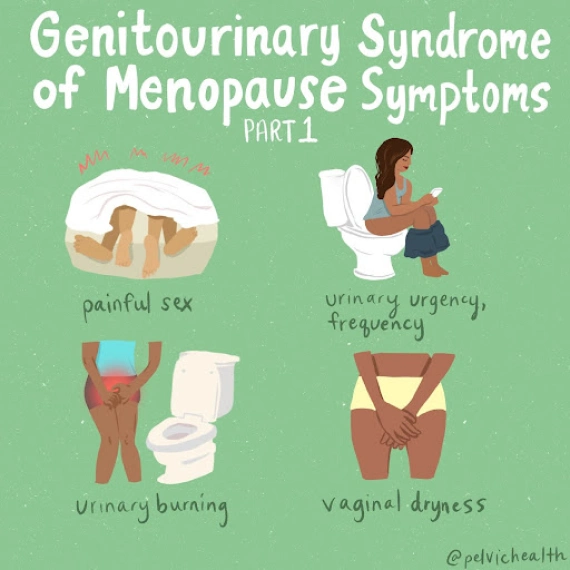
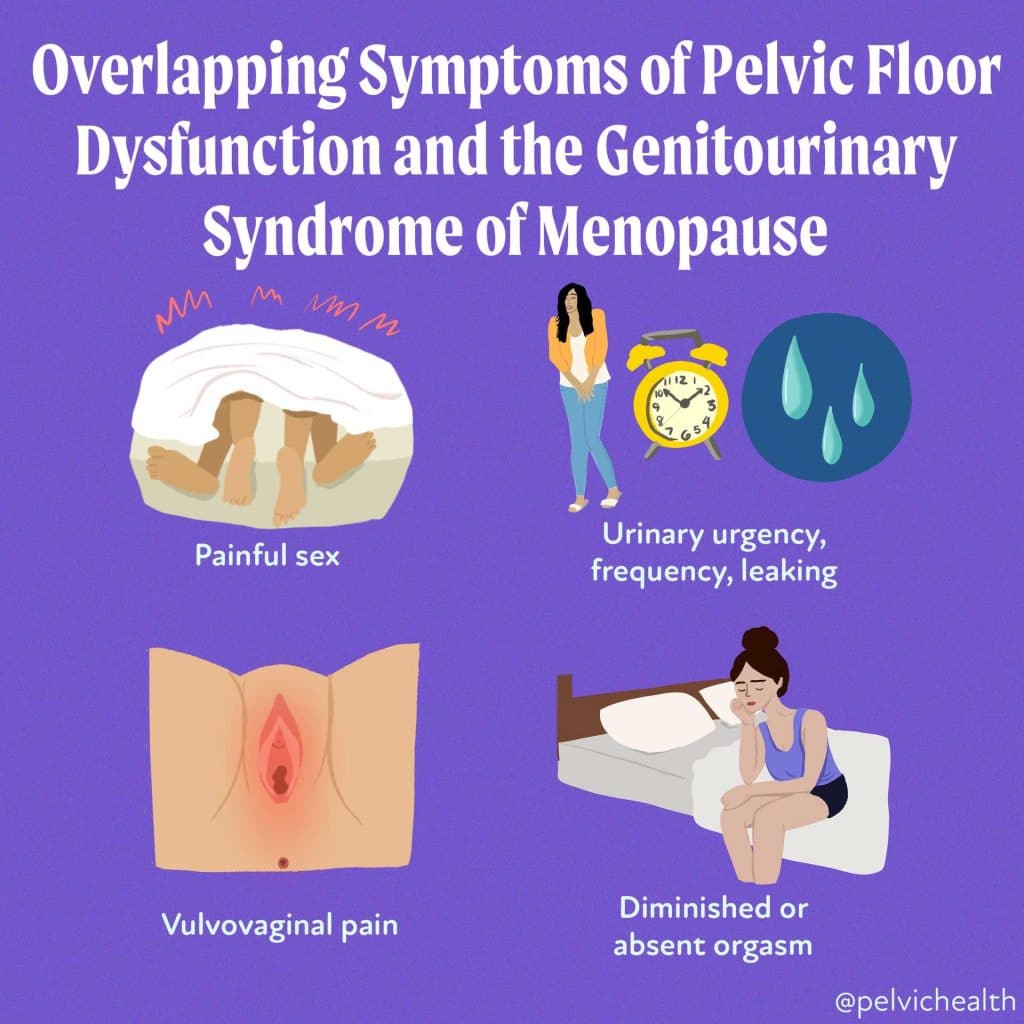
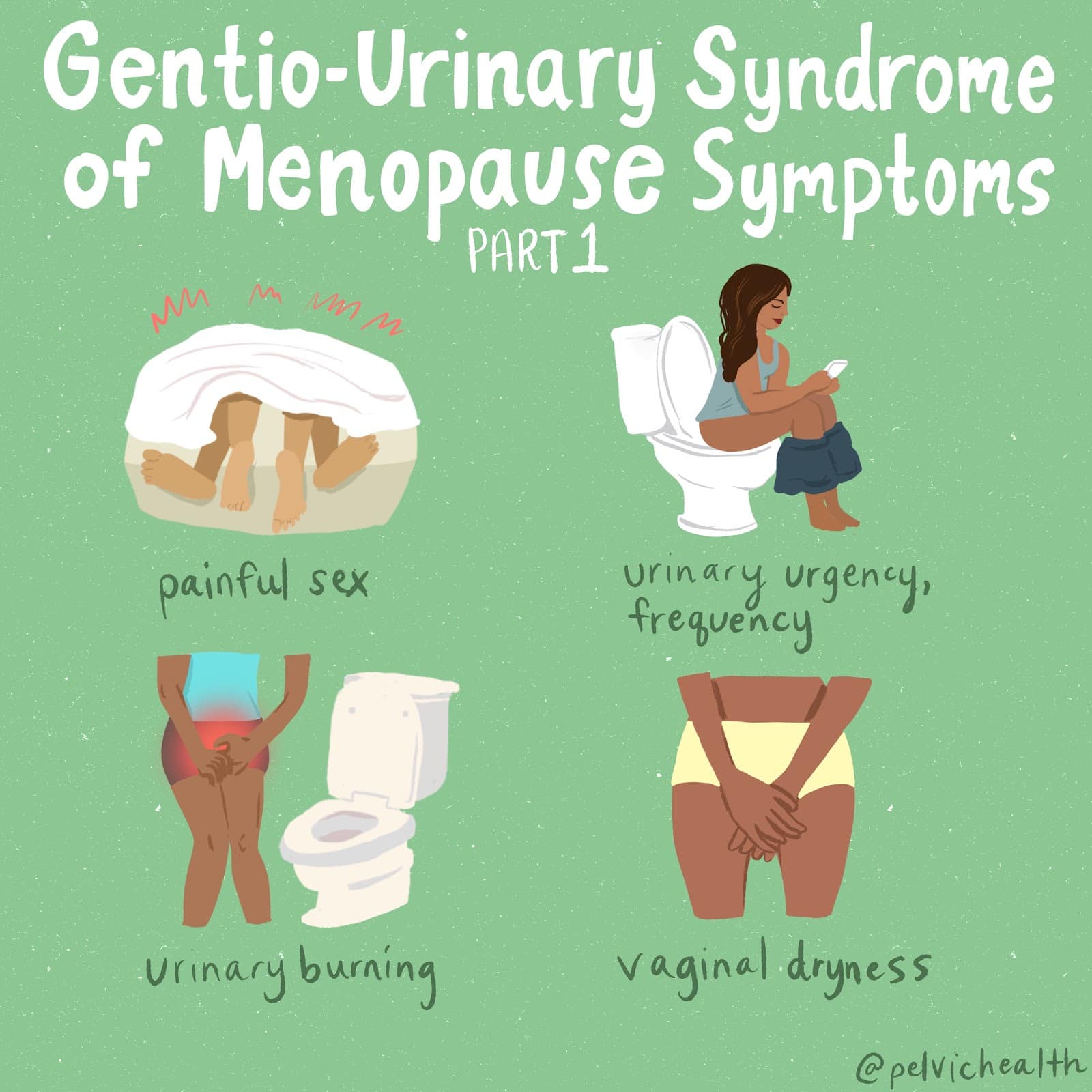
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting
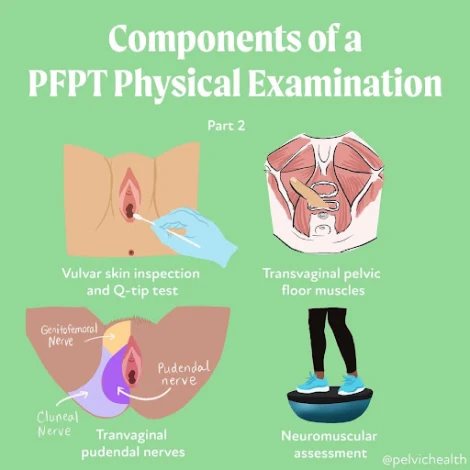
An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.
