By PHRC Admin
Welcome 2024, goodbye 2023! It’s been another year full of changes for Pelvic Health and Rehabilitation Center. With the start of the new year, we would like to acknowledge all of the changes that have occurred both virtually and in person.
Last year…..
- PHRC Walnut Creek moved into a bigger, better space!
- PHRC Ohio opened in September 2023, bringing the number of PHRC locations to 11!
-
- We welcomed many new faces to the PHRC team!
- Cambria Oetken, PT, DPT – Westlake Village
- Jillian Farren, PT, DPT – Los Angeles, CA
- Danae Narvaza PT, DPT – Encinitas, CA
- Tiffany Vo, PT, DPT– San Francisco, CA
- Daniela Vinski – Pasadena, CA Administrative Assistant
- Jacob Berg– Lexington, MA Administrative Assistant
- Amanda Baker– Merrimack, NH Administrative Assistant
- Wendy Rosas – Encinitas, CA Administrative Assistant
- Aurora Pancoast – Walnut Creek, CA Administrative Assistant
- We welcomed many new faces to the PHRC team!
Social Media Expansion and Engagement
- With our ever increasing audience, we wanted to share some wins through social media! Our Youtube channel surpassed the 11k subscribers mark, our Instagram page flew over 46k followers, and recently our Tik Tok hit 9k followers, Twitter soared over 7k followers, LinkedIn almost hit 1.5k followers and our Facebook almost doubled in followers from 8k to 14k followers! We thank you for your support and for helping us spread the word about pelvic floor physical therapy and pelvic health!
We were featured as guests on quite a few podcasts!
- iCareBetter: Endometriosis Unplugged– Jandra Mueller began a partnership with iCareBetter starting their podcast where they dive deep into the world of endometriosis, sharing personal stories, expert insights, and practical advice for better care.
- Our confounder, Stephanie Prendergast, was interviewed by The Vagina Coach, Kim Vopni on her podcast – Between Two Lips. She was also interviewed by Samantha Cohen, cofounder of Femme Farmacy, in an episode titled, Pelvic floor Physical Therapy and A PT’s Central Role in Navigating Pelvic Pain.
We were featured as guests on quite a few blogs!
- Our cofounder, Elizabeth Akincilar, was featured in Insider Magazine:
- Stephanie was also featured in a LA Times article; ‘Just do kegels’ is tired. What’s next for this hot women’s health market?
- As The Pelvis Turns featured a guest blog from the Tight Lipped Community; Tight Lipped: You’re Not Alone; Patient-Led Communities
PHRC continues its partnerships in helping The Jackson Clinics Foundation in fundraising efforts to create a two year degree specializing in Pelvic Health! You can read more about it on our blog!

We celebrated our 17 year anniversary! Yes, you read that right! Check out our timeline below:




- We were a part of numerous education seminars!
- PHRC’s Jandra Mueller started the year off by co-hosting with Britt Gosse-Jesus, DPT, a 2-day live-online course hosted by Pelvic Health Solutions which is open to ALL healthcare providers who are interested in how to provide better care for those who suffer from endometriosis;
- PHRC’s Jandra Mueller taught an Endometriosis course hosted by Pelvic Health Solutions in November and December of 2022.
- Jandra and Stephanie were two panelists at the ISSWSH Fall Course October 2023
- PHRC’s Molly Bachmann hosted PHRC’s first ever workshop:
- Preparing your body for birth and postpartum: A Workshop for pregnant people that goes beyond kegels and “what to expect when you’re expecting”
- We started a new Instagram Live series with other specialists!
- Mondays with Molly
- First guest: Erin Pritchard, MA, LPCC-S, Founder of Sea Glass Ohio discussing the topic of The relationship between Purity Culture and Pelvic Health.
- Mondays with Molly
The Year of the Dragon!
We are continuing to build and expand our virtual services;
Our pelvic floor physical therapist, Molly Bachmann, continues to offer Peripartum Pelvic Floor Physical Therapy virtual appointments for:
- Birth preparation
- Birth planning
- Postpartum planning
- Birth & Postpartum education
- Exercise Considerations & more!
