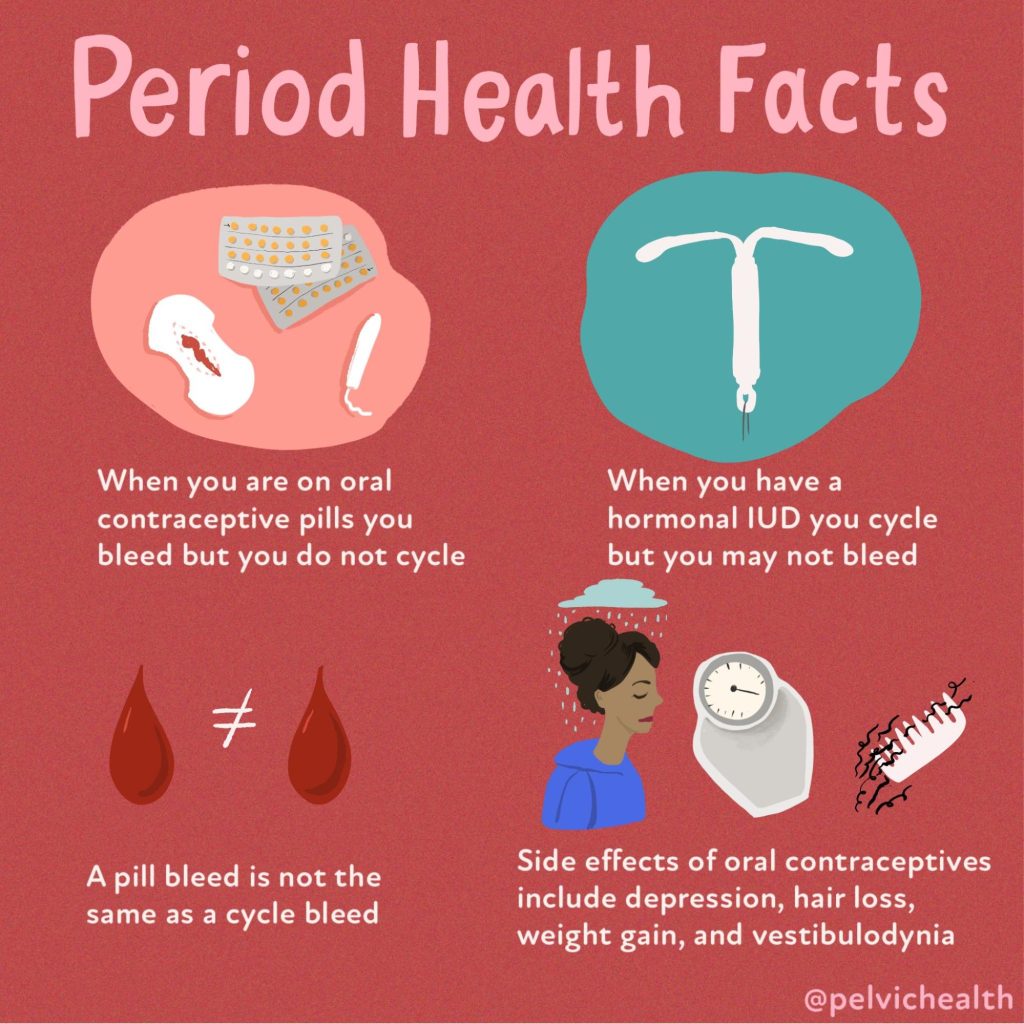
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
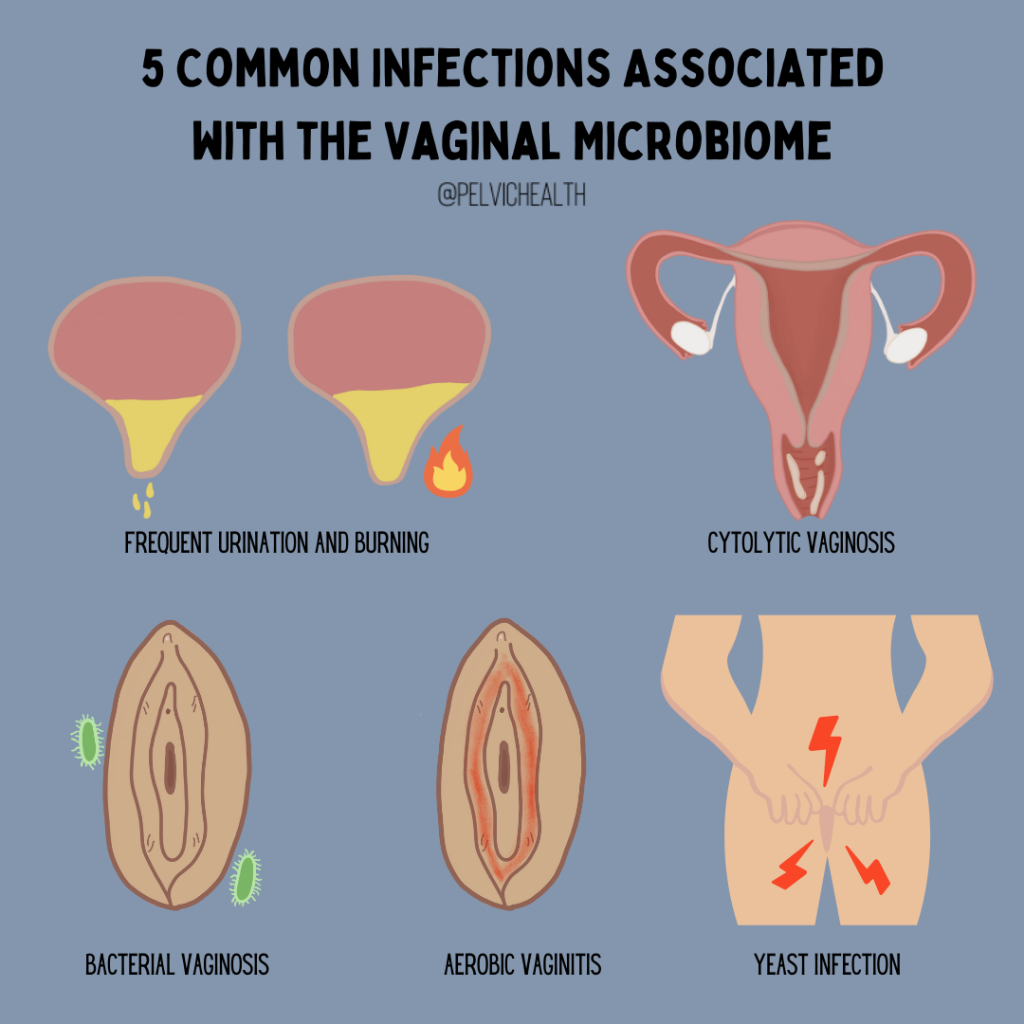
By Amanda Stuart, PT, DPT, PHRC West Los Angeles
The vagina, like the gut, hosts its own ecosystem of microorganisms, known as the Vaginal Microbiome (VMB). When there’s a disruption in this ecosystem (dysbiosis), it can lead to various infections affecting genital and reproductive health. These infections may include bacterial vaginosis (BV), aerobic vaginitis (AV), cytolytic vaginosis, vulvovaginal candidiasis (yeast infections), and sexually transmitted infections (STIs). In this week’s blog, we will discuss how imbalances in the microbiome play a role in these conditions and the latest evidence.
Recently, the human microbiome has been the focus of several areas of research, while it is in its infancy, we are starting to learn more about the role these invisible organisms have on our health. Before diving into changes, we need to understand what a ‘healthy’ environment looks like.
Oftentimes people initially associate the word “microbiome,” with gut health or maybe even the skin’s ecosystem. In this instance, the vaginal microbiome is just as important to overall well-being and deserves equal acknowledgment. This complex community of microorganisms plays a crucial role in maintaining vaginal health, preventing infections, and supporting reproductive and sexual health.