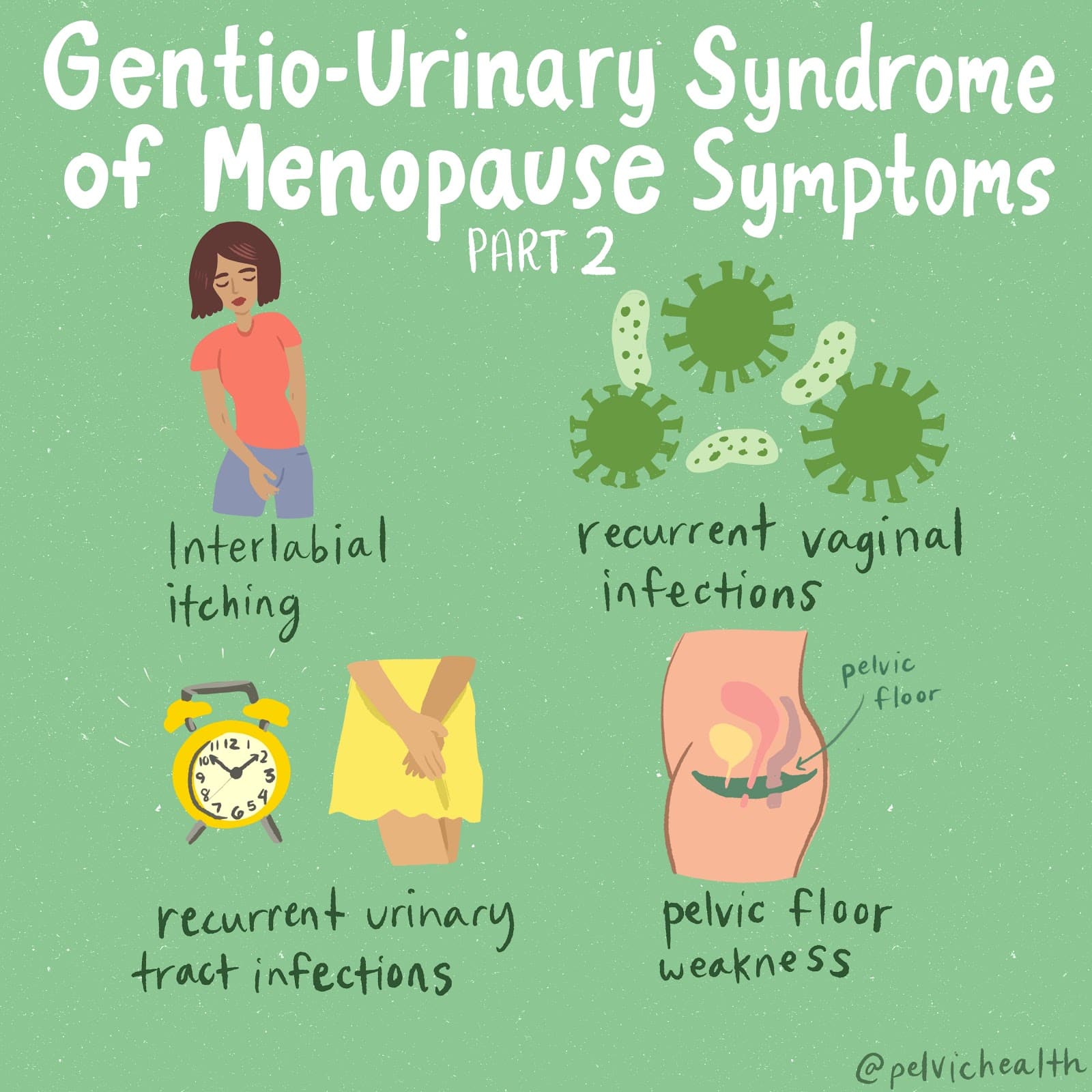
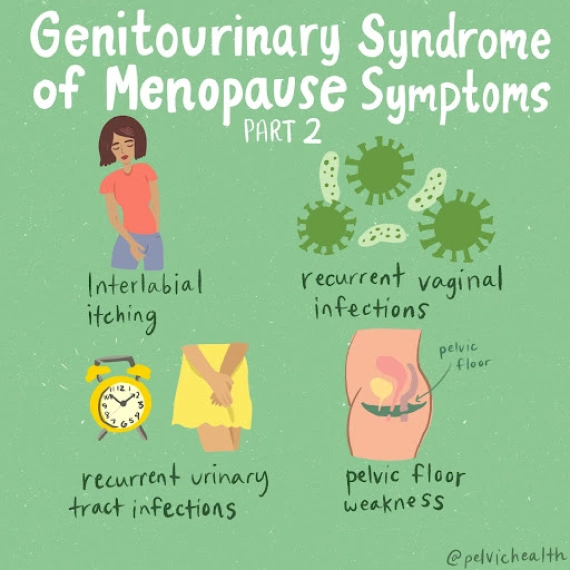
Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
By Cambria Oetken, DPT, PHRC Westlake Village
Here is What You Need To Know!
This year new moms are finally getting the attention they deserve! We are excited to report our trusted sexual medicine experts coined a new term that describes the genitourinary hormonal deficiencies of lactating moms experience.
