
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Menopause encompasses more than just hot flashes, night sweats, and mood swings. Despite being a common phase affecting roughly half of the population, menopause is often misunderstood, both by the public and many healthcare providers. This gap in knowledge can lead to unnecessary suffering, as many individuals are not fully informed about effective treatments.
Perimenopause, the transitional phase leading up to menopause, typically begins in a person’s 40s, with menopause itself usually occurring in the early 50s. While systemic symptoms like hot flashes and mood changes are well-known, many people also experience less obvious but equally impactful genitourinary symptoms. These can include painful intercourse, urinary urgency, frequent urination, leakage, burning sensations, recurrent vaginal and urinary tract infections, and vaginal dryness. Collectively, these symptoms are part of the Genitourinary Syndrome of Menopause (GSM). Additionally, many women experience pelvic floor dysfunction, which affects nearly 50% of women by their 50s and can overlap with GSM symptoms.
While systemic hormonal therapy is commonly used to manage menopause symptoms, it may not address the specific needs of those experiencing GSM. The North American Menopause Society recommends the use of vaginal estrogen as an effective treatment for alleviating GSM symptoms and improving quality of life.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and Genitourinary Syndrome of Menopause (GSM) can overlap and include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An experienced healthcare provider, whether a pelvic floor physical and occupational therapists or a medical doctor, can conduct several assessments to diagnose pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. These evaluations include a vulvovaginal visual examination, a Q-tip test to pinpoint areas of pain, and a digital manual examination.
Without appropriate medical management, all women may eventually experience symptoms of Genitourinary Syndrome of Menopause (GSM). Many are unaware that a pelvic floor physical and occupational therapy evaluation can be highly beneficial for addressing the musculoskeletal issues contributing to their discomfort. Combining pelvic floor physical and occupational therapy with medical treatments can be crucial for improving sexual enjoyment and resolving urinary and bowel problems.
Virtual pelvic floor therapy for menopause—contact us to get started!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- Every day, approximately 6,000 women reach menopause.
- In the United States, around 50 million women are currently navigating menopause.
- About 84% of women experience genital, sexual, and urinary discomfort related to menopause, which often does not resolve without intervention, yet fewer than 25% seek assistance.
- An estimated 80% of OB-GYN residents acknowledge feeling inadequately prepared to address menopause-related issues.
- Genitourinary Syndrome of Menopause (GSM) is clinically identified in 90% of postmenopausal women, yet only one-third report experiencing symptoms in surveys.
- Barriers to treatment include women needing to initiate discussions about their symptoms, a belief that these issues are simply part of aging, and a failure to connect symptoms with menopause.
- Only 13% of healthcare providers routinely inquire about menopause-related symptoms with their patients.
- Even after a diagnosis of GSM, many women remain untreated. This is partly due to healthcare providers’ reluctance to prescribe treatments and patients’ concerns about the safety of topical vaginal therapies, despite evidence showing that GSM significantly affects quality of life.


Hormone deficiency can lead to itching in the labial and vaginal areas. Additionally, other dermatological conditions, such as Lichen Sclerosus and cutaneous yeast infections, should also be considered.
During menopause, individuals are particularly susceptible to frequent vaginal and urinary tract infections due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a major contributor to pelvic floor dysfunction. It’s crucial to address these infections promptly, as ongoing visceral-somatic input from untreated infections can lead to increased pain and further dysfunction even after the infection has been resolved. Without appropriate hormone therapy, infections may persist, leading to severe consequences. Untreated infections can cause unprovoked pain, make sexual activity difficult or impossible, and undiagnosed urinary tract infections (UTIs) may progress to kidney issues and other serious complications.
We recommend consulting with a menopause specialist to effectively monitor, prevent, and treat Genitourinary Syndrome of Menopause (GSM) since these issues are both significant and manageable. It’s important to normalize discussions about GSM; there’s no need for embarrassment. With appropriate care, individuals can lead fulfilling lives. Combining virtual pelvic floor physical and occupational therapy with medical management is essential for optimal results.
