
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
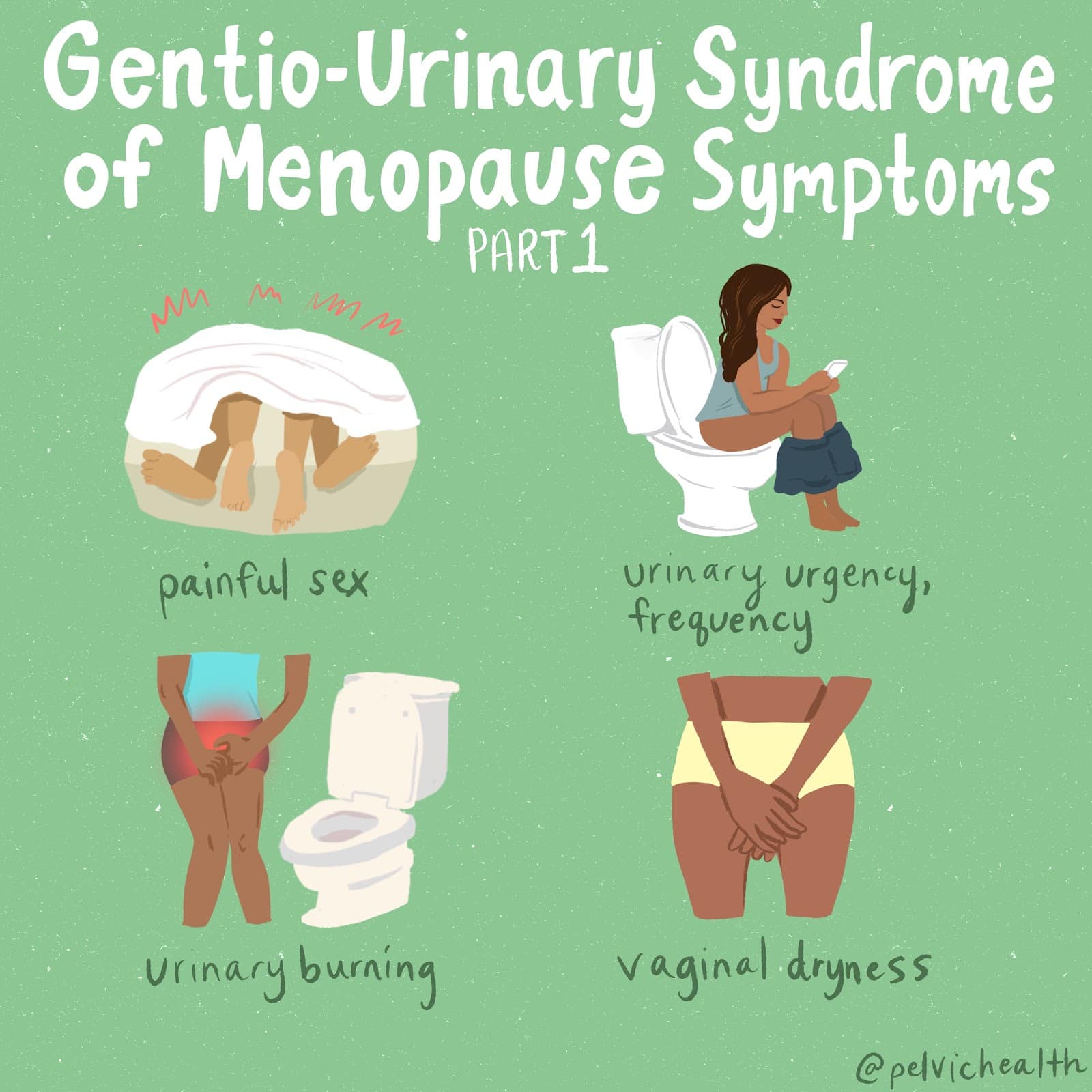
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
