By Stephanie A. Prendergast, MPT, Cofounder, PHRC Los Angeles
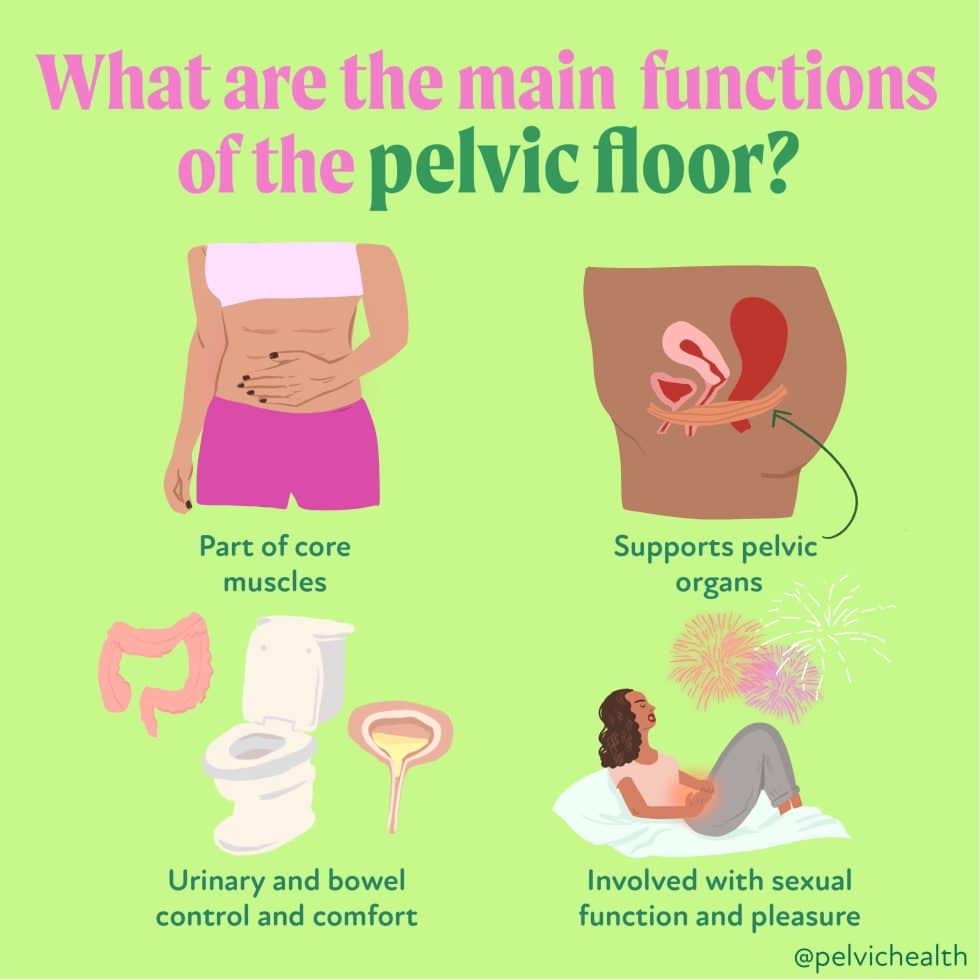
To start, there are various functions we can thank our pelvic floor, but let’s get into the MAIN functions:
Part of core muscles
The pelvic floor supports your core muscles: transversus abdominis, rectus abdominis, and the external oblique muscles. The PFM tends to act reflexively when we’re using our core under normal circumstances.
Supports pelvic organs
The pelvic floor muscles run from your pubic bone back to your tailbone. They support your pelvic organs and are also responsible for urinary bowel and sexual function.
Urinary and bowel control and comfort
As your bladder fills, the pelvic floor muscles will tighten so you don’t leak urine. As gas or stool enters the rectum, the pelvic floor muscles tighten so you don’t lose control of your bowels. When you go to use the restroom you naturally relax the muscles to initiate your urine stream.
Involved with sexual function and pleasure
When vulva owners, start to enter the arousal phase, muscles of this part the anterior pelvic floor start to contract and that allows blood flow to enter the clitoris and result in clitoral engorgement, as well as facilitating lubrication from our glands in the vestibule.
For those with a penis, most people can relate to the muscles also getting tight and they help to keep blood flow in the penis, which results in erection. As one goes through the sexual response, they start to get closer to orgasm, and when people have an orgasm the muscles of the pelvic floors are rapidly contracting to result in ejaculation for some, and sexual pleasure for all.
Fun fact: During an orgasm, the pelvic floor muscles contract up to 64 times in a minute!
