By PHRC Admin
Interstitial Cystitis/ Painful Bladder Syndrome is a treatable pelvic pain syndrome affecting roughly 12 million people in the United States alone. If it affects so many, what are the causes? We’re glad you asked! There’s many!
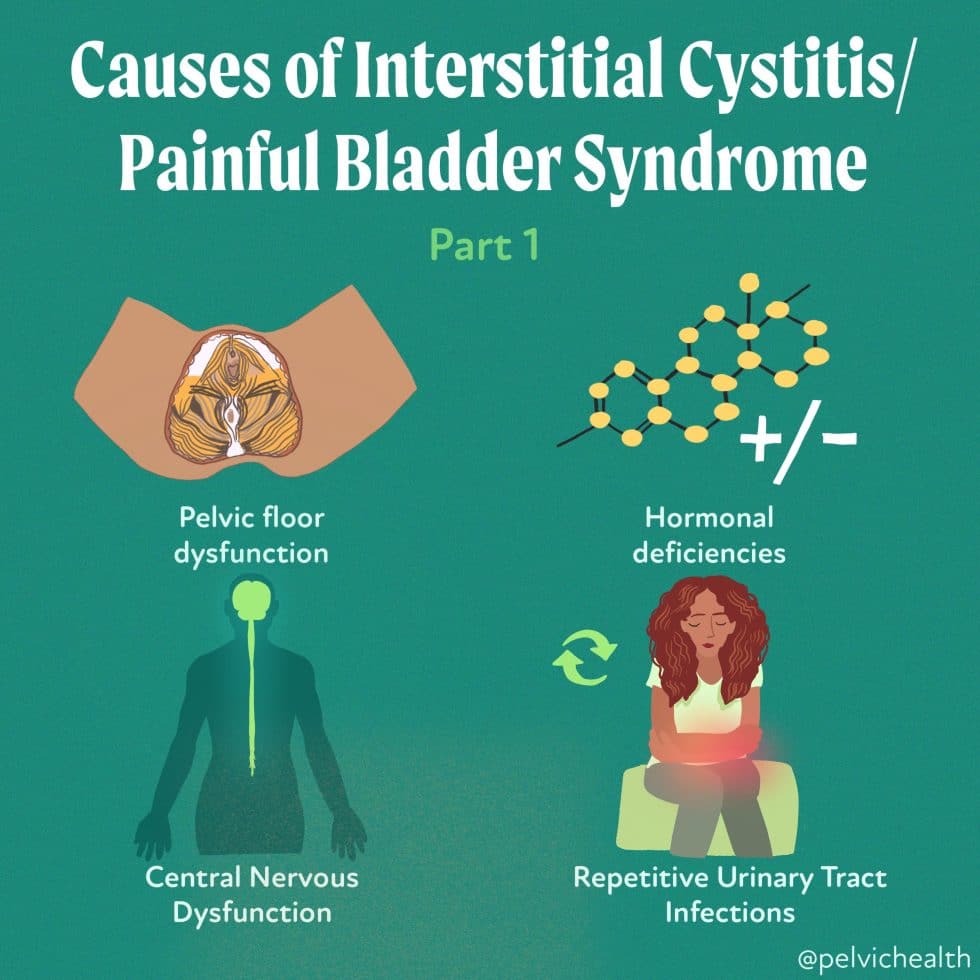
Pelvic Floor Dysfunction
Multiple studies conducted in the US and abroad show that up to 92% of people with IC/Painful Bladder Syndrome have pelvic floor dysfunction. The prevalence is so high that the American Urologic Association classified pelvic floor dysfunction as a phenotype, or subset, of IC in 2022.
Hormonal Deficiencies
Others may develop symptoms in response to hormonal deficiencies, which can occur from using oral contraceptive birth control bills, certain prescription acne medications, while breastfeeding, or in perimenopause/menopause.
Central Nervous Dysfunction
Some people have central nervous system sensitivities and experience body-wide pain and the symptoms of IC. CNS is another subset, or phenotype of IC.
Repetitive UTIs
Some people develop IC symptoms after a series of culture-proven UTIs, the symptoms can persist when the infection has cleared.