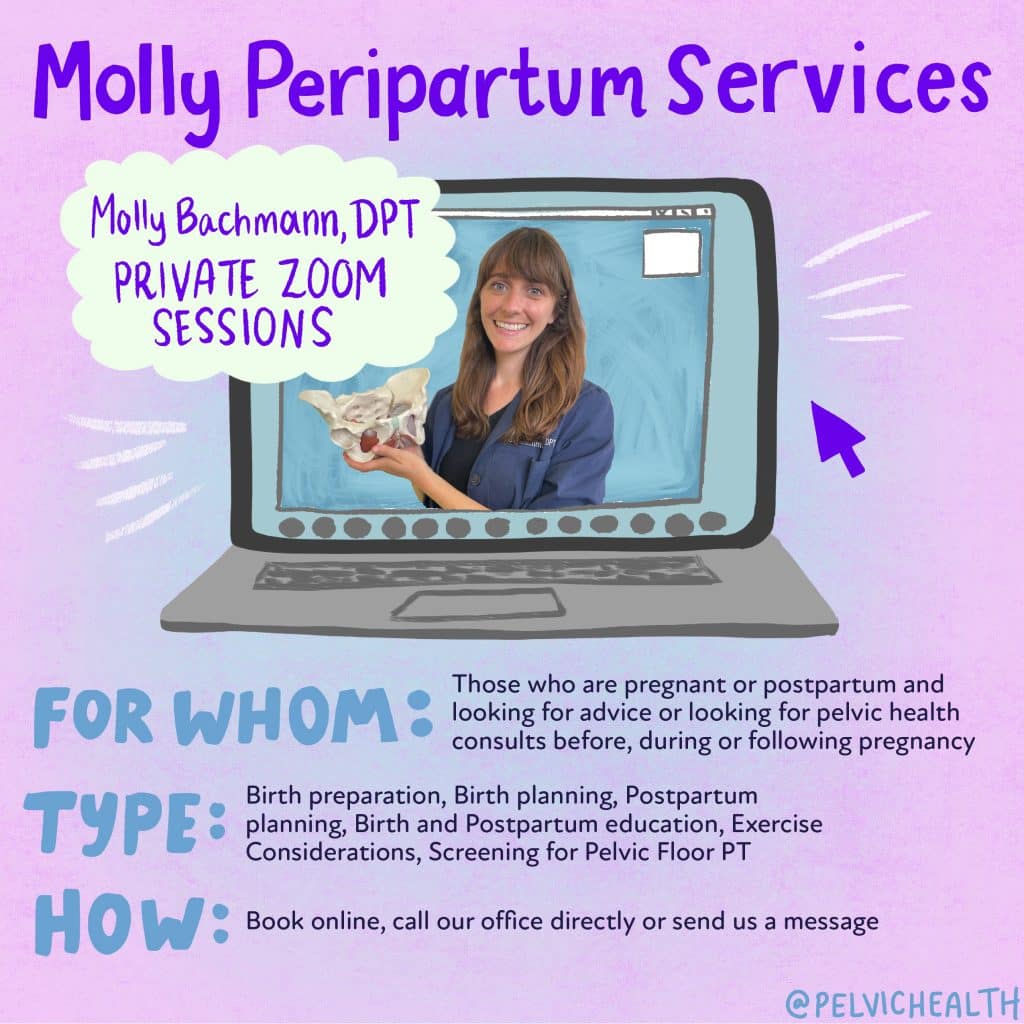
You can read more and book via our website for these services.
As we close out another year, we want to take a moment to reflect on the progress we’ve made in raising awareness about pelvic health. We’ve delved into critical topics, shared inspiring stories, and provided resources that have hopefully empowered many of our readers. Through it all, our goal has remained constant: to break down the barriers of silence and stigma around pelvic health.
Looking forward to 2024, we’re excited to continue this important conversation, bring you more enlightening content, and further our commitment to promoting pelvic health for all. Thank you for joining us on this journey – here’s to a healthier, stronger new year!
______________________________________________________________________________________________________________________________________
We are excited to announce our physical therapist, Molly, is now located in our 11th location in Columbus, OH. Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Melissa Patrick is a certified yoga instructor and meditation teacher and is also available virtually to help, for more information please visit our therapeutic yoga page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!