Composition of a Healthy VMB:
- Dominated by lactobacillus bacteria, which produce lactic acid and bacteriocins, this maintains a healthy acidic pH which reduces risk of these conditions.
- Studies show that lactobacilli and the resulting acidic pH of the vagina promote a healthy epithelial barrier, inhibiting the colonization of harmful microbes.
Host Factors affecting the VMB:
- Genetic factors, including racial background, can influence the composition of the VMB.
- Different Lactobacillus species, like L. crispatus and L. iners, have varying effects on the VMB and susceptibility to infections.
- L. crispatus is associated with lower risks of infections like bacterial vaginosis and vulvovaginal candidiasis, while L. iners may coexist with bacteria linked to dysbiosis.
Bacterial Vaginosis (BV):
- BV involves the displacement of Lactobacilli by anaerobic bacteria like Gardnerella vaginalis.
- BV-associated bacteria produce biofilms that disrupt the vaginal mucosal and epithelial barriers, increase the vaginal PH and produce enzymes that enhance their ability to colonize.
- Treatment with Metronidazole is initially successful but recurrence is common at a rate of 50% within as little as 12 weeks to 12 months.
- Introducing L. Crispatus following Metronidazole treatment has been shown to decrease recurrence by 15% at week 12.
Vulvovaginal Candidiasis (Yeast):
- Vulvovaginal Candidiasis often occurs when the vaginal environment is altered by antibiotic treatment, hormonal changes, metabolic disease, immunological incompetence, sexual activity or other conditions that permit yeast, mainly Candida species (spp.), to colonize the female reproductive tract.
- L. Crispatus dominance is associated with lower risks of Candida colonization.
- Treatment involves antifungal medication such as Fluconazole, Nystatin, etc.
Aerobic Vaginitis:
- Aerobic Vaginitis is typically associated with purulent discharge, vaginal itching, dyspareunia and an inflamed vaginal wall.
- Similar to BV, this condition presents with a reduction of vaginal Lactobacilli.
- The bacteria most frequently encountered in aerobic vaginitis include group B streptococcus (GBS), E. coli and Staphylococcus aureus.
- A combination of antibiotics and probiotics are commonly used for treatment.
Closing Thoughts:
Now that I’ve discussed certain characteristics of both a healthy and unhealthy vaginal microbiome, let’s conclude with talking about how to address the dysbiosis that can occur:
- Low-dose transvaginal topical estrogen has shown to be effective at engendering a more optimal Lactobacillus-rich microbiome while not increasing the risk of estrogen-sensitive cancers.
- Probiotics, combined with antibiotics or antifungals and estrogen therapy, may improve the vaginal microbiome balance and vaginal health.
- It is important to note that Cytolytic Vaginosis would be the exception in that probiotics would not be warranted as this is caused by an overgrowth of Lactobacilli.
- Other treatments like Statins and vitamin D may also be beneficial.
- Vaginal Microbiome transplants from healthy donors have shown promise in treating recurrent BV but come with risks and challenges.
Composition of the Vaginal Microbiome in Vaginitis
Condition Vaginal Microbiome Features
Cytolytic vaginosis |
Overgrowth of Lactobacillus spp. |
Bacterial vaginosis |
Enrichment of Atopobium vaginae, BVAB1, BVAB2, BVAB3, Gardnerella vaginalis, Mobiluncus spp., Mycoplasma spp., Porphyromonas spp., Prevotella spp., Sneathia spp., and Ureaplasma spp.; depletion of Lactobacillus spp. |
Vulvovaginal candidiasis |
Normal to BV-like vaginal microbiome; colonization by Candida albicans, Candida glabrata, Candida parapsilosis, Candida tropicalis, or Candida krusei. |
Trichomoniasis (STI) |
BV-like vaginal microbiome; invasion by Trichomonas vaginalis |
Aerobic vaginitis or desquamative inflammatory vaginitis |
Depletion of Lactobacillus spp.; frequent detection of aerobic, enteric bacteria, e.g., E. coli, Enterococcus spp., Staphylococcus spp., and Streptococcus spp. aBVAB1, “Candidatus Lachnocurva vaginae”; BVAB2, Lachnospiraceae BV-associated bacterium 2; BVAB3, Mageeibacillus indolicus. |
Understanding the intricacies of the microbiome extends beyond just gut health—it’s a holistic view of the human body’s interconnected systems, including those critical to pelvic health. The vaginal microbiome, for instance, plays a pivotal role in preventing infections and maintaining overall reproductive wellness. Incorporating prebiotic foods into your diet can support these beneficial microorganisms, fostering a balanced and healthy microbiome throughout the body. By raising awareness and promoting education on this topic, we can empower individuals to make informed decisions about their health and recognize the importance of a balanced vaginal microbiome. Understanding this often-overlooked aspect of health is essential for holistic wellness.