What is the Genitourinary Syndrome Lactation?
Earlier this year, an article was published proposing the novel term, genitourinary syndrome of lactation (GSL) in hopes to bring awareness to this population as well as the proper management, treatment and diagnosis. GSL describes the collection of genitourinary symptoms experienced by postpartum moms during the lactation period. While postpartum already encompasses significant changes both emotionally and physically, additional care should be provided for those suffering from genitourinary symptoms in order to alleviate burden and optimize wellness during a vulnerable time. The collection of genitourinary symptoms include vaginal dryness, dyspareunia, urinary symptoms and alterations in sexual function which can significantly impact these patients quality of life. This syndrome occurs due to hormonal changes associated with alterations in the genitourinary tract that will be discussed further.
Lactation and the potential impact on the genitourinary tract
Lactation comes with in depth physiological changes creating significant hormone shifts. In the first trimester of pregnancy, estrogen changes areola enlargement and maturation. In the second trimester, there is an increase in progesterone that helps with colostrum production and lobe proliferation. By the 3rd trimester, mature cells form, colostrum is produced by oxytocin in preparation for lactation to occur. Postpartum, there is a drop in progesterone and an increase in prolactin to drive milk supply. This increase in prolactin decreases the ovarian production of two crucial hormones, estrogens and androgens (such as testosterone). To maintain proper lactation, prolactin has to be present which in turn continues to suppress estrogen and androgen release. Lactating women therefore experience a hypoestrogenic and hypoandrogenic state, persisting at times as long as lactation continues. This state is similar to menopause. Estrogen is needed for maintaining vaginal wall thickness and lubrication as well as urethral and vulvar thickness. There are several estrogen receptors in this genitourinary tract including the clitoris and bladder trigone as well. Estrogen is also responsible for maintaining lactobacillus which is needed to maintain a healthy acidic PH to help fight off infections. Androgens also work hand in hand with estrogen to maintain vascularity and healthy vaginal tissue therefore, with the reduction of these, this puts the patient at risk for dyspareunia (pain with intercourse), Vestibulodynia (pain at the vestibule), and can limit sexual desire as a whole.
Vaginal dryness continues to be a primary concern in these individuals that can contribute to discomfort, irritation and pain with sexual intercourse (dyspareunia). Another contributing impact from a lack of estrogen is the ability to recover optimally from vulvovaginal tears or injury. Estrogen promotes growth of crucial cells to help repair tissue. Studies have shown that supplementing with estrogen can improve wound healing synthesis and boost collagen during this repair phase.
Another disrupting symptom that is common postpartum is urinary incontinence. Urinary incontinence is common postpartum and can be emotionally distressing and shameful for patients and society has normalized this as a result of pregnancy. Additional conditions include pelvic organ prolapse and even anal incontinence. There is a connection between SUI and collagen and as we know, collagen is reduced in lactating women due to depletion of estrogen needed for tissue repair and collagen optimization.
Treatment Approaches for Genitourinary Syndrome Lactation (GSL)
Pharmacological Options
Vaginal Estrogen Therapy can be an option for women experiencing vaginal dryness or with complaints of dyspareunia, recurrent UTIs, or vulvar and vaginal changes. While there are limited studies on estrogen therapy in this population, there have been positive subjective reports of improvement at the perineum with no serious adverse events noted. The concern and hesitation with vaginal estrogen use is that it may transfer to breast milk or reduce milk supply. However, even in studies using the highest dose of estrogen possible there were no traces of estradiol detected in breast milk and is unlikely to affect breast milk supply. We know from previous research that low dose vaginal estrogen is considered safe even in women with estrogen receptor positive malignancies (cancer).
DHEA has been indicated for the use for the genitourinary syndrome of menopause and is FDA approved for severe dyspareunia in postmenopausal women. DHEA works to convert to estrogen and testosterone and has limited concern for absorption systemically. DHEA is not currently being used in lactating mothers and there are a lack of studies in its use with this population.
Non pharmacological Options
Functional Microablative CO2 laser is being studied for vulvovaginal atrophy and some researchers have found improvements in dyspareunia, pain at vaginal orifice and dryness.
Vaginal Lubricants and Moisturizers
Lubricants and moisturizers can be helpful in this population as vaginal dryness tends to be one of the most common concerns that can also impact sexual functioning. This option could be a first step approach that is conservative and easily accessible. Moisturizers and lubricants with hyaluronic acid (HA) have been shown to significantly improve these symptoms and even quality of life just after 12 weeks of use. Additional studies have shown HA use with estriol cream to have an even greater impact when combined. Some of our favorite moisturizers and lubricants can be found below.