Treatment:
How We Can Help You

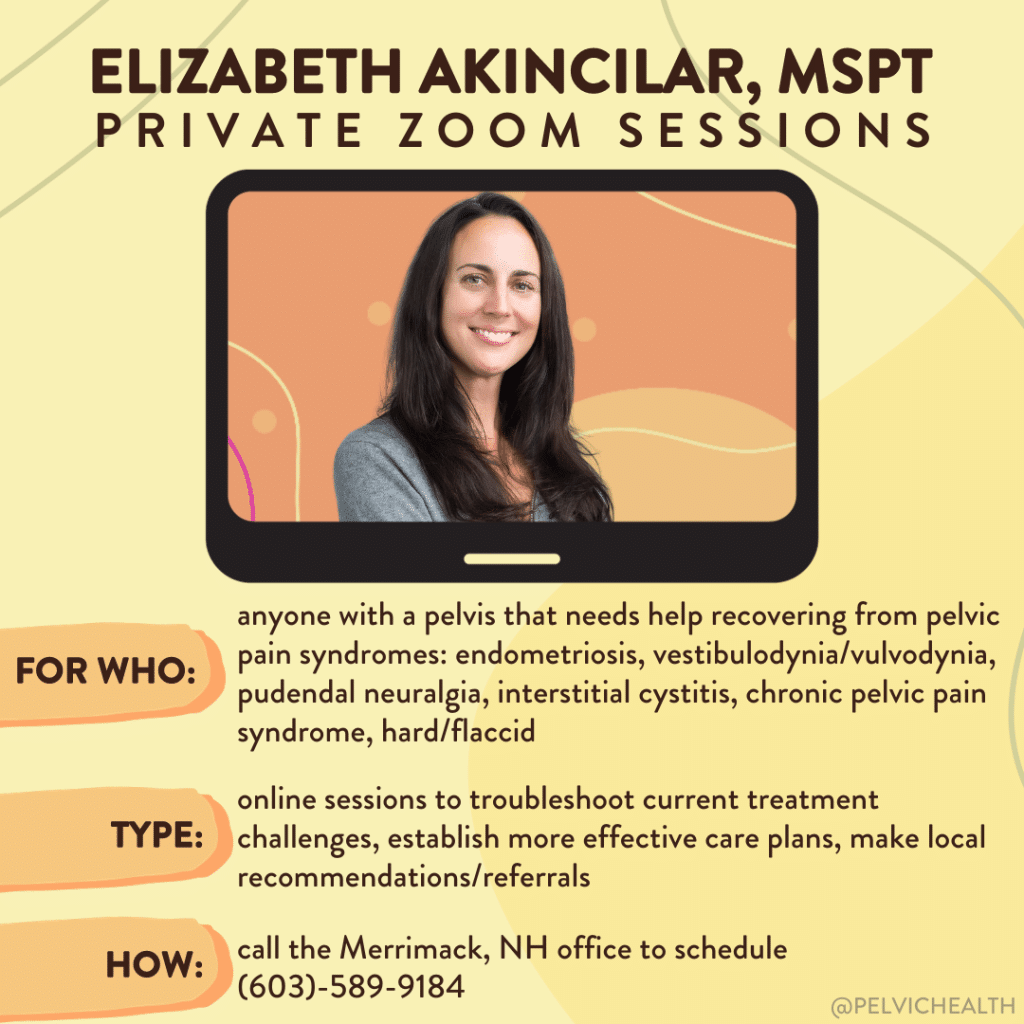
If you’re experiencing sexual dysfunction, it’s beneficial to consult a pelvic floor physical and occupational therapists online. They can assess whether any issues with your pelvic floor are contributing to your symptoms. During your initial virtual evaluation, the therapist will review your medical history, including previous diagnoses, treatments, and their effectiveness. They understand that many patients feel frustrated by the time they seek help.