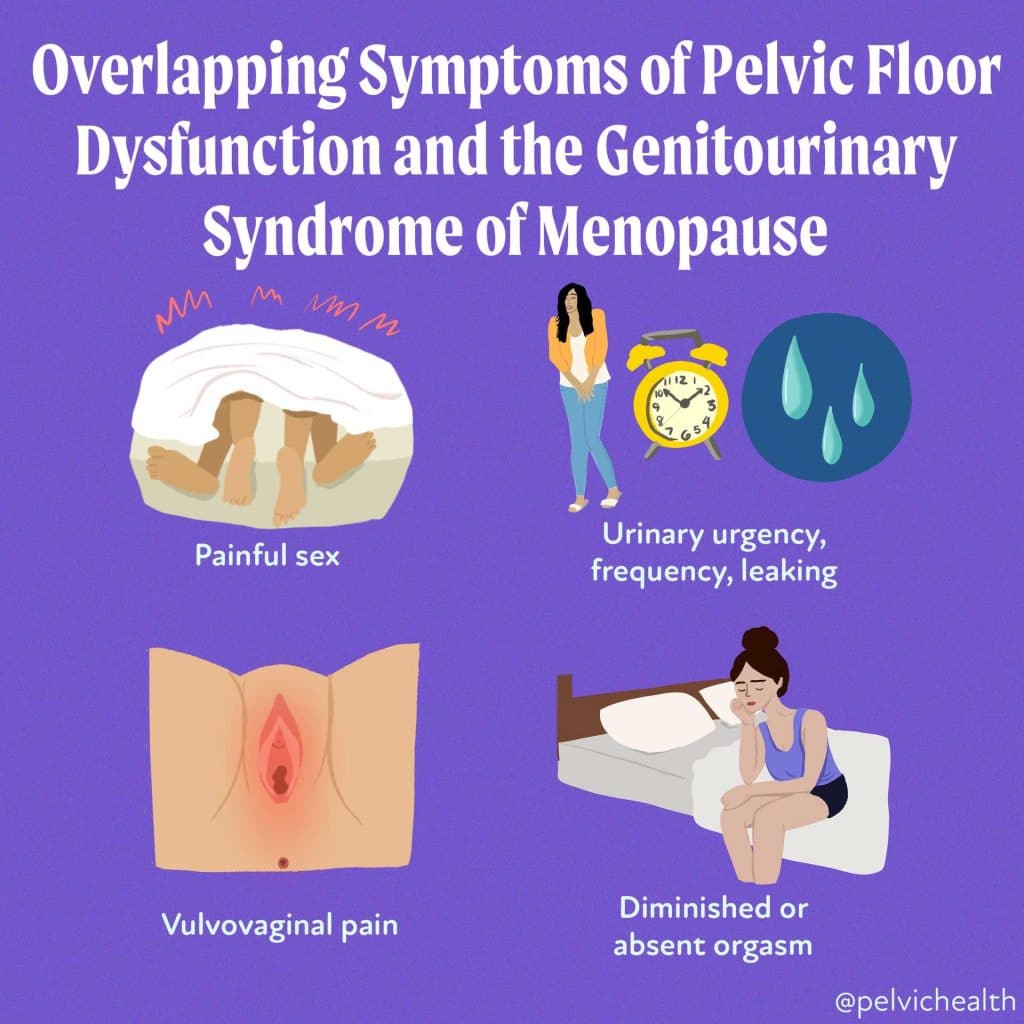
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting
An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.