Pelvic Floor Physical and Occupational Therapy and Occupational Therapy
This is crucial in optimizing both peripartum and postpartum challenges involving the genitourinary tract. Through exercises, manual therapy, education on proper postures especially with breastfeeding, body mechanics, improving pelvic floor motor control and strength, enhancing sexual wellbeing and overall optimizing postpartum recovery. Therapy can also help to reduce severe perineal tearing through instruction on perineal massage and positional options during delivery to further reduce recovery time postpartum. Pelvic floor therapy has been shown to decrease the risk of urinary incontinence in late pregnancy and postpartum and women were less likely to report pelvic organ prolapse and with a reduction in unsatisfactory sexual function. Pelvic floor therapy should be considered standard care during and after pregnancy to optimize function, well being and prevent potential genitourinary symptoms.
Conclusion
In conclusion, GSL hopes to be recognized as a diagnosis to help bring support and optimal treatment to these lactating individuals in order to optimize their well being both emotionally and physically during a critical period. Should you be an expecting mom, reaching out to your physical or occupational pelvic floor therapist is a great start to begin preparing for progression of pregnancy, delivery and postpartum and can help guide you through an evolving time. Therapists can also work closely with your provider in managing GSL. If you live near one of our 11 locations, please give us a call, we are happy to help!
Reference:
Perelmuter S, Burns R, Shearer K, Grant R, Soogoor A, Jun S, Meurer JA, Krapf J, Rubin R. Genitourinary syndrome of lactation: a new perspective on postpartum and lactation-related genitourinary symptoms. Sex Med Rev. 2024 Jun 26;12(3):279-287. doi: 10.1093/sxmrev/qeae034. PMID: 38757214.
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: genitourinary system, urinary tract, breastfeeding, birth, infants, support, breastfed, health
By Cambria Oetken, DPT, PHRC Westlake Village
The Clitoris. We Found it!
There is conflicting evidence as to when the clitoris was exactly discovered and studied. It is thought to date back to 400 BC when Hippocrates described the clitoris as a protrusion which functioned to protect the vagina. There was a later time when anatomists denied its existence altogether. With religious and cultural influences, the clitoris was either disregarded or demonized and in the middle ages, it was even known as “the devil’s teat.” A procedure called a cliteroidectomy (removal of the clitoris) was even a commonly utilized medical practice to treat “hysteria.” With a confusing and lack of understanding about its history, it was only until recently in 2005 that O’Connell, Sanjeevan, and Hutson published in The Journal of Urology recognition of this organ of female sexual pleasure as a three dimensional organ through cross sectional imaging. We now know that the clitoris is more than what is seen on the surface composed of the internal paired clitoral bulbs, corporal bodies, and crura which is composed of erectile tissue. It was not until 2022 however that it was determined the clitoris is composed of 10,000+ nerve fibers which has been discussed as more than a human penis contains. Sounds pretty sensitive and important right??
Stop Ignoring the Clitoris
Historically, and currently, there is a lack of research in regards to the clitoris while the penis has been a counterpoint of research for centuries. Within this new era, the clitoris is becoming more recognized, understood and appreciated for its complexity and sensitivity as well as its importance in female sexual wellness. Luckily, there are prominent medical providers who are bringing more attention to this organ and to women’s sexual wellness as a whole. In a recent New York Times article, written by Rachel E. Gross, she interviews Dr. Rachel Rubin, a urologist and sexual medicine expert, who has been a pioneer in driving attention to women’s sexual health. Dr. Rubin is breaking down barriers around the context of the vulva and the clitoris being “private and shameful” parts thus further empowering the lives of women worldwide. In this article, Dr. Rubin states how the clitoris is “completely ignored by pretty much everyone,” and that “there is no medical community that has taken ownership in the research, in the management, and in the diagnosis of vulva-related conditions.”
F
The article recognizes how there is little to no education about the clitoris in medical school and how women’s health and sexual health as a whole is not a focus for women at all. In fact, in many surgeries such as pelvic mesh surgeries, urethral surgeries even minimally invasive hip surgeries put this organ, its several nerve endings and supporting pelvic nerves at severe risk however is not protected by providers due to its historical lack of relevance, understanding and underlying anatomy.
Women’s lives can be severely impacted by damage to this important structure just as a male would be should there be damage to their counterpart. We now know that sexual wellness is a major part of health both mentally, emotionally and physically and thus should be treated with such importance as any other organ in the body.
Now for a quick anatomy lesson…
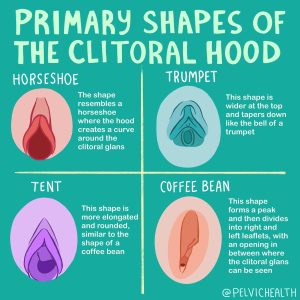
The clitoris is composed of more than just what we see as a knob on the external surface. What you see externally is the conveniently placed glans towards the top of the vulva with the clitoral hood draping over it. Think of this as the “tip of the ice berg” because beneath the surface are the much larger paired clitoral bulbs, corporal bodies, and crura, which are all composed of erectile tissue (as pictured below). Similarly these same structures can be identified in the male counterpart of the penis.