The therapist will examine your nerves, muscles, joints, tissues, and movement patterns. After the assessment, they will discuss the findings with you and set both short-term and long-term therapy goals. Typically, physical and occupational therapy sessions occur once or twice a week over a period of approximately 12 weeks. Your therapist will also coordinate with other specialists on your treatment team and provide you with a personalized home exercise program. Our goal is to support your recovery and help you achieve the best possible quality of life.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
Get virtual pelvic floor therapy for menopause. Book your online consultation today!
By Elizabeth Akincilar, MSPT, Cofounder, PHRC Merrimack
The pelvic floor plays a significant role in several crucial functions, including bowel health, sexual function, and balance. However, certain common habits and misconceptions can lead to pelvic floor dysfunction. Did you know we were featured in an Insider magazine article? Let’s review these common mistakes and hopefully give you a few ways to avoid them in the future!
Here are some key points to remember:
Breath-holding during workouts
This common mistake can cause the pelvic floor to tighten, leading to sexual dysfunction and problems with urination and bowel movements. Holding your breath during activities like lifting heavy objects or exercising can increase pressure on the pelvic floor muscles, potentially leading to pelvic pain. Focus on maintaining proper breathing techniques during physical exertion.
Part I: Breathing Techniques for Pelvic Floor Health
Part II: Breathing Techniques for Pelvic Floor Health
Check out our full Youtube playlist about Breathing Techniques.
Sedentary lifestyle
Sitting for extended periods can compress the muscles and nerves in the pelvis, triggering urinary tract issues and chronic pain in the pelvic and lower back area.
Unnecessary or incorrect Kegel exercises
Not everyone needs to do Kegel exercises. Doing them unnecessarily or incorrectly can over-tighten the pelvic floor, causing sexual dysfunction, frequent urination, or difficulty with bowel movements.
Poor dietary habits
Good pelvic floor and bowel health are closely linked to a diet rich in fiber and adequate water intake.
Incorrect pooping technique
Western toilet designs aren’t ideal for proper bowel movements. Using a toilet stool or elevating your feet can improve your pooping technique while reducing the daily chronic pelvic pain experienced.
Ignoring pelvic pain
Any pain or discomfort in the pelvic region should be evaluated by a medical professional. Whether or not you have had your pelvic pain diagnosed or not, getting your pelvic pain treated can greatly improve your quality of life. When you ignore your pelvic pain, it can develop into chronic pelvic pain, but help is out there! Whether or not your pelvic pain is manifesting as: menstrual cramps, ongoing pain, bladder issues, constipation, or other symptoms, treatment options are available. Your pelvic health matters!
Overlooking symptoms in menopause and postpartum
Menopausal individuals should not ignore pelvic discomfort, and postpartum individuals should seek help for any form of incontinence. Whether you have acute pelvic pain or not, PFPT can be a beneficial part of any care plan for those under this category.
Enduring severe menstrual pain
Debilitating menstrual pain is not normal and should be checked by a healthcare provider. High levels of pain related to the menstrual cycle should be taken seriously.
Posture
Maintaining pelvic health requires awareness and proactive measures, including maintaining good posture, practicing appropriate exercise techniques, and seeking timely medical care for any concerns. Your pelvic muscles will thank you for paying attention to them!
Frequently Asked Questions
Q: What does a pelvic floor physical and occupational therapy appointment entail?
A: Hi! To put it simply, a PFPT appointment starts with an evaluation of your health history, followed by both an external and internal exam. Pelvic floor pt appointments can involve a lot, so we didn’t want you to miss any information. Here is a short clip about what to expect, followed by this extensive blog about the initial appt/treatment plan!
Q: I can’t find a provider, or you are too far away
A: This directory might help you locate a provider near you. The providers on the listed are trusted specialists who can assist in treating chronic pelvic pain.
Q: How can I book an appointment with you?
A: Great question! There are various ways to do so. You can fill out your information here and we can get a hold of you. Or you can book a telehealth appointment here. OR you could call any of our offices (phone numbers here) and schedule an appointment directly.