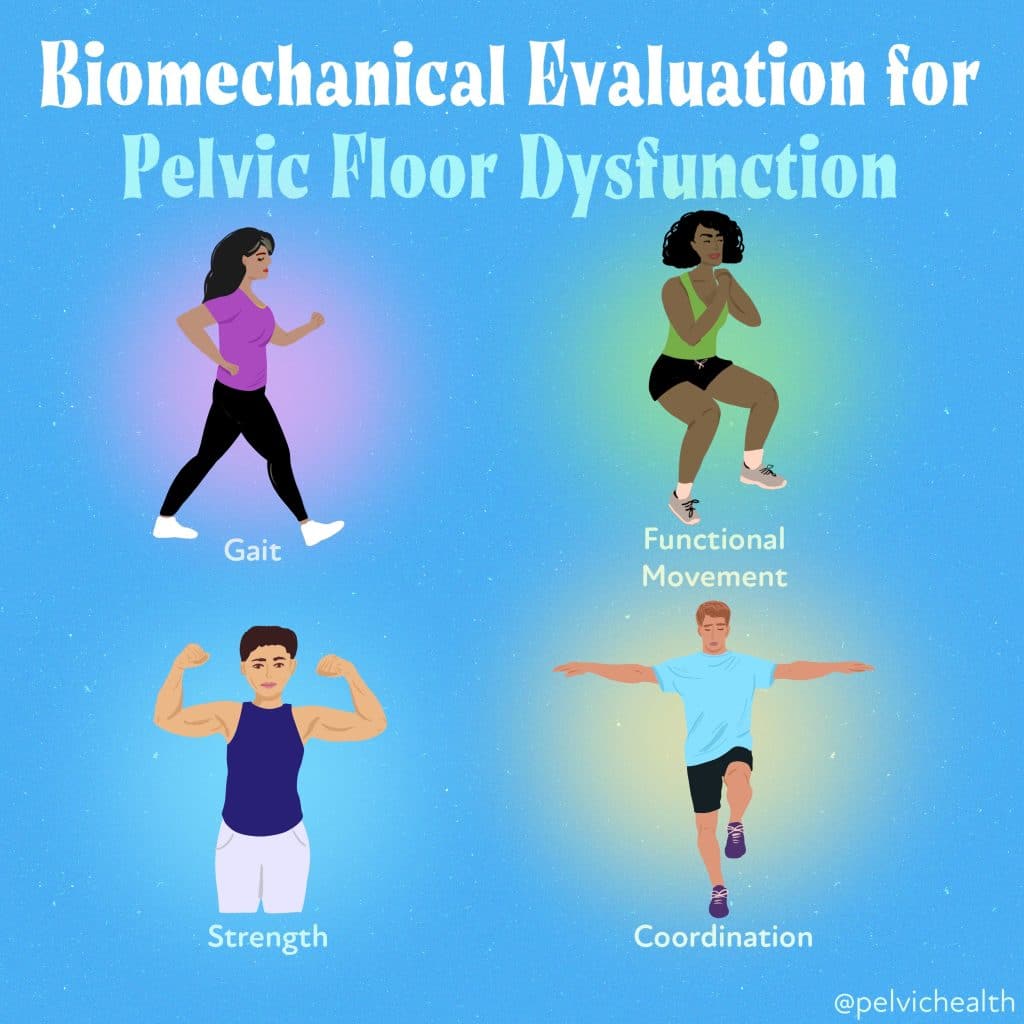
A common misconception about the pelvic floor is that it works in isolation. However, the pelvic floor works with the back, the abdomen and the hips, and is reliant on healthy joints above and below to function at its maximum capacity.
The pelvic floor is a DYNAMIC stabilizer and is the first set of muscles to turn on when we initiate any movement. This helps to keep us upright and to keep us from falling over. Therefore, a complete pelvic floor assessment will almost always involve analyzing your functional movement patterns at some point in the process.
We need our pelvic floor when we are walking, squating, balancing etc.!
Many people may have symptoms that occur in the pelvic floor. But as we often see, sometimes the pelvic floor muscles actually are functioning very well! It’s that the individual’s back, hips, knees, ankles . . . sometimes even their toes, do not support the body in the way that they should, which leads to compensatory movement patterns.
Having a biomechanical assessment can help us identify the root cause of your symptoms! Drop your questions in the comments below!
______________________________________________________________________________________________________________________________________
We are excited to announce Molly will be helping PHRC open their 11th location in Columbus, OH in September of 2023. Join the waitlist and be the first to be contacted!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical therapists via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Melissa Patrick is a certified yoga instructor and meditation teacher and is also available virtually to help, for more information please visit our therapeutic yoga page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!