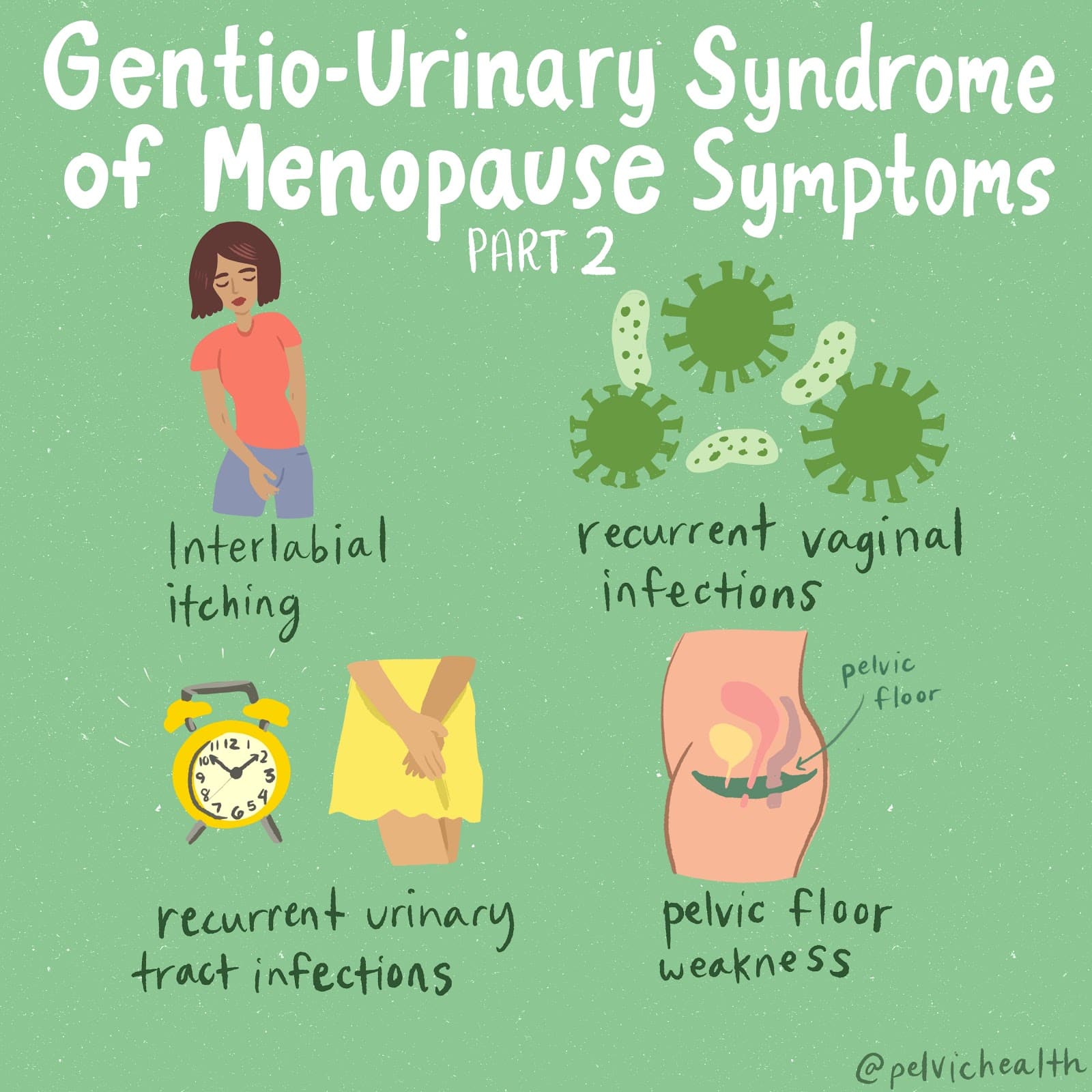
Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
Last week our staff attended the 2014 Annual Meeting of the International Pelvic Pain Society (IPPS) in Chicago. During its nearly 20-year existence the IPPS has been a major driver of the progress made in the treatment of chronic pelvic pain. And what makes the Annual Meeting of the organization so exciting is that it provides an opportunity for our community of providers to take stock, to determine where we are and where we still need to go in our quest to provide the best treatment for our patients.
Take a look a few of these must-read nuggets from the conference!
