Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By PHRC Admin Team
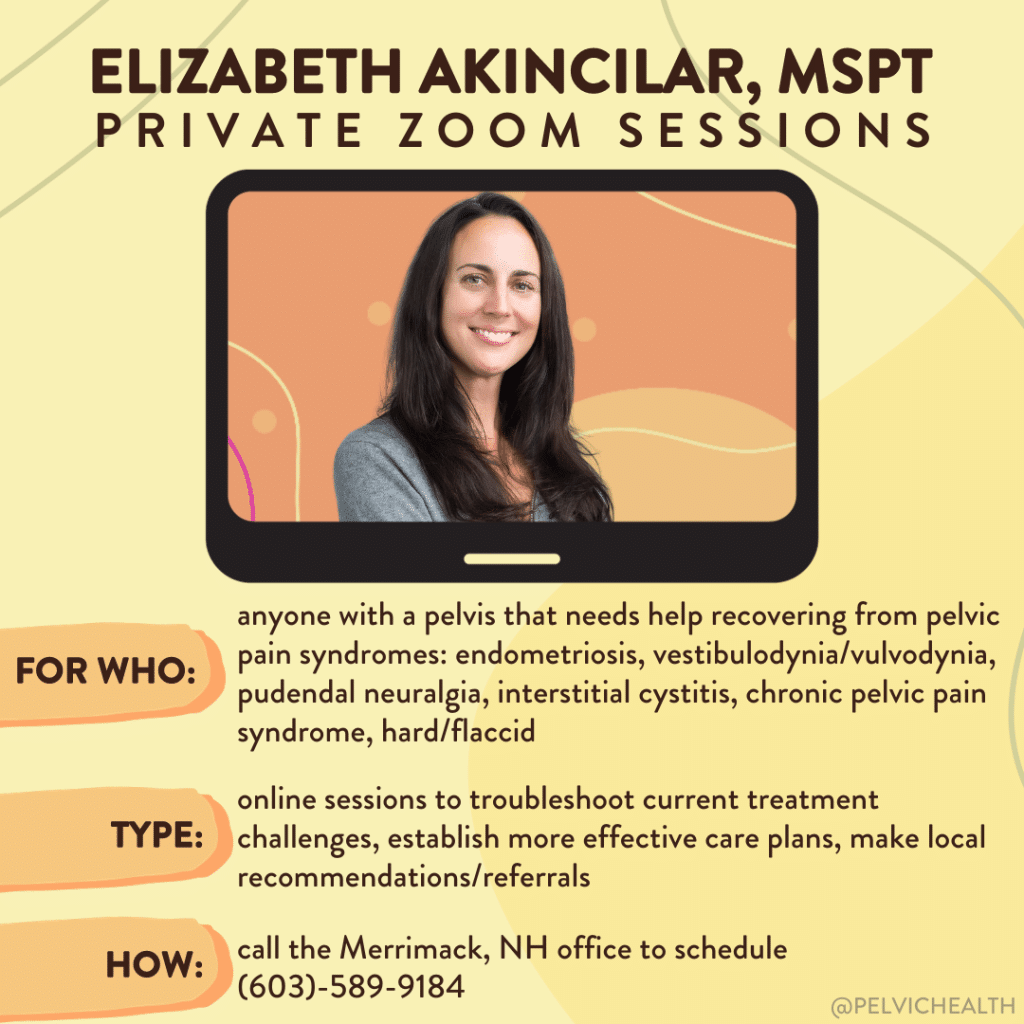
Did you know that the Pelvic Health and Rehabilitation Center offers a variety of virtual health services?
Often people do not understand their symptoms until they stumble upon our website, blog, or social media channels. Some people have a diagnosis but they do not have a pelvic floor physical and occupational therapists locally to help them. Other times people have a pelvic floor physical and occupational therapists but for some reason are not getting better or feel stuck in their treatment plans. Others just want another opinion from trusted experts.
Melinda Fontaine, DPT offers virtual consultations specifically for the pediatric population with pelvic health concerns as well as folks looking for postpartum care or post-prostatectomy care.
Jandra Mueller, DPT, MS offers virtual services (for pelvic pain and endometriosis). Jandra has a special interest in endometriosis and pelvic pain and has her Master of Science in Integrative Health and Nutrition. With the growing popularity of digital health, Jandra is able to offer these services to those throughout the United States as well as internationally. Therefore, she is able to help those that would otherwise not have access to a medical provider who can address both their physical complaints as well as underlying contributors to their pain.
PHRC Co-founders Elizabeth Akincilar, MSPT and Stephanie Prendergast, MPT primarily offer virtual consultations for complex pelvic pain syndromes such as pudendal neuralgia, vulvodynia, and endometriosis. Additionally, Elizabeth has a special interest in male pelvic pain/chronic nonbacterial prostatitis and neuropathic pelvic pain, whereas Stephanie has a special interest in menopause and Interstitial Cystitis/Painful Bladder Syndrome.