_____________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Elizabeth Akincilar, MSPT, Cofounder, PHRC Merrimack
The pelvic floor plays a significant role in several crucial functions, including bowel health, sexual function, and balance. However, certain common habits and misconceptions can lead to pelvic floor dysfunction. Did you know we were featured in an Insider magazine article? Let’s review these common mistakes and hopefully give you a few ways to avoid them in the future!
Here are some key points to remember:
Breath-holding during workouts
This common mistake can cause the pelvic floor to tighten, leading to sexual dysfunction and problems with urination and bowel movements. Holding your breath during activities like lifting heavy objects or exercising can increase pressure on the pelvic floor muscles, potentially leading to pelvic pain. Focus on maintaining proper breathing techniques during physical exertion.
Part I: Breathing Techniques for Pelvic Floor Health
Part II: Breathing Techniques for Pelvic Floor Health
Check out our full Youtube playlist about Breathing Techniques.
Sedentary lifestyle
Sitting for extended periods can compress the muscles and nerves in the pelvis, triggering urinary tract issues and chronic pain in the pelvic and lower back area.
Unnecessary or incorrect Kegel exercises
Not everyone needs to do Kegel exercises. Doing them unnecessarily or incorrectly can over-tighten the pelvic floor, causing sexual dysfunction, frequent urination, or difficulty with bowel movements.
Poor dietary habits
Good pelvic floor and bowel health are closely linked to a diet rich in fiber and adequate water intake.
Incorrect pooping technique
Western toilet designs aren’t ideal for proper bowel movements. Using a toilet stool or elevating your feet can improve your pooping technique while reducing the daily chronic pelvic pain experienced.
Ignoring pelvic pain
Any pain or discomfort in the pelvic region should be evaluated by a medical professional. Whether or not you have had your pelvic pain diagnosed or not, getting your pelvic pain treated can greatly improve your quality of life. When you ignore your pelvic pain, it can develop into chronic pelvic pain, but help is out there! Whether or not your pelvic pain is manifesting as: menstrual cramps, ongoing pain, bladder issues, constipation, or other symptoms, treatment options are available. Your pelvic health matters!
Overlooking symptoms in menopause and postpartum
Menopausal individuals should not ignore pelvic discomfort, and postpartum individuals should seek help for any form of incontinence. Whether you have acute pelvic pain or not, PFPT can be a beneficial part of any care plan for those under this category.
Enduring severe menstrual pain
Debilitating menstrual pain is not normal and should be checked by a healthcare provider. High levels of pain related to the menstrual cycle should be taken seriously.
Posture
Maintaining pelvic health requires awareness and proactive measures, including maintaining good posture, practicing appropriate exercise techniques, and seeking timely medical care for any concerns. Your pelvic muscles will thank you for paying attention to them!
Frequently Asked Questions
Q: What does a pelvic floor physical and occupational therapy appointment entail?
A: Hi! To put it simply, a PFPT appointment starts with an evaluation of your health history, followed by both an external and internal exam. Pelvic floor pt appointments can involve a lot, so we didn’t want you to miss any information. Here is a short clip about what to expect, followed by this extensive blog about the initial appt/treatment plan!