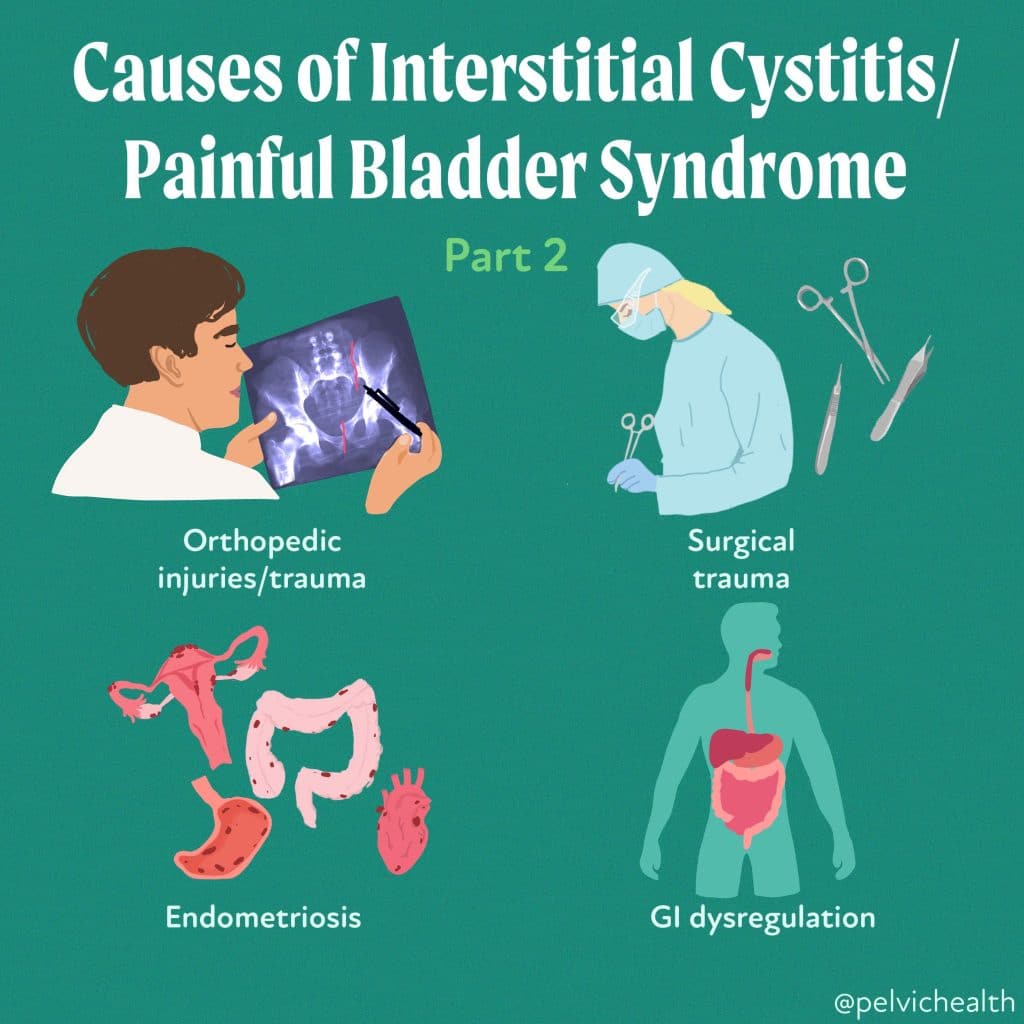
There is no one-size-fits-all treatment protocol for IC/PBS. Multimodal combinations of therapies are effective and can result in complete symptom resolution! Pelvic floor physical therapists are well-positioned to help patients organize their medical team and help patients make reasonable, strategic treatment decisions. The specific cause of Interstitial Cystitis is still not clearly known, but several factors have been identified that may contribute to developing this condition. One of these factors includes trauma to the bladder, such as from pelvic surgery or orthopedic injuries. There are many causes of IC/PBS, including:
- Orthopedic injuries/trauma
- Surgical trauma
- Endometriosis
- GI dysregulation
The symptoms of Interstitial Cystitis can range from mild discomfort to severe pain, which can be aggravated by certain foods or drinks such as coffee, soda, alcohol, tomatoes, hot and spicy foods, chocolate, caffeinated beverages, citrus juices and drinks, MSG, and high-acid foods (BCM). It’s important to consult with a healthcare provider if you suspect you may have Interstitial Cystitis or if you experience persistent bladder pain or discomfort, especially if these symptoms coincide with a history of bladder trauma or orthopedic injuries.
We understand that IC is commonly seen in people with vulvodynia, endometriosis, and fibromyalgia. Understanding the underlying cause/causes is part of what we work to figure out during pelvic floor physical therapy.
______________________________________________________________________________________________________________________________________
We are excited to announce our physical therapist, Molly, is now located in our 11th location in Columbus, OH. Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Melissa Patrick is a certified yoga instructor and meditation teacher and is also available virtually to help, for more information please visit our therapeutic yoga page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!