Over the last 2 years we have been honored to assist hundreds of people from around the world who were struggling with pelvic health and were unable to receive care locally or in-person due to the pandemic. We look forward to continuing this program to help folks navigate their health concerns and spread the word about pelvic health.
If you think you would benefit from a virtual consultation with one of our experts, you can schedule an appointment directly via our website.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By PHRC Admin Team
October is National Breast Cancer Month, a time to raise awareness about this deadly disease that affects millions of people across the globe. Approximately one in eight women will be diagnosed with breast cancer in their lifetime, making it the most common form of cancer among women in the United States .
This month is an opportunity for everyone to join forces and work together to support those affected by breast cancer as well as promote education, research and early detection. It’s also an important reminder that there are more survivors than ever before due to advances in medical technology and treatments over the years.
One way to get involved during National Breast Cancer Month is to wear pink ribbons or donate money towards breast cancer charities like National Breast Cancer Foundation (NBCF). NBCF has provided funding for screenings, diagnostic testing, patient navigation and survivor support services since 2003. Participating in walks or runs such as Susan G. Komen’s Race for the Cure® are also great ways to show support while raising funds for research into causes, prevention and cures .
Aside from donating money or raising awareness through events, individuals can look out for their own health by getting screened regularly for breast cancer. Early detection is key when it comes to successful treatment against this disease so make sure you keep up-to-date with your mammograms if you are over 40 or follow your doctor’s screening advice if you have a family history of breast cancer.
National Breast Cancer Month serves as an important reminder about how far we have come in the fight against this horrible disease thanks to increased awareness and funding going towards research into its causes and treatments. We should take every moment of October to celebrate all those who have survived breast cancer while striving forward towards a cure.
If you or someone you know has been diagnosed with breast cancer, there are several resources available to help navigate the journey.
For information and support, organizations like Susan G. Komen provide a wealth of resources such as access to a breast cancer helpline as well as helpful information about options for treatment, financial assistance and insurance coverage. They also have online discussion boards and chat rooms where survivors can talk with others who have gone through a similar experience.
The American Cancer Society is another great resource that provides free educational materials and support services like coaching programs and free rides to medical appointments through their Road to Recovery program. Additionally, the ACS partners with more than 200 local cancer organizations across the country so that individuals can find support services close to home.
Other organizations such as BreastCancer.org are dedicated specifically to providing accurate and up-to-date information about breast cancer diagnosis, treatments and care for those affected by it. You can also find many nonprofit foundations that fund research into causes, prevention and cures for breast cancer like the Breast Cancer Research Foundation (BCRF) or the Avon Foundation for Women which provides grants to support screenings, diagnostic tests and treatment options for underserved communities.
No matter your needs during this difficult time, make sure you reach out for help – whether it be from family members or professional resources – because knowing you are not alone in this fight is invaluable when facing breast cancer head on.
Resources:
-
The American Cancer Society (ACS): Provides resource lists for free or low-cost mammograms and financial assistance.
-
National Breast Cancer Foundation: Offers various resources to help spread awareness during Breast Cancer Awareness Month.
-
World Health Organization (WHO): Provides resources to increase support for the awareness, early detection, treatment, and palliative care of breast cancer.
-
Breast Cancer Now: Focusses on raising awareness around secondary breast cancer.
-
Commission on Cancer (CoC) and National Accreditation Program for Breast Centers (NAPBC): Offers resources to promote Breast Cancer Awareness Month.
-
CDC’s National Breast and Cervical Cancer Early Detection Program: Offers free or low-cost mammograms to women who have low incomes and are uninsured.
-
Breast Cancer Foundation: Provides a range of targeted materials approved by its Medical Advisory Committee, available free of charge.
-
CancerCare: Provides breast and cervical cancer resources.
-
Susan G. Komen Patient Care Center: Your go-to source for timely, accurate breast health and breast cancer information, services, and resources.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Stephanie A. Prendergast, MPT, Cofounder, PHRC Los Angeles
Our muscles are hormonally sensitive structures and weaken over time as we experience hormonal decline. In addition, the prevalence of pelvic floor dysfunction rises and the combination of these two scenarios can cause people a fair amount of grief.
A recent study showed 95.3% of people with lumbopelvic pain also had either pelvic floor pain or pelvic organ prolapse upon digital examination! Some people had pain, some people had weakness, some people had both.
“Just do Kegels” was the solution in the 80s, thankfully we know much more now and we know pelvic floor contractions alone are not the solution. An evaluation with a skilled pelvic floor physical and occupational therapists will help people identify musculoskeletal impairments and a treatment plan for home and in the clinic to address them.
Even though people may experience the exact same symptoms the underlying causes of them are often different. There is no one-size-fits-all approach to pelvic health!