Additional resources we recommend:
Hormonal Prepartum Changes and Postpartum Complaints
Embracing IBS Awareness Month: A Pelvic Floor PT Perspective
What to Know About Your Menstrual Cycle
Clinical Manifestations of Endometriosis
Our Educational Resources for Pelvic Pain
(Purchase a copy of it via our website)
Just a few podcasts of so many…
- iCareBetter: Endometriosis Unplugged
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Alexa Savitz, DPT, PHRC Pasadena
Meet Jackie!
Jackie, six months postpartum, came to PHRC experiencing heaviness, pressure, muscle spasms around the rectum, and pelvic pain near her right hamstring and sit bone. She had a vacuum-assisted vaginal birth and a Grade Two Perineal Tear. Despite being ‘cleared for activity’ at her six-week check-up, her pain persisted. After consulting a urogynecologist, she was diagnosed with Grade One Uterine Prolapse. Jackie mentioned that she tended to tighten her pelvic floor out of fear of prolapse symptoms. During our treatment, she was fitted for a pessary, which she rarely wore due to discomfort caused by the device. Before pregnancy, she was active in hiking and weightlifting. Now, she struggled to walk a mile without symptoms, experienced pelvic pain while lifting her baby, and found it difficult to stand and cook dinner at the end of the day.
Goals for Pelvic Floor Physical and Occupational Therapy
Jackie aimed to return to hiking with her baby, resume general exercise, and eliminate pain while standing and cooking.
Physical Examination
The physical exam revealed the following impairments:
- Reduced coordination of her deep core muscles and mild diastasis recti
- Increased pelvic floor muscle tension with painful palpation of the transverse perineal and levator ani muscles
- Reduced pelvic floor muscle strength and poor neuromuscular coordination
- Myofascial trigger points in the pelvic girdle and weakness in her gluteal muscles
- Vulvar tissue dryness, which is now called the GenitoUrinary Syndrome of Lactation* and is treated with topical vulvar estrogen
*A groundbreaking study has revealed that high prolactin levels during lactation can cause genitourinary symptoms like vaginal dryness and urinary incontinence in those postpartum. This research sheds light on the under-recognized “Genitourinary Syndrome of Lactation” and underscores the importance of better screening and care for new moms.
Suspected Causes and Treatment Approach
I suspected her pelvic floor muscle tension stemmed from childbirth-related perineal injury and her body’s natural tendency to tighten due to fear of prolapse. This tension likely contributed to her pelvic floor pain.
We began with techniques to relax her pelvic floor muscles, including breathing exercises and internal pelvic floor muscle release, and down-training the soft and connective tissues of the pelvic girdle with mobilization techniques. Jackie was given home exercises to relax her pelvic floor through breathing, stretches, and foam rolling. We later incorporated self-symptom management using a pelvic wand to help release her pelvic floor tension. Additionally, we focused on deep core activation and diaphragmatic breathing to support her pelvic floor muscles and alleviate the heaviness and pressure. Proper breathing patterns are crucial to managing pelvic floor pressure and prolapse symptoms, especially during lifting and other daily activities. We also worked on lifting mechanics and carrying postures to help manage pressure, and included hip strengthening exercises to support her pelvic floor muscles and improve pelvic stability.
Achieving Goals!
By the fourth visit, Jackie was able to go cross-country skiing without experiencing heaviness or pelvic pain. By the sixth visit, her daily pelvic pain had resolved, with only intermittent pain during higher-level activities. We progressed her exercises, incorporating hip hinging, lunging, and hip stability with increased loads as tolerated, to mimic her daily activities and goals.
Although we planned for 12 visits, I saw Jackie for nine due to her moving from the area. By the ninth visit, she could hike one mile while carrying her baby, go on three-mile hikes without pelvic pain, and squat and lift her baby without pain. She was mostly symptom-free! Both of us were confident that she could manage any occasional postpartum symptoms independently with her home exercise program.