Malinda heard Dr. Afton Hassett give a wonderful presentation titled The Role of Resilience in Chronic Pain. In her presentation, Dr. Hassett discussed the nature of pain and that pain is processed by many areas of the brain and not solely the somatosensory cortices. Pain can be sensory, emotional and cognitive. Sensory pain is what most of us are aware of. An example is when you place your hand over a hot flame. An example of emotional pain is going through a breakup.
In one study referenced by Dr. Hassett, researchers found that when a person goes through a breakup the sensory and emotional parts of the brain are both activated. The conclusion: thoughts and emotions are processed by similar parts of the brain.
Dr. Hassett discussed her research on the affects of negative and positive emotions with regard to pain. She has found that negative emotions can contribute to the following: higher pain intensity, lower pain tolerance, worse weekly pain, greater use of pain medication, increased fatigue, more physical symptoms, and poor quality of life.
Dr. Hassett stated that patients who have positive emotions have a higher tolerance to pain, decreased pain intensity, decreased same day pain report, decreased use of pain medication, and a longer life span.
Dr. Hassett acknowledged the difficulty of staying positive while experiencing pain. She recommends one or more of following interventions to help stay positive:
- Keeping a gratitude diary: Write down three things daily that you are grateful for. The three things must be different each day. Smile as you write these things down, which will help you feel grateful.
- Gratitude visit: Think of people in your life who have been kind to you, but have never heard you express your gratitude. Write a gratitude letter to one these individuals, describing why you are grateful. Name specific events or things they did for you and how it has affected your life. Make an appointment with the individual and read the letter out loud to them. Discuss how both of you feel about each other, the letter, and the future.
- Three good things: Before bed write down 3 good things that went particularly well that day. Next to each positive event, answer the following questions, “Why did this good thing happen?”
- Intentional Kindness: Everyday do one intentionally kind thing for a loved one, a complete stranger, and yourself. Look the person in the eye and be gracious. Expect nothing in return, however acknowledge the gratitude if offered by the other person. When you intentionally offer one kind thing to yourself, acknowledge the importance of self-care and kindness. Log these acts in a diary and take note what the kind act was and how it made you feel.
- Savoring a beautiful day: Block time off on your schedule for at least one hour, up to eight hours for your own pleasure. Plan one or a sequence of activities that brings you real pleasure. Savor each activity using all your senses and with feeling of gratitude.
Casie also commented on Dr. Hassett’s lecture. As PHRC’s resident Yogi, she had some interesting insights!
As a physical and occupational therapists and a yoga teacher I often find myself wearing two different thinking caps as I try to find balance between western medicine and more yogic principles in my treatment of patients with chronic pelvic pain. Often times these two worlds don’t overlap so I was pleasantly surprised when Dr. Hassett asked participants at this year’s IPPS conference to take part in an exercise I have practiced many times in yoga workshops.
Dr. Hassett asked this very serious group of health care professionals to stop and take a moment to make eye contact with the person sitting next to them, smile at them, and then say something kind to them. As you can imagine there was an uncomfortable unfamiliarity and awkwardness at first, however there was a palpable shift in the mood in the conference hall after just 3 minutes of kind exchanges and deliberate personal connection.
Dr. Hassett’s point was this; that positive affect is a positive predictor in patient’s reported pain levels, health outcomes, and sense of well-being.
As clinicians working with patients with chronic pelvic pain we are well equipped with the pharmaceuticals, nerve blocks, surgeries, etc. that our patients often unfortunately require at times. It was nice to hear that Dr. Hassett was reminding us as clinicians that we have more tools to serve these patients are using a biopyschosocial approach, something that was a common thread throughout many lectures at IPPS. The exercise mentioned above was an example of an intervention that could increase resilience, a quality that has been found in the research to play a role on positively impacting positive affect. We want this in our patients!
Dr. Hassett cited a long list of studies throughout her talk linking positive affect in patients with lower overall pain ratings, decreased induced pain sensitivity, decreased use of pain medication, and longer tolerance to pain. She cited data that linked decreased positive emotions in patients with chronic pelvic pain (Hassett et al. Reg Anes Pain Med 2012;37:398-402) and emphasized the need to boost resilience as a way to combat pain.