Q: I can’t find a provider, or you are too far away
A: This directory might help you locate a provider near you. The providers on the listed are trusted specialists who can assist in treating chronic pelvic pain.
Q: How can I book an appointment with you?
A: Great question! There are various ways to do so. You can fill out your information here and we can get a hold of you. Or you can book a telehealth appointment here. OR you could call any of our offices (phone numbers here) and schedule an appointment directly.
Additional resources we recommend:
Hormonal Prepartum Changes and Postpartum Complaints
Embracing IBS Awareness Month: A Pelvic Floor PT Perspective
What to Know About Your Menstrual Cycle
Clinical Manifestations of Endometriosis
Our Educational Resources for Pelvic Pain
(Purchase a copy of it via our website)
Just a few podcasts of so many…
- iCareBetter: Endometriosis Unplugged
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Alexa Savitz, DPT, PHRC Pasadena
Meet Jackie!
Jackie, six months postpartum, came to PHRC experiencing heaviness, pressure, muscle spasms around the rectum, and pelvic pain near her right hamstring and sit bone. She had a vacuum-assisted vaginal birth and a Grade Two Perineal Tear. Despite being ‘cleared for activity’ at her six-week check-up, her pain persisted. After consulting a urogynecologist, she was diagnosed with Grade One Uterine Prolapse. Jackie mentioned that she tended to tighten her pelvic floor out of fear of prolapse symptoms. During our treatment, she was fitted for a pessary, which she rarely wore due to discomfort caused by the device. Before pregnancy, she was active in hiking and weightlifting. Now, she struggled to walk a mile without symptoms, experienced pelvic pain while lifting her baby, and found it difficult to stand and cook dinner at the end of the day.
Goals for Pelvic Floor Physical and Occupational Therapy
Jackie aimed to return to hiking with her baby, resume general exercise, and eliminate pain while standing and cooking.
Physical Examination
The physical exam revealed the following impairments:
- Reduced coordination of her deep core muscles and mild diastasis recti
- Increased pelvic floor muscle tension with painful palpation of the transverse perineal and levator ani muscles
- Reduced pelvic floor muscle strength and poor neuromuscular coordination
- Myofascial trigger points in the pelvic girdle and weakness in her gluteal muscles
- Vulvar tissue dryness, which is now called the GenitoUrinary Syndrome of Lactation* and is treated with topical vulvar estrogen
*A groundbreaking study has revealed that high prolactin levels during lactation can cause genitourinary symptoms like vaginal dryness and urinary incontinence in those postpartum. This research sheds light on the under-recognized “Genitourinary Syndrome of Lactation” and underscores the importance of better screening and care for new moms.
Suspected Causes and Treatment Approach
I suspected her pelvic floor muscle tension stemmed from childbirth-related perineal injury and her body’s natural tendency to tighten due to fear of prolapse. This tension likely contributed to her pelvic floor pain.
We began with techniques to relax her pelvic floor muscles, including breathing exercises and internal pelvic floor muscle release, and down-training the soft and connective tissues of the pelvic girdle with mobilization techniques. Jackie was given home exercises to relax her pelvic floor through breathing, stretches, and foam rolling. We later incorporated self-symptom management using a pelvic wand to help release her pelvic floor tension. Additionally, we focused on deep core activation and diaphragmatic breathing to support her pelvic floor muscles and alleviate the heaviness and pressure. Proper breathing patterns are crucial to managing pelvic floor pressure and prolapse symptoms, especially during lifting and other daily activities. We also worked on lifting mechanics and carrying postures to help manage pressure, and included hip strengthening exercises to support her pelvic floor muscles and improve pelvic stability.
Achieving Goals!
By the fourth visit, Jackie was able to go cross-country skiing without experiencing heaviness or pelvic pain. By the sixth visit, her daily pelvic pain had resolved, with only intermittent pain during higher-level activities. We progressed her exercises, incorporating hip hinging, lunging, and hip stability with increased loads as tolerated, to mimic her daily activities and goals.