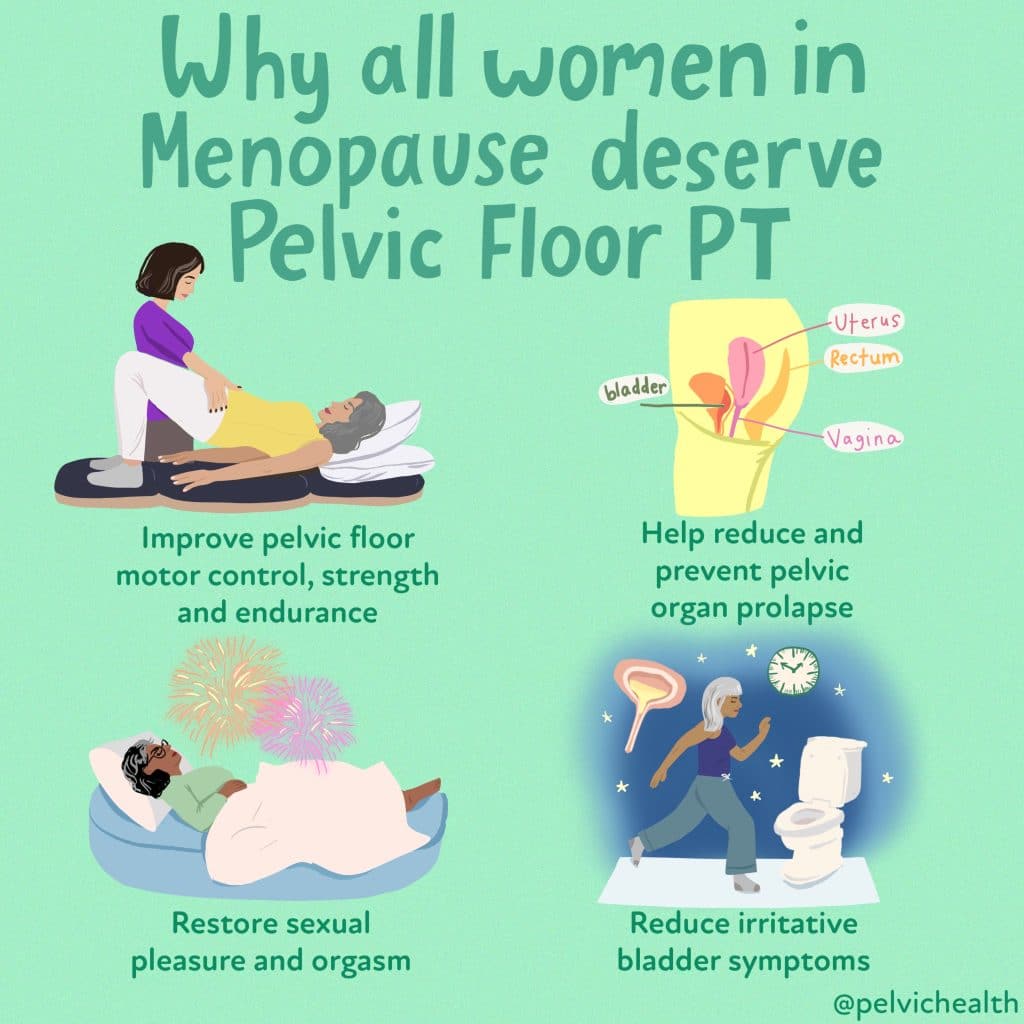
Understanding the Impact of Menopause on Pelvic Health
Menopause can significantly impact pelvic health, leading to conditions such as urinary incontinence, pelvic organ prolapse, and sexual dysfunction. The reduction in estrogen levels can cause the pelvic floor muscles to lose elasticity and strength, making them less supportive of the organs they cradle.
The Role of Pelvic Floor PT
Pelvic floor PT is a specialized form of physical and occupational therapy that focuses on strengthening the pelvic floor muscles and relieving associated symptoms. It involves exercises designed to improve muscle function, flexibility, and endurance. The therapy also includes education about lifestyle modifications that can support pelvic health.
The Benefits of Pelvic Floor PT in Menopause
-
Improved Bladder Control: Pelvic floor PT can help manage urinary incontinence, a common issue in menopause, by strengthening the muscles that control urination.
-
Reduced Pelvic Pain: Regular pelvic floor exercises (as prescribed by your pelvic floor pt) can alleviate discomfort caused by pelvic organ prolapse or sexual dysfunction.
-
Enhanced Sexual Function: A functional pelvic floor can improve sexual satisfaction by increasing sensation and reducing pain during intercourse.
-
Prevention of Future Issues: Even if you’re not currently experiencing pelvic floor issues, PT can be a proactive measure to prevent potential future problems.
Every one going through menopause deserves to live their life to the fullest, unburdened by pelvic health issues. Pelvic floor PT can be a powerful tool in managing the changes that come with menopause. It’s never too late to start – your pelvic health is worth it.
Remember, everyone’s journey through menopause is different, and so are their pelvic health needs.
Resources:
Want to read the study we referenced?
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.