Why Every New Mom Deserves To See a Pelvic Floor Physical and Occupational Therapists
Whether you are pregnant or postpartum, pelvic floor therapy can be a great resource! Pelvic floor dysfunction and/or pelvic floor disorders can be treated by seeing a pelvic floor physical and occupational therapists! Postpartum pelvic floor recovery can seem intense, but your pelvic health is crucial for a variety of basic bodily functions. Your well being is important, especially when experiencing postpartum issues. Regardless of the pelvic floor issues you are experiencing, we hope referrals to see a pelvic floor therapist becomes more common practice to all those postpartum.
All pregnant and postpartum women can benefit from pelvic floor physical and occupational therapy given the crucial role these muscles play during delivery and how prevalent dysfunction is after birth. Pelvic floor physical and occupational therapy reduces the risk of pelvic organ prolapse, urinary, bowel, and sexual dysfunction and pelvic pain. Similar to other diagnoses we treat, many of our patients tell us they wish they knew about us sooner.
Postpartum pelvic floor therapy can help with pelvic floor disorders such as:
- Urinary retention, urgency, frequency, hesitancy, pain and incontinence (leaking)
- Constipation, difficulty with bowel movement, fecal incontinence
- Painful sex, diminished or absent orgasm
- Diastasis Rectus Abdominis
- Restoring core function and strength: abdominals and pelvic floor muscles
- Pelvic floor and pelvic girdle, low back, and hip pain
- Cesarean section and episiotomy scar tissue and pain
- Pelvic organ prolapse prevention and/or treatment
- Eliminate perineal pain and/or levator ani trauma
- Reduce pain from pelvic neuralgias
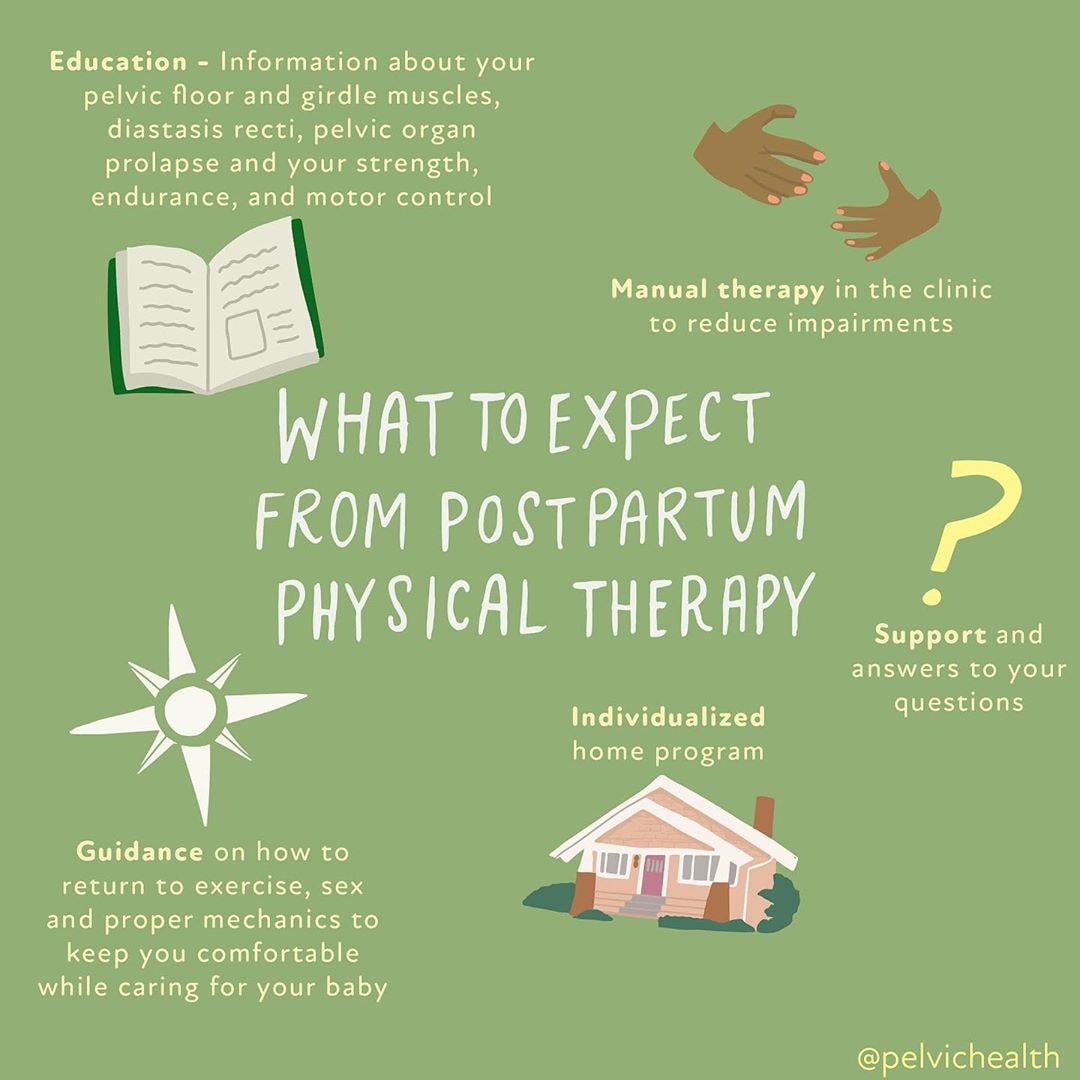
What to Expect from Postpartum Physical and Occupational Therapy
Education
Information about your pelvic floor and girdle muscles, diastasis recti, pelvic organ prolapse and your strength, endurance, and motor control. We want you to know about your pelvic floor anatomy!
Manual Therapy
In the clinic to reduce impairments (whether that was a vaginal delivery or not). Your pelvic floor therapist will create an individualized treatment plan.
Guidance
On how to reduce pain, return to exercise/physical activity, sexual intercourse (reducing painful sex) and proper mechanics to keep you comfortable while caring for your baby. You will receive a home exercise program with pelvic floor exercises geared towards your specific needs.