Although we planned for 12 visits, I saw Jackie for nine due to her moving from the area. By the ninth visit, she could hike one mile while carrying her baby, go on three-mile hikes without pelvic pain, and squat and lift her baby without pain. She was mostly symptom-free! Both of us were confident that she could manage any occasional postpartum symptoms independently with her home exercise program.
Why Every New Mom Deserves To See a Pelvic Floor Physical and Occupational Therapists
Whether you are pregnant or postpartum, pelvic floor therapy can be a great resource! Pelvic floor dysfunction and/or pelvic floor disorders can be treated by seeing a pelvic floor physical and occupational therapists! Postpartum pelvic floor recovery can seem intense, but your pelvic health is crucial for a variety of basic bodily functions. Your well being is important, especially when experiencing postpartum issues. Regardless of the pelvic floor issues you are experiencing, we hope referrals to see a pelvic floor therapist becomes more common practice to all those postpartum.
All pregnant and postpartum women can benefit from pelvic floor physical and occupational therapy given the crucial role these muscles play during delivery and how prevalent dysfunction is after birth. Pelvic floor physical and occupational therapy reduces the risk of pelvic organ prolapse, urinary, bowel, and sexual dysfunction and pelvic pain. Similar to other diagnoses we treat, many of our patients tell us they wish they knew about us sooner.
Postpartum pelvic floor therapy can help with pelvic floor disorders such as:
- Urinary retention, urgency, frequency, hesitancy, pain and incontinence (leaking)
- Constipation, difficulty with bowel movement, fecal incontinence
- Painful sex, diminished or absent orgasm
- Diastasis Rectus Abdominis
- Restoring core function and strength: abdominals and pelvic floor muscles
- Pelvic floor and pelvic girdle, low back, and hip pain
- Cesarean section and episiotomy scar tissue and pain
- Pelvic organ prolapse prevention and/or treatment
- Eliminate perineal pain and/or levator ani trauma
- Reduce pain from pelvic neuralgias
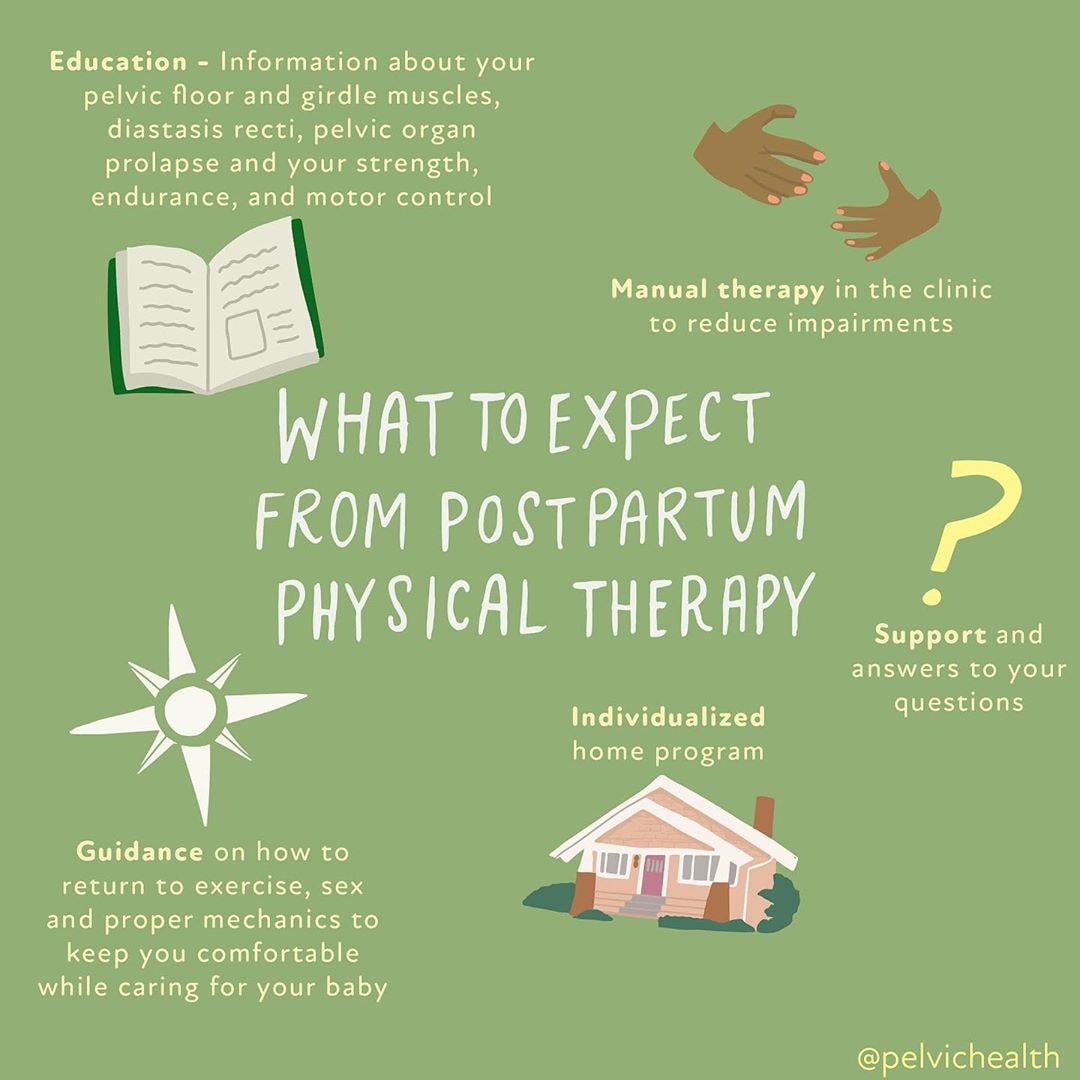
What to Expect from Postpartum Physical and Occupational Therapy
Education