Another study performed on a group of patients recovering from Lyme disease showed that positive affect was the “only significant predictor of persistent symptoms” (Hassett, results not yet published). With such a direct correlation and positive predictive power it makes sense that we as clinicians promote these qualities that have the potential to help our patients in a way that surgery and injections might not.
Dr. Hassett has inspired me to wear new kind of thinking cap as I go back into the clinic this week; one that blends both evidence-based practice and classic yogic philosophies promoting psychological well being. I’m excited to get back to the clinic and start sharing these findings with my patients.
Great job Malinda and Casie! It was so interesting to read what you each took away from the presentation, which was a true highlight of the conference!
For her part, Melinda heard Carolyn Vandyken, PT speak about integrating central sensitization into clinical practice. She began by differentiating acute and persistent pain and how persistent pain involves the central nervous system and is often multifactorial. She highlighted the fact that pain cannot be removed without leaving a change in the person. She concluded by discussing treatments aimed at the central nervous system and shared with us a powerful short animation from Dr. Brené Brown of the RSA called The Power of Empathy, http://www.thersa.org/events/rsashorts/the-power-of-empathy
And Stacey heard Jennifer Gunter, MD speak about interventional procedures for chronic pelvic pain. Dr. Gunter believes that the key principles to pain management for chronic pain are first and foremost patient self-care and then as well medical management, physical and occupational therapy, interventional procedures, and mental health care. She focused primarily on the procedure component during her lecture. She described that the benefits from procedures are often not a cure but can bring about temporary improvements that can help with improved mobility, reduce central sensitization, and improve ability to perform physical and occupational therapy. Examples of procedures are trigger point injections, nerve blocks, radiofrequency, and Botox injections.
Stay tuned next week for the second half of our conference coverage when, among others, Allison discusses Dr. Andrew Goldstein’s controversial lecture and Stephanie give us the low down on Dr. Jeannette Potts’ talk aptly titled “The Problem is NOT the Prostate!”
Did you attend the conference this year, what did you think? Are there any topics above that you’d like to read about more in depth on our blog? Let us know!
All our best,
The PHRC Team
At PHRC we treat a wide variety of patient populations. One population that we’re beginning to see more often is patients undergoing treatment for anal cancer.
Recent research has shown that the incidence of anal cancer, which is linked to the human papillomavirus (HPV), is on the rise, especially among men and women under the age of 45.
Although we’re seeing more of these patients, they remain highly underserved when it comes to physical and occupational therapy. That’s because many physicians and patients simply are not aware of the help that physical and occupational therapistss, specifically pelvic floor physical and occupational therapistss, can offer.
Thus, I’ve decided to write this blog, which gives a complete overview of how pelvic floor PT can help anal cancer patients.
Anal cancer is a malignancy that starts in the anus, the opening at the end of the rectum. The American Cancer Society estimates that 7,210 cases will be diagnosed in 2014. The good news is that when detected early, anal cancer is usually curable. This page on the website of the Anal Cancer Foundation is one of the best sources of information on the disease.
Anal cancer is typically treated with combined chemoradiation therapy, and even in early diagnoses, treatment can often have serious and difficult side effects.
Patients who receive local radiation to their pelvis and anus, for example, may suffer from long-term fatigue, gastrointestinal, and sexual health dysfunction. In addition, in women, treatment may result in vaginal stenosis, which is the narrowing of the vagina due to scar tissue formation, and anal stenosis, often rendering sexual activity extremely painful. For men, it cause erectile dysfunction and anal stenosis.