The Facts
- Up to 70% of women experience stress urinary incontinence in the postpartum period
- 36% of women have persistent Diastasis Rectus Abdominis after giving birth
- Up to 65% of women experience sexual dysfunction 18 months postpartum, regardless of the method of delivery
- 21% of women who undergo vaginal deliveries have Levator Ani Avulsion
- Vaginal deliveries are the number one risk for pelvic organ prolapse
- 77% of postpartum women have low back pain that interferes with daily tasks
- 51% of women can not perform a kegel with verbal cuing alone, 25% of women perform the exercise in a manner that promotes further (pelvic floor) dysfunction
Additional Resources from our PHRC Blog:
Diastasis Recti: What is it and who can it affect?
Moisturize My Vagina?! What you need to know
Top 5 Stretches to Relax the Pelvic Floor Muscles
Foam Rolling for your Pelvic Floor
Pain Interventions for Labor and Birth With a Partner
Other Postpartum Success Stories:
Postpartum Urinary Incontinence is Common: Here’s How We Can Help
Pain in your tailbone? You are not alone: Michelle’s Success Story
Success Story: Pelvic Floor PT Helped Charli Resolve Postpartum Pain
Success Story Jamie: Pushing Back Against Postpartum Prolapse
Source
Perelmuter, S., Burns, R., Shearer, K., Grant, R., Soogoor, A., Jun, S., Meurer, J. A., Krapf, J., & Rubin, R. (2024). Genitourinary syndrome of lactation: a new perspective on postpartum and lactation-related genitourinary symptoms. Sexual medicine reviews, qeae034. Advance online publication. https://doi.org/10.1093/sxmrev/qeae034
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Jandra Mueller, DPT, MS, PHRC Encinitas
Here at PHRC we regularly discover all sorts of new and cool products that are available for people’s pelvic health needs. I am amazed at some of the products available and that are being developed and am so thankful there are people that are creating these products because they are SOOO helpful! This is an updated version of one of our previous blogs, since there have been some new developments in the last few years and we wanted to share them with you!
Pelvic health physical and occupational therapistss treat a multitude of conditions that can include, but are not limited to, urinary dysfunction, sexual dysfunction, bowel issues (aka pooping), as well as pain in the pelvic region. Pelvic floor dysfunction is not a gender-specific disorder and can affect all people at different phases of their lives.