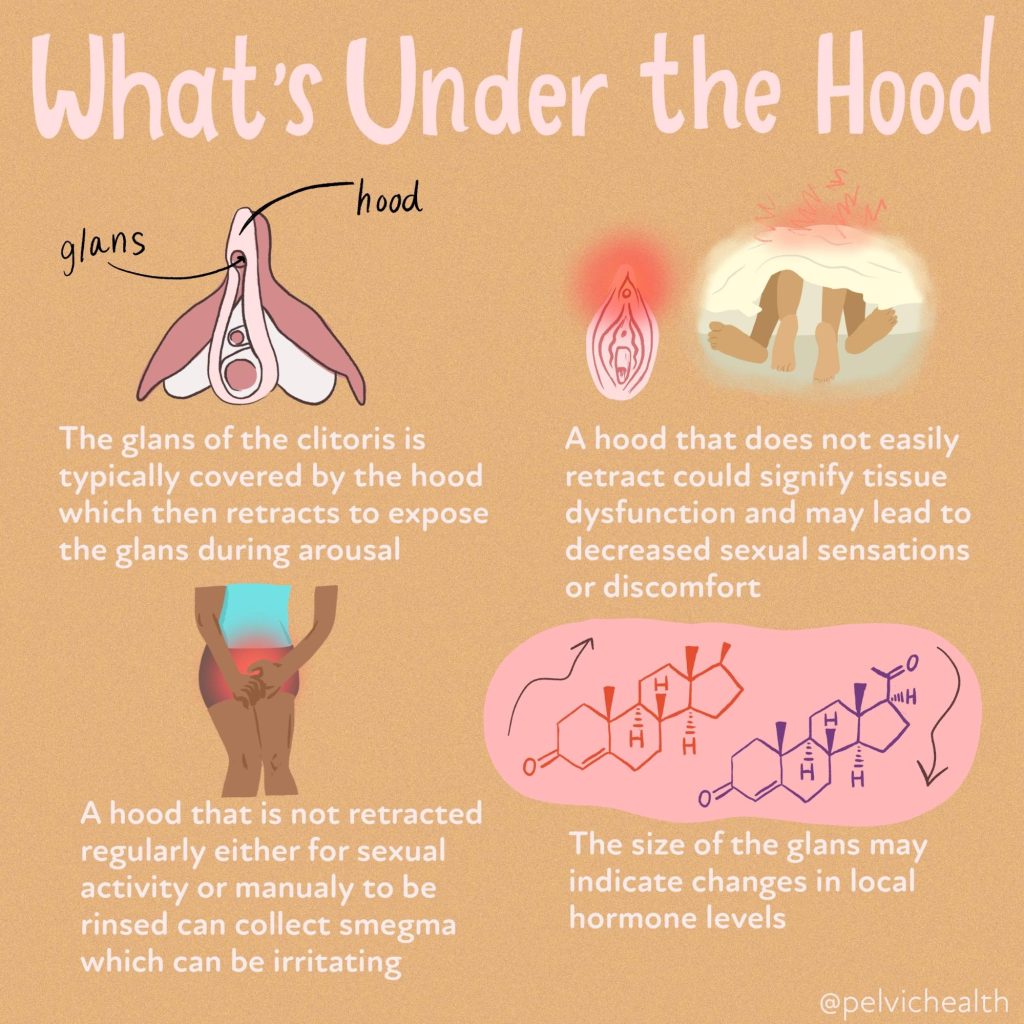
Men who are uncircumcised retract their foreskin to clean underneath. All people with a clitoris should carefully do the same, let us explain!
View this post on Instagram
Caring for and finding your clitoris
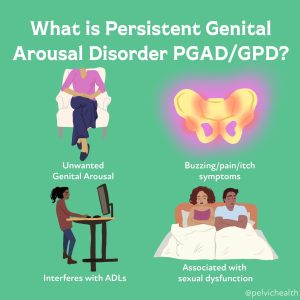
If you are having symptoms at the clitoris, such as pain, decreased arousal, decreased orgasm, absent orgasm, or additional arousal conditions such as persistent genital arousal disorder(PGAD)/genito-pelvic dysesthesia (GPD) it is important to share these concerns with your provider.
At Home Self-Exams
However, performing a self exam at home and becoming familiar with your anatomy can be a great start. Regular self exams can be helpful by using a mirror or by palpating the structures. Oftentimes there can be clitoral hood adhesions, vulvar dermatological concerns, smegma and keratin pearls around the clitoris that could be problematic. To examine your vulvar tissue, begin by laying back with a mirror in order to see the tissues appropriately. Begin by finding the clitoral hood or clitoris at the top of the vulva closest to your pubic bone. You can retract the clitoral hood with two fingers to expose the glans of the clitoris. The clitoral hood should move fairly easily and fully expose the clitoral head. If the clitoral hood does not move optimally or does not expose the glans there could be limited mobility or adhesions present. Also be aware of any smegma or discharge under the hood that could be building up.