Fortunately, pelvic floor PT can help with these side effects, as well as with the following:
- hip pain and/or pelvic pain, patients will often say that they feel as though they’ve lost range of motion in their hip/pelvis;
- surgical pain if there is a surgery;
- fatigue, which can be a short-term or long-term effect;
- lymphedema, which is localized fluid retention due to a compromised lymphatic system;
- general musculoskeletal impairments, such as overall weakness, neuropathy or just general deconditioning;
- pelvic floor dysfunction, which includes, in addition to the above-mentioned issues, gas and fecal incontinence, urinary symptoms, such as hesitancy or a weak urine stream;
- and scar tissue due to radiation burns.
PT can Help
I believe there is a big role that physical and occupational therapy can play in the management of the above-mentioned side effects. While there is not much research literature to support this, we’ve seen very good clinical evidence that indicates pelvic PT is worth the time and resources for patients.
So exactly how can PT help?
For one thing, many patients experience musculoskeletal pain as a result of treatment, typically in the pelvic area. Even areas of the pelvis that haven’t been radiated can be affected due to radiation of nearby tissue. To be sure, the pelvic floor can act as a veritable house of cards, where one problematic area can cause issues to adjacent areas. Thus, manual therapy techniques such as myofascial trigger point release, connective tissue manipulation, scar mobilization, and joint mobilization can treat the affected tissues.
For pelvic floor dysfunction caused by stenosis of the anus and/or vagina, manual therapy can help to maintain the openness of the organ. Patients with stenosis also need to be placed on a dilator program that ensures progress continues outside of treatment. A PT can help patients learn how to use dilators, and monitor their progress.
Another pelvic floor-related issue that can occur as a result of cancer treatment, is gas and/or fecal incontinence. This is because radiation therapy can damage the integrity of pelvic floor tissues, which can in turn cause a laxity in the muscles that results in uncontrollable gas, or a loss of bowels. There may also be a situation where tissue such as the external sphincter, must be removed.
For its part, pelvic floor rehab can help to strengthen any affected muscles by using techniques such as biofeedback, patient education, and/or neuromuscular electrical stimulation. That said, although gas and fecal incontinence are dysfunctions that pelvic physical and occupational therapy can help to decrease, I should make it clear that we can’t always completely cure these issues.
When it comes to overall function, patients often feel that their body has significantly changed as a result of having endured incessant pain or fatigue. Many patients that I have treated feel as though they’ve lost mobility, strength, or their muscles have been deconditioned as a result of lack of use. As PTs, we can help to recondition patients by working to correct their posture, sitting position, gait and walking, and by treating any lower back or hip impairments with manual therapy, neuromuscular reeducation, and patient-specific exercises.
Fatigue is a big issue for patients going through cancer treatment. And there is evidence to support that PT is a great tool that can help combat chronic fatigue. A therapist can help patients pace out their daily activities, and whenever possible, help them to resume physical activity. When it comes to a body in motion, we want to place patients on a program that combines aerobic, strengthening, stretching, and balance activities.
A final point that I’d like to mention pertains to lymphedema caused by cancer treatment. If for instance, lymphedema occurs in the groin area, pelvic floor rehab can manually drain the lymphatic system, and decrease symptoms like pain and swelling.
For any patient who is considering pelvic floor rehab, please be aware that it’s a good idea to receive clearance by your physician in order to start therapy. Additionally, like all other forms of therapy, it’s important to give PT a fair chance to make a difference. Meaning, this type of therapy requires at least a three to twelve month patient commitment. However, patients may not be required to come on a weekly basis.
If you have any questions about pelvic floor rehabilitation in the case of anal cancer treatment, please do not hesitate to leave them in the comment section below.
Postpartum pelvic floor rehabilitation is a big part of what we do at PHRC, and a major issue that we treat for new moms involves C-section scarring. In this post, we’re going to discuss the issues that can arise as a result of a C-section scar as well as how these issues can be addressed with the help of a PT.
As of 2012, 33% of births ended in C-section. (However, recently published guidelines were aimed at lowering that number.) “C-section” is short for cesarean section, and is the delivery of a baby through an incision in the mother’s abdomen and uterus.