This week, we wanted to highlight some of our continued go-tos that can help people recover from pelvic pain, specifically painful sex, and introduce some new products that have been developed. There are a variety of pelvic floor disorders that affect daily life; we hope this list helps you receive the best care possible while alleviating any discomfort being experienced. If you see a product on this list that interests you, it may be a good idea to discuss it with your physical and occupational therapists and how it can be implemented into your treatment plan.
Let’s talk about sex baby… and many of the products, tools, and resources available.
Dilators aka “trainers”
Here at PHRC we have quite a few that we are a fan of! Dilators are used to increase tolerance of both vaginal and anal sex for all people, straight, bisexual, transexual, pansexual… literally everyone! There are differences in materials, colors, styles, and pricing so finding the right fit for you is important. Dilators are a great tool to pair up with a regimen of pelvic floor physical and occupational therapy.
 Milli vaginal trainer
Milli vaginal trainer
This dilator is unique, it is the only expandable dilator yet. This means that you don’t have to insert a series of dilators each time which may eliminate irritation if you have pain with initial insertion. It expands inside of you and you can measure specifically the dilation. Recovering from painful sex can take time, we love that this device helps people objectively measure progress with the digitized face depicting the size it has expanded to. It is made of a soft silicone and it does have a vibrating feature. It comes in its own charging case so it is easier to travel with as well.
 Soul Source Silicone Dilators
Soul Source Silicone Dilators
With the release of their new silicone finish, these dilators come in a vast variety of sizes and have different sets to match your needs. They are also made locally in CA! They are a bit on the pricier side, but they are definitely a quality product!
 GRS – Dilator set by Soul Source
GRS – Dilator set by Soul Source
Soul source has made these specifically for those undergoing gender reassignment surgery in conjunction with a surgeon that performs this surgery. These dilators are made of rigid polyurethane, and can be chilled in order to use for post-surgical swelling in addition to using them for general dilation post-surgery.
New Flora Dilator Sets |
She-ology Wearable Dilators |
Intimate Rose Dilator Set |
||
 With a nice smooth silicone finish, these dilators are slightly different in length and size, and are one of the more affordable sets on the market. With a nice smooth silicone finish, these dilators are slightly different in length and size, and are one of the more affordable sets on the market. |

These silicone dilators are like no other. This is the first set of wearable dilators for those that want to try a different position or move around. They also come in a larger, more advanced set.
|

Similar to soul source, these offer soft silicone (maybe even a little softer) and a variety of sizes and sets, and a bit cheaper as well! Silicone in general is nice because it often feels more like human skin instead of hard plastic. |
 Clone-A-Willy
Clone-A-Willy
Yes, you heard it correctly, a cloning kit that allows you to clone your partner! This is for patients working specifically towards a goal of pain-free intercourse with their partner who may have anxiety/have a hard time communicating their needs during intercourse with their partners. Also comes in a variety of colors, and it even glows in the dark!
New Flora Pelvic Wand
Intimate Rose Pelvic Wand
Many patients ask us, “so how can I do this on my own?” Well, the pelvic wands offer just that. With the S-shape meant to help with your ergonomics of gripping, this slides right in and allows you to access your pelvic floor muscles. With the tapered end, it’s great for trigger point release. They also offer a wand with a vibrating feature as well. There are now a couple on the market, both offering vibrating options, though each have a slightly different shape.
Ohnut!
Made for the people, by the people. This device made by The Pelvic People, was developed for those that have pain with deep penetration. They are very soft, stackable rings that go on the male partner to create essentially a buffer so that penetration does not go so deep, yet both partners still feel pleasurable. They now offer an additional vibrating ring to enhance pleasure!
 The Kiwi
The Kiwi
Featuring the newest product from The Pelvic People, this device is a two-for-one. With the ability to help you tackle pelvic pain and progress towards pleasure, this is one of the best devices on the market right now! Offering a dual control vibration and multiple options for use, we give it 5 stars!