Information about your pelvic floor and girdle muscles, diastasis recti, pelvic organ prolapse and your strength, endurance, and motor control. We want you to know about your pelvic floor anatomy!
Manual Therapy
In the clinic to reduce impairments (whether that was a vaginal delivery or not). Your pelvic floor therapist will create an individualized treatment plan.
Guidance
On how to reduce pain, return to exercise/physical activity, sexual intercourse (reducing painful sex) and proper mechanics to keep you comfortable while caring for your baby. You will receive a home exercise program with pelvic floor exercises geared towards your specific needs.
The Facts
- Up to 70% of women experience stress urinary incontinence in the postpartum period
- 36% of women have persistent Diastasis Rectus Abdominis after giving birth
- Up to 65% of women experience sexual dysfunction 18 months postpartum, regardless of the method of delivery
- 21% of women who undergo vaginal deliveries have Levator Ani Avulsion
- Vaginal deliveries are the number one risk for pelvic organ prolapse
- 77% of postpartum women have low back pain that interferes with daily tasks
- 51% of women can not perform a kegel with verbal cuing alone, 25% of women perform the exercise in a manner that promotes further (pelvic floor) dysfunction
Additional Resources from our PHRC Blog:
Diastasis Recti: What is it and who can it affect?
Moisturize My Vagina?! What you need to know
Top 5 Stretches to Relax the Pelvic Floor Muscles
Foam Rolling for your Pelvic Floor
Pain Interventions for Labor and Birth With a Partner
Other Postpartum Success Stories:
Postpartum Urinary Incontinence is Common: Here’s How We Can Help
Pain in your tailbone? You are not alone: Michelle’s Success Story
Success Story: Pelvic Floor PT Helped Charli Resolve Postpartum Pain
Success Story Jamie: Pushing Back Against Postpartum Prolapse
Source
Perelmuter, S., Burns, R., Shearer, K., Grant, R., Soogoor, A., Jun, S., Meurer, J. A., Krapf, J., & Rubin, R. (2024). Genitourinary syndrome of lactation: a new perspective on postpartum and lactation-related genitourinary symptoms. Sexual medicine reviews, qeae034. Advance online publication. https://doi.org/10.1093/sxmrev/qeae034
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!