A helpful strategy to potentially help with clitoral hood mobility and reduce buildup of discharge is by retracting the clitoral hood in the shower and letting warm water run over the area. Ensure you are avoiding harsh soaps or additional washes to this area to avoid irritation of the tissue. Again, it is always important to speak with your provider or a sexual medicine expert to address these issues.
Multiple pathologies such as pelvic floor dysfunction, pudendal neuralgia, PGAD, and vulvar dermatoses can lead to changes in sexual pleasure and can cause pain. Stay tuned to our blog for more in depth articles, if you have questions we are here to help and please reach out to us!
References
Half the World Has a Clitoris. Why Don’t Doctors Study It?
Human Clitoris Has Over 10,000 Nerve Fibers | Oregon Health & Science University (ohsu.edu). SexualDiversity.org
Maria Uloko, Paige Isabey, Blair Peters. How many nerve fibers innervate the human clitoris? A histomorphometric evaluation of the dorsal nerve of the clitoris, abstract was presented by Blair Peters, on Oct. 27, 2022, at the 23rd annual joint scientific meeting of Sexual Medicine Society of North America and International Society for Sexual Medicine.
Uloko M, Isabey EP, Peters BR. How many nerve fibers innervate the human glans clitoris: a histomorphometric evaluation of the dorsal nerve of the clitoris. J Sex Med. 2023 Feb 27;20(3):247-252. doi: 10.1093/jsxmed/qdac027. PMID: 36763957
Resources
Clitoral Pain: Unmasking Common Culprits
Clitoral Pain: Causes and Treatment
Why Your Clitoris Is In Pain [Youtube Video]
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: clitoral stimulation, clitoral hood, labia minora, glans clitoris, sexual arousal, nerve endings, female genital anatomy, female sexual function, female sexual response
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
Pudendal and Pelvic Neuralgias Symptoms, Causes, and Treatments
-
.
-
.
Pelvic floor muscles play an integral role in urinary, bowel, and sexual functioning. Additionally, they function as part of our core and support our pelvic organs. They are part of our pelvic girdle (the bones that support your hips and connect your legs to your spine). Most people do not know they even have pelvic floor muscles until issues arise and they begin to search for help and care. Because the nature of the symptoms can fall under the umbrella of urologic, gynecologic, and colorectal disciplines, people with symptoms often seek out the help of these providers. Recent studies have shown that medical schools do not currently include pelvic floor dysfunction training in their curricula, which is leading to diagnostic confusion and delays for suffering patients.
Pelvic floor dysfunction is a neuromuscular condition that must involve the care of a skilled pelvic floor physical or occupational therapist to establish a proper diagnosis and effective treatment plan. The therapists at the Pelvic Health and Rehabilitation Center have undergone extensive training in the management of pelvic floor dysfunction and are prepared and ready to help.
What is the Pelvic Floor?
The pelvic floor muscles are bowl-like muscles inside the pelvic girdle. They attach at the pelvic girdle. They are loosely grouped as superficial or deep.
The superficial muscles, also known as the urogenital diaphragm, include the bulbospongiosus, ischiocavernosus, superficial and deep transverse perineal muscles, and the urethral and anal sphincter muscles.
The deep layer consists of the levator ani muscle group, which includes the pubococcygeus, puborectalis, iliococcygeus, and coccygeus.
Additionally, the obturator internus and piriformis muscles are external rotators of the hip and also have portions of their muscle bellies that communicate with the pelvic floor muscles. While these two muscles are external hip rotators, they also play a role in pelvic floor muscle function and dysfunction.
The pelvic floor muscles have unique innervation (nerve supply) in that they reflexively work with our core, bladder, and bowel function. However, we also have the ability to override the autonomic control. These muscles are always active because of these reflexive loops. When the muscles become impaired, they might be too tight, too weak, or have dysfunctional neuromuscular control. When this happens, people can experience bladder, bowel, sexual dysfunction, pelvic organ prolapse, and pelvic floor, girdle, hip, and lower back pain.
Symptoms of Pelvic Floor Dysfunction
Pelvic floor dysfunction can manifest in a range of symptoms, which generally fall into five categories: urinary, bowel, sexual dysfunction, musculoskeletal, and/or neuropathic pelvic pain.
Historically, pelvic floor dysfunction was oversimplified into what was called ‘low-tone’ and ‘high-tone’ pelvic floor disorders.