Personal Lubricants
To begin, there are a ton of personal moisturizers aka lubricants out there that are better used for anal vs. vaginal use. These depend on both the pH of the product as well as the osmolality. And there are things to consider like water-based or oil-based. SO. MANY. OPTIONS!
Lube + Sperm:
- The best conditions for sperm survival and motility is pH 7.2-8.5 and osmolality 270-360 mOsm/kg.
- Brands: Pre-Seed, Yes Baby
Vaginal and Rectal pH
- Vaginal: 3.8 – 4.5
- Rectal: 7.0
Osmolality
- The World Health Organization (WHO) recommends osmolalities of less than 380 mOsm/kg
- Silicone-, Plant, and Oil-based lube are also less likely to irritate, but their osmolality cannot be measured.
For a more in depth review about why lube selection is important, one of our senior physical and occupational therapistss, Melinda Fontaine (Walnut Creek, CA), wrote a blog that you can read here.
What we use in the clinic:
Typically we use slippery stuff for our transvaginal work and surgilube for transrectal work. Releveum is now classified as a moisturizer because it can be used for longer than 60 minutes, while lubes are short-term and do not last longer than 60 minutes. Releveum is an aloe vera based lube/moisturizer. It contains 4% lidocaine that can be used to help soothe or numb burning tissue, like for those that have pain with initial penetration and suffer from Vestibulodynia, and can help in the short-term for improving that pain!
Moisturizers and other care products for “down there”
There are some other moisturizers that can be helpful for irritated tissue, especially if you don’t want to, or cannot use hormones for any reason. There are two that we often recommend for women that have pain with initial penetration from irritated or inflamed tissue at the entrance of the vagina and the vestibule. I often recommend them for my mama’s that are pregnant or postpartum and CANNOT use any hormones (even local ones) because it is contraindicated in pregnancy and postpartum. This is also true for those women who are concerned about, or would feel more comfortable not using hormones because they have had certain types of cancer.
Vital V V-Magic
These are both used to soothe the tissues, but have slightly different ingredients. Vital V has vitex, which is chaste berry extract while Vmagic has some ingredients that are more antimicrobial. We use them both and it may just be a personal preference of which may work for you!
 Kindra
Kindra
The Daily Vaginal Lotion features a blend of ultra-hydrating extracts to support skin-moisture barrier healing for vulvar and vaginal dryness. Whereas the V Relief Serum features a biomimetic peptide clinically studied to reduce skin sensitivity and reactivity, including stinging, burning, and itching.
Education
If you have ever been a patient here at PHRC, visited our office, or seen our videos on social media, you know how valuable education is to us!
When Sex Hurts
Pelvic Pain Explained
PHRC’s First E-Book!
Our favorite books to recommend are “When Sex Hurts” which has been updated with SO much new information about the causes of painful sex and what you can do about it, authored by some of the top pelvic health specialists in the world. “Pelvic Pain Explained” which was co-authored by PHRC’s co-founders Stephanie Prendergast (Pasadena, CA) and Elizabeth Akincilar (Merrimack, NH) and PHRC’s very first e-book “Vulvodynia, Vaginismus, & Vestibulodynia: Your guide to diagnosis and treatment” by Stephanie Prendergast, Elizabeth Akincilar, and Jandra Mueller. You can find this book for $10 on our website. We’ve compiled so many of the resources we’ve collected over the years into a fun, digestible book for patients to get the help they need
Your toolbox does not need to just be manual therapy techniques! If you have feedback about these products we’d also love to hear so feel free to comment below and share some of your favorites! We love to hear back from patients and healthcare providers about the types of products they use as treatment options.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok












 Milli vaginal trainer
Milli vaginal trainer  Soul Source Silicone Dilators
Soul Source Silicone Dilators GRS – Dilator set by Soul Source
GRS – Dilator set by Soul Source
 Clone-A-Willy
Clone-A-Willy








 Kindra
Kindra