These days the most common incision used for a C-section is the “horizontal” or “bikini incision.” The incision is cut through the lower abdomen at the top of the pubic hair just over the hairline. Scarring from the incision builds up underneath the incision as well as in the uterus.
Before we discuss the potential problems caused by a C-section scar, let’s first take a look at what scar tissue is.
Scar tissue is fibrous tissue that replaces normal tissue after an injury. It’s made of the same stuff as the tissue it replaces—collagen. However, the quality of the collagen is inferior to the tissue it replaces. Plus, the tissue is usually not as elastic as the original tissue. It’s important to bear in mind that the scar that you can see is actually only the tip of the iceberg as most scars extend deeper into the body than the bit of scar that is outwardly visible.
Now let’s take a look at some potential problems caused by a C-section scar.
A common complaint after a C-section is the sensitivity of the scar itself. For instance, it may hurt to lean over to pick up baby or may cause pain with lifting or other positional changes. Standing up straight may be painful as well as reaching over the head.
In addition, the scar may cause a slight postural change, a sort of “pulling forward” that along with a decrease in the support of the back from the abdominal muscles could result in back pain.
But the possible consequences don’t stop there. The scarring can cause the adjacent muscles to develop trigger points that refer pain to areas like the clitoris or urethra. In addition, the adjacent connective tissue can become restricted also causing pain. Lastly, the scarring can irritate superficial nerves in the area of the scar.
What’s more, the round ligament that attaches from the sides of the uterus to the labia can be caught in scar tissue after a C-section because the incision is also right over the area where the round ligament crosses the pelvic brim. If this happens, a woman can experience labial pain, especially with transitional movements like going from a seated position to a standing position.
Another symptom we have seen with our patients who have had C-sections is that they may have issues with lower digestion such as irritable bowel syndrome or constipation. This occurs because of the tightening created by the scar tissue pulls within the abdominal cavity and thus affects the organs.
The good news is that the problems caused by a C-section scar can be treated with pelvic floor physical and occupational therapy. So how does a physical and occupational therapists treat a C-section scar?
Most problems caused by C-section scarring can be improved or corrected altogether by making the scar more flexible by manipulating the scar tissue. The more scar tissue is moved and massaged, the softer and more similar to the tissue around it it becomes. This reduces tightness and breaks up adhesions (an “adhesion” occurs when scar tissue attaches to a nearby structure).
So if a scar is pulled in all directions, the body will lay down the fibers of the scar tissue with more organization, and in a similar alignment to the tissues around it. This results in the scar blending in better and behaving more like normal tissue.
What this means during your PT treatment is that the therapist will massage and manipulate your C-section scar and the area around it. Scars (internal and external) can be pushed, pulled, pinched, rolled, and rubbed. (Warning: manipulating a scar can be painful. That’s because tissue that has restricted blood flow is super-sensitive to touch, so treatment can be painful.)
But, this is a pain that comes with gain. Ultimately, scar mobilization promotes collagen remodeling, which increases pliability of the tissues and reduces uncomfortable sensations, such as itching or sensitivity.
It’s best to start C-section scar mobilization early in the healing process, usually six to eight weeks after the procedure. The reason that early intervention is ideal is because the tissue will respond quickest during this period.
However, the body remodels scar tissue constantly, so your tissues are being replaced with new tissue all the time, just at a much slower rate when scar tissue is older. A PT can also instruct a new mom on how to perform the mobilization at home if appropriate.
Pelvic floor physical and occupational therapy is helpful for all postpartum women regardless of how they delivered their baby. Read more about it in Cosmo magazine and our follow-up post here.
If you have any questions about C-section scarring, please leave them in the comment section or email to [email protected].
————————————————————————————————————————————–
Are you unable to come see us in person? We offer virtual appointments!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical and occupational therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical and occupational therapistss committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. The cost for this service is $75.00 per 30 minutes. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.




