope is that after you have read this blog that you will never try to get 8 sneezes in a row just so you can experience a “pseudo-orgasm”. No one experiences orgasms in exactly the same way. And it is because of this inherent variety that orgasms can be hard to explain. But I do know one thing-orgasms are important not only for our mental, emotional, and relationship health but for our pelvic floor muscles too! It is important to understand the anatomy involved and be able to recognize when something is not quite right and seek help.
Readers we want to hear from you! Do you have an orgasm or anatomy question? Please share in the comments section below!
And if you haven’t already, subscribe and follow us on Facebook and Twitter where the conversation on pelvic health is ongoing!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.