The ‘low-tone’ pelvic floor disorders included symptoms such as urinary and fecal incontinence (loss of bladder or bowel control), pelvic organ prolapse (when pelvic organs drop from their normal position), and post-prostatectomy and other surgical repairs, and are associated with lifetime milestones involving physiologic change such as the post-partum period (the time after childbirth) and perimenopause and menopause. These symptoms and time frames leave the pelvic floor muscles vulnerable to impaired neuromuscular control (disruption in the communication between nerves and muscles), which can result in weakness and poor endurance.
The ‘high-tone’ pelvic floor disorders were associated with symptoms of urogenital pain (pain in the urinary or genital region), irritative bladder symptoms (frequent or urgent need to urinate), and sexual pain and were more commonly identified in adolescents through aging adults of all sexes. While aging adults often suffer from sexual pain disorders, early pelvic pain research separated out premenopausal and menopausal women to show that muscular dysfunction and sexual pain can exist in premenopausal years as well.
However, emerging research on pelvic floor disorders has broadened our understanding of the syndrome, and we now understand people with any pelvic floor diagnosis or cluster of symptoms can have muscle dysfunction that includes elevated or reduced EMG findings (or tone), impaired neuromuscular control (disruption in nerve-to-muscle signaling), impaired lumbo-pelvic-hip biomechanics (issues with how the lower back, pelvis, and hips move together), muscle pain, weakness and endurance challenges.
Problems in how the body functions can happen at any age and in all sexes. Appropriate interdisciplinary care that includes pelvic floor physical and occupational therapy allows us to collaborate to establish the proper differential diagnosis and care plan.
1. Urinary Symptoms
Bladder changes are a common symptom of pelvic floor dysfunction. These symptoms can vary in severity from barely noticeable to severely limiting. Examples of urinary symptoms that are associated with pelvic floor dysfunction are listed below. Patients may experience some of these symptoms or a combination of multiple symptoms on this list.
- Stress Incontinence, which is the involuntary leaking of urine when coughing, laughing, sneezing, or during exercise, this is also common after pelvic surgeries, including prostatectomy
- Urge Incontinence, which is the involuntary urinary leaking when the urge strikes, such as putting the key in the front door to head to the bathroom
- Mixed Incontinence, which is a combination of both stress and urge incontinence
- Bladder pain, involves discomfort or pain in the bladder region, upon bladder filling or without bladder filling
- Urethral pain, which can occur unprovoked (spontaneous) or in a provoked situation such as in response to touch, urination, or clothing or sitting. Urethral pain can also occur before, during, and after urination
- Urgency/frequency, which is the feeling of needing to urinate urgently, even when the bladder isn’t full, can lead to frequency which refers to an increased number of trips to the bathroom
- Urinary hesitancy, involves difficulty starting the urine stream or having a slow flow
- Climacturia, which is leaking urine with orgasm
Causes of Urinary Issues/Bladder Dysfunction
Tight, weak, and discoordinated pelvic floor and girdle muscles can cause urinary dysfunction. There are a number of reasons pelvic floor muscles can become dysfunctional, key reasons are listed below.
- Recurrent Urinary Tract Infections (UTIs), urinary tract infections are considered recurrent if someone has more than 2 in a 6-month period or more than 3 in one year, the bladder irritation from the infection triggers the viscero-somatic reflex and pelvic floor dysfunction can occur and can continue to mimic the symptoms of a UTI in the absence of infection
- Hormonal deficiencies, specifically the Genitourinary Syndrome of Menopause (GSM), the Genitourinary Syndrome of Lactation (GSL), and Hormonally Mediated Vestibulodynia in premenopausal women can cause irritation of the vestibule, which houses the urethra, and these deficiencies also cause pelvic floor dysfunction
- Hormonally mediated vestibulodynia can be caused by medications that suppress free testosterone, including oral contraceptives, GnRH agonists, and acne medications
- Biomechanical or structural dysfunction, including hip dysfunction, sacroiliac joint dysfunction, piriformis syndrome, scoliosis, leg length discrepancy
- Pelvic Floor Dysfunction, involving tight, weak, or discoordinated pelvic muscles
- Pelvic Organ Prolapse, which occurs when the pelvic organs descend into the vaginal canal and cause urinary symptoms
- Endometriosis, constipation, and gastrointestinal distress or bloating, which cause increased pressure on the pelvic floor and bladder and can cause urinary symptoms
Treatment for Urinary Issues/Bladder Dysfunction
The American Urological Association published guidelines in 2011, 2014, and 2022 stating that manual pelvic floor physical and occupational therapy is the first-line treatment for people with irritative bladder symptoms associated with the diagnosis of Interstitial Cystitis/painful Bladder Syndrome. The International Continence Society also recommends physical and occupational therapy as first-line treatment for people with urinary leaking. Once lower urinary tract pathology is ruled out or being treated