Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By Stephanie Prendergast, MPT, Cofounder, PHRC Los Angeles
Dear Patients and Colleagues,
Change is a constant part of life, and after ten rewarding years in West LA I have made the decision to transition to PHRC’s Pasadena location. I started to fall in love with Pasadena when I opened this location in 2022, though I never imagined we would move here! My husband and I decided it was time for a change, so we packed up our two dogs and moved from Playa Vista to a historic home in Pasadena in March.
While I am excited about this change I also feel sadness as I transition from our West LA office. In 2014, I moved from the San Francisco Bay Area to open PHRC West LA, and for the past 10 years West LA has been home. During this time I had the pleasure of treating hundreds of patients, forming strong and valued relationships in the medical community, and growing our PHRC West LA team. I love being a pelvic floor physical and occupational therapists, a trusted medical colleague, and a mentor to PHRC staff. It is exciting to watch our West LA branch continue to grow and expand! While I am no longer treating patients in that location, I know the office is in good hands with Amanda Stuart, Jillian Ferran, and Sabrina Dickerson. Please be assured we are currently accepting new patients in West LA!
I want to express my deepest gratitude to everyone who has been a part of my journey at PHRC West LA. Your support, friendship, and encouragement have meant the world to me, and I am profoundly grateful for the opportunity to have been a part of this incredible community.
Starting this week I am accepting patients with pelvic pain disorders in Pasadena. I am excited to work alongside Alexa Savtiz, PT, DPT!
Now is a good time to share a little more about my interest in pelvic pain syndromes and why I hope you chose to come to PHRC Pasadena for your care.
Here is a little about me:
I am co-founder of the Pelvic Health and Rehabilitation Center (PHRC), which I established in San Francisco in 2006 alongside Liz Akinicilar. Together, we have expanded PHRC’s footprint to encompass 11 locations, including SF, Berkeley, Walnut Creek, Los Gatos, West Los Angeles, Westlake Village, Encinitas, Pasadena, CA; Columbus, OH; Lexington, MA; and Merrimack, NH.
Liz and I pioneered the first continuing education course focused on Pudendal Neuralgia, delivering the two-day program 37 times from 2006 to 2013. I was elected to the Board of Directors of the International Pelvic Pain Society in 2002, in 2013 I was honored to be elected as the first physical and occupational therapists to assume the presidency of the Society.
I am also an author, with numerous publications in peer-reviewed journals and textbooks. I enjoy lecturing at medical conferences and within the community on numerous pelvic health-related topics. As you can imagine, I have a LOT to say about pelvic pain and constantly advocate for our patients and pelvic floor physical and occupational therapistss. Therefore, Liz and I co-authored a book, “Pelvic Pain Explained,” in 2016. In 2019, we introduced a second continuing education course, “Advanced Management of Pelvic Pain Syndromes which we are proud to teach. Physical therapy schools do not include pelvic floor dysfunction in their curricula, it is part of our mission to help newer physical and occupational therapistss acquire the needed knowledge to help this patient population. Within PHRC we have trained over 50 physical and occupational therapistss and are very proud of our formalized training program! The therapists of PHRC undergo weeks of manual and didactic training, following the formal training program everyone here continues with 2.5 hours of weekly mentoring with our senior leadership team. As knowledge of pelvic floor disorders evolves we pride ourselves on staying current to offer our patients the highest quality of care.
In response to the evolving landscape of healthcare, me and Liz unveiled a groundbreaking virtual health/telehealth platform in 2020, extending our services globally to individuals seeking pelvic health consultations and mentoring for professionals in the field. In addition to clinical practice and teaching, I am proud to serve as an Associate Editor for the Journal of Sexual Medicine and I am currently faculty for the International Association for the Study of Women’s Sexual Health.
I am an advocate for individuals suffering from pelvic floor dysfunction. I am honored to become faculty for the Tight Lipped patient advocacy group, we are working to bring pelvic pain education into OBGYN residency programs. Similar to lack of pelvic floor knowledge in PT schools, OBGYNS are also not trained in pelvic pain syndromes in medical school. We will continue to help in any way we can! Recently we published an e-book “Vulvodynia, Vestibulodynia, and Vaginismus,” alongside Jandra Mueller and Liz. PHRC continues to make waves with its award-winning blog, “As The Pelvis Turns,” published every Thursday. Please connect with me on Twitter and LinkedIn Instagram, YouTube, TikTok, Facebook!

I am looking forward to serving the Pasadena community and continuing to advocate for this field!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
The Pelvic Health and Rehabilitation Center cordially invites you to an exclusive fundraising and educational event in honor of Pelvic Pain Awareness Month! We extend our heartfelt invitation to join us in lending support to two vital nonprofit organizations that rely on your generous contributions to sustain their impactful initiatives.
One of these organizations is Tight Lipped, a dedicated patient advocacy group committed to delivering sexual medicine training to OBGYN residents. Additionally, we champion the work of Riley Hooper, a remarkable documentarian and dancer, who is currently crafting a feature length film titled “Vestibule.” This poignant film chronicles Riley’s personal journey with neuroproliferative Vestibulodynia, shedding light on this often overlooked condition.
Understanding that patients grappling with pelvic pain often seek clarity and guidance, our team of medical experts is eager to provide answers and insights. In appreciation of your donations benefiting Tight Lipped and the film “Vestibule,” esteemed professionals: Dr. Rachel Rubin, Dr. Sarah Cigna, and Dr. Jill Krapf will join Stephanie Prendergast, Jandra Mueller, Riley Hooper, Bryn Silverman, and Keena Batti from Tight Lipped live for an engaging Q&A session and an exclusive sneak peek of the film.
Furthermore, as an added bonus, each attendee will receive a complimentary copy of the Pelvic Health and Rehabilitation Center’s recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Interested in joining us?
📅 Thursday, May 30th
🕜 4-5:30pm PDT/ 7-8:30pm EDT
📍 via Zoom
🎫 $15 minimum donation
PLEASE sign up and secure your spot with us!
Please forward this newsletter to everyone you know.
We thank you in advance for your donations and hope to see you there!
More About Tight Lipped:
Tight Lipped, a grassroots patient advocacy group, launched in May 2019 as a podcast, and quickly evolved into a platform empowering individuals with vulvovaginal and pelvic pain to openly discuss their conditions and seek care. Through community workshops, the creation and distribution of an 80-page zine called Opening Up, and advocacy campaigns, Tight Lipped strives to change healthcare systems’ treatment of these conditions, starting with advocating for standardized training in OB/GYN residency programs.
More About Vestibule:
VESTIBULE is a feature documentary that chronicles filmmaker Riley Hooper’s decade-long journey to diagnose, treat, and heal from Vestibulodynia. Combining documentary footage with stylized dance sequences, she tells the story of her body while exploring a maternal lineage of shame and resilience. What begins as a singular mission to have pain-free sex becomes a multi-generational story about sexual health, pleasure, and agency.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Elizabeth Akincilar, MSPT, Cofounder, PHRC Merrimack
Pelvic pain is a complex condition that can have various causes, including medical conditions, injuries, and certain behaviors. In this blog, we will discuss 10 common behaviors that can potentially lead to pelvic pain(and potentially chronic pelvic pain). It’s important to note that while these behaviors may contribute to pelvic pain, they may not be the sole cause. Whether it’s acute pelvic pain or not, you deserved quality treatment and getting your pelvic pain diagnosed!
Understanding these behaviors can help you make positive changes to prevent or alleviate pelvic pain.
Constipation or straining to evacuate stool
Chronic constipation or frequently straining during bowel movements can put pressure on the pelvic floor muscles, leading to pain and discomfort.
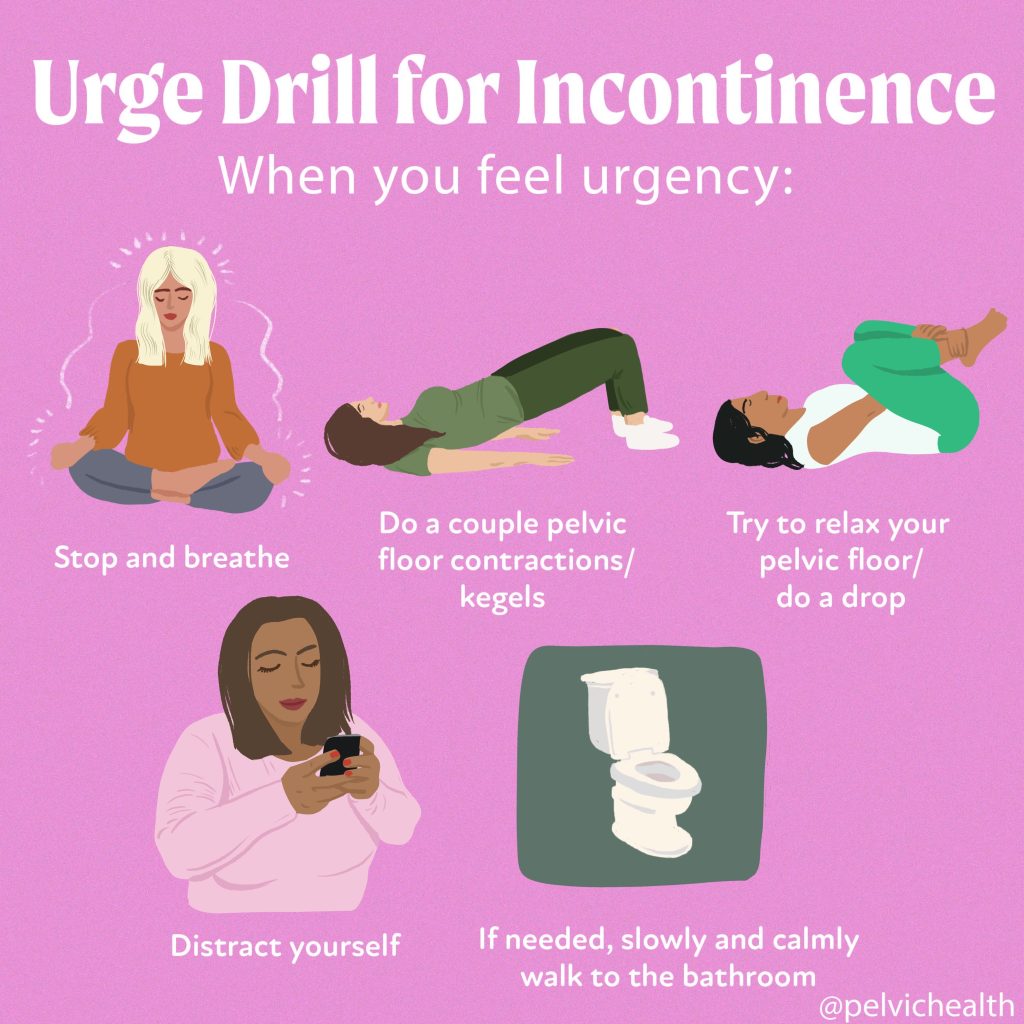
Holding your urine or delaying urinating
Ignoring the urge to urinate or frequently holding your urine can cause the bladder to become overactive and lead to pelvic pain.
Sitting all day
Prolonged sitting can cause the pelvic floor muscles to become tense, contributing to pelvic pain. Taking breaks to stand, stretch, or engage in light movement throughout the day can help alleviate this.
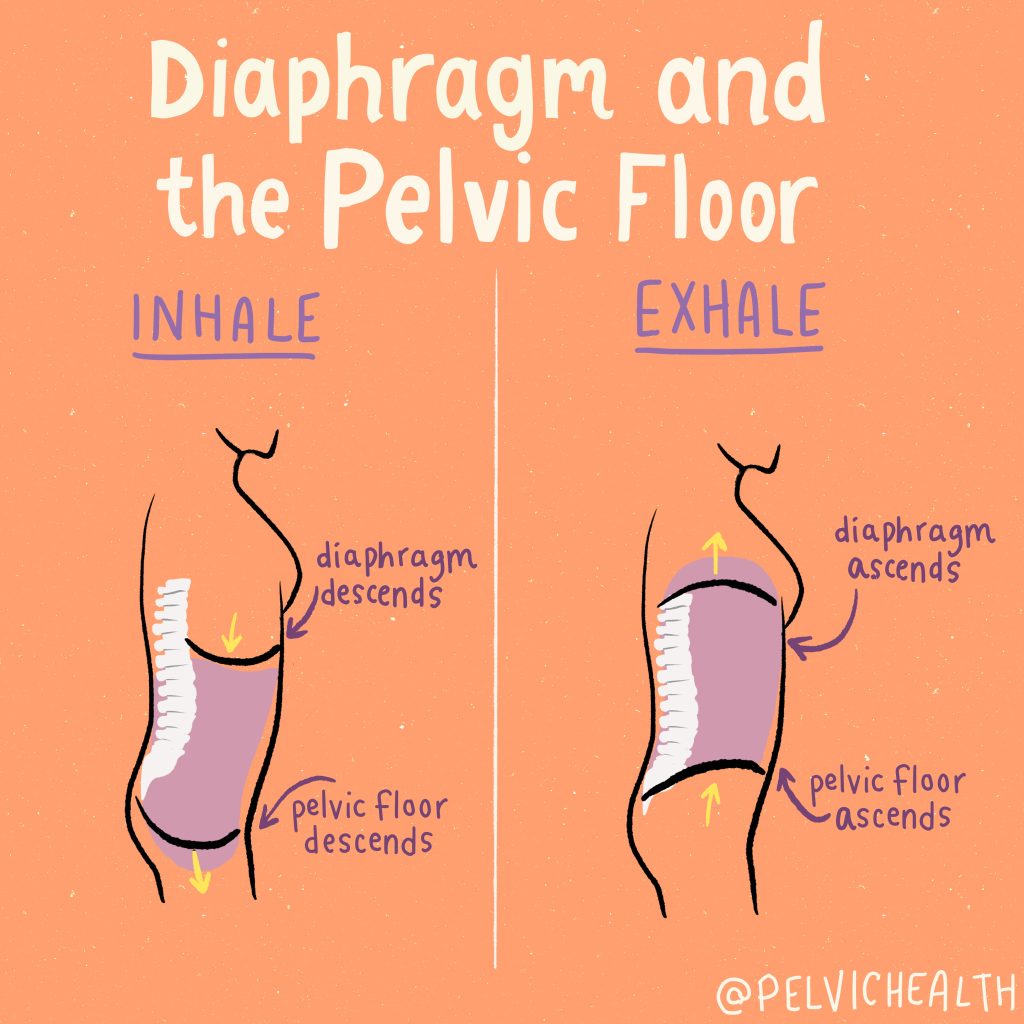
Holding your breath
Holding your breath during activities like lifting heavy objects or exercising can increase pressure on the pelvic floor muscles, potentially leading to pelvic pain. Focus on maintaining proper breathing techniques during physical exertion.
Clenching your butt
Habitually tensing or clenching your buttock muscles can put strain on the pelvic floor muscles, leading to pain and discomfort. Becoming aware of this habit and consciously relaxing your buttocks can help reduce pelvic pain.
Holding in your belly
Constantly holding in your stomach muscles can strain the pelvic floor muscles and contribute to pelvic pain. Practice consciously relaxing your abdominal muscles when not engaging in physical activity.
Incorrect breathing mechanics during weightlifting
Improper breathing techniques during weightlifting, such as holding your breath, can increase pressure on the pelvic floor muscles and potentially lead to pelvic pain. Consult with a professional to learn proper breathing techniques during exercise.
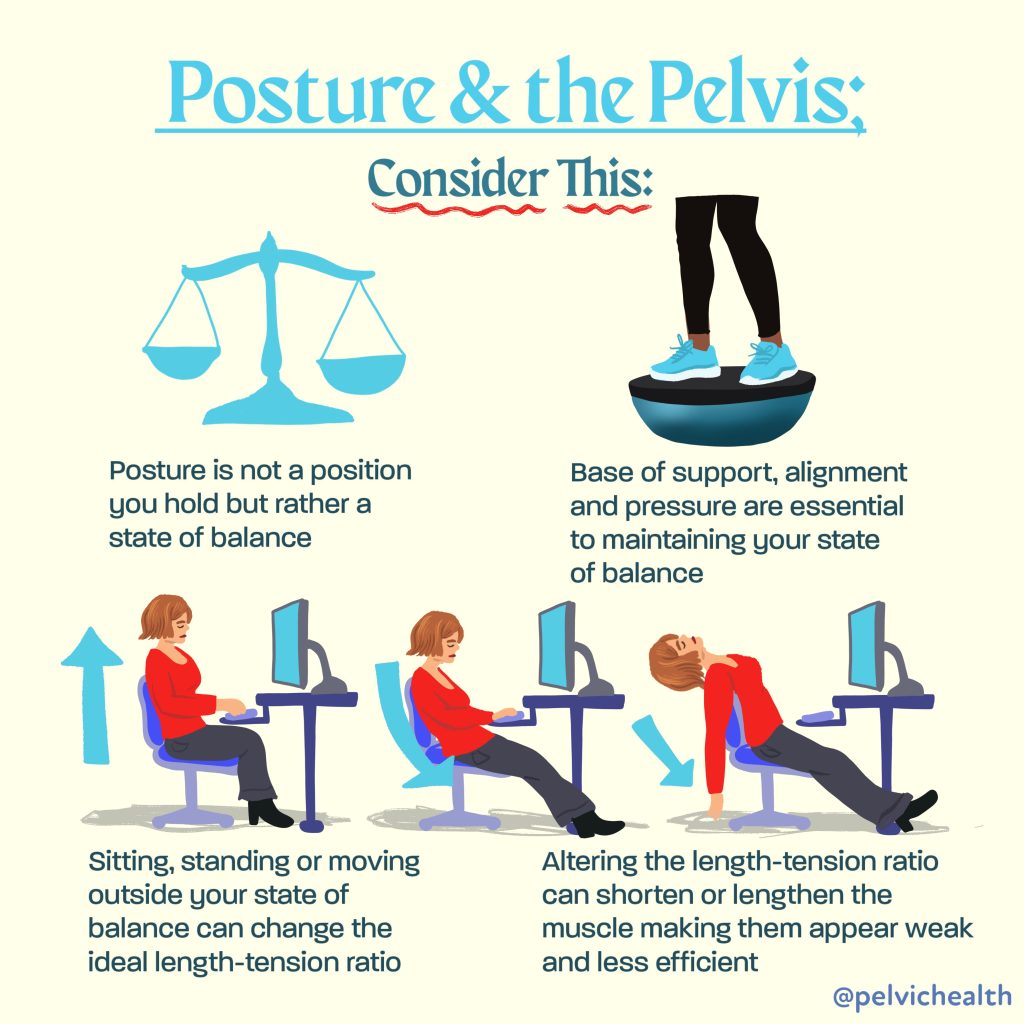
Postural dysfunction
Poor posture, such as slouching or hunching over, can affect the alignment of the pelvis and spine, leading to pelvic pain. Maintaining good posture and engaging in exercises that promote core strength and flexibility can help alleviate pelvic pain caused by postural dysfunction.
Edging during sexual activity
Edging, the practice of intentionally delaying orgasm during sexual activity, can cause the pelvic floor muscles to become tense, resulting in pelvic pain. Communicating with your partner and finding a balance that prevents excessive muscle strain can help prevent this.
Excessive or aggressive masturbation
Engaging in excessive or aggressive masturbation can strain the pelvic floor muscles and potentially lead to pelvic pain. Being mindful of your body’s limits and avoiding excessive or forceful stimulation can help prevent this.
It’s important to note that every individual is unique, and what may cause pelvic pain in one person may not affect another in the same way. If you are experiencing pelvic pain or discomfort, it is essential to consult with a healthcare professional, such as a physical and occupational therapists specializing in pelvic health, to properly diagnose and treat the underlying cause. They can provide personalized guidance and recommend appropriate treatment options to help alleviate your pelvic pain.
Remember, addressing these behaviors and seeking professional help can lead you on the path to pelvic pain relief and improved overall well-being.
Remember, addressing these behaviors and seeking professional help can lead you on the path to pelvic pain relief and improved overall well-being. Whether you are experiencing: chronic pelvic pain, pelvic inflammatory disease, painful menstrual cramps, irritable bowel syndrome, or other pelvic pain, help is available! Please check out our chronic pelvic pain resources below:
Resources:
How to find informed medical providers
International Pelvic Pain Society Find a Provider
International Society for the Study of Women’s Sexual Health
American Physical and Occupational Therapy Association’s Section on Women’s Health PT Locator
Herman and Wallace Find a Provider
Pelvic Guru Provider Directory
Have chronic pain but don’t know where to start? Get your pelvic pain treated today by requesting an appointment with us virtually to see how pelvic floor physical and occupational therapy can help you!
Frequently Asked Questions
Q: What are pelvic floor muscles?
A: The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
Q: What is pelvic floor physical and occupational therapy?
A: During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
Q: Do I need pelvic floor therapy forever?
A: The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
Q: What other causes pelvic pain should I know about?
A: We recommend checking out our services to find a complete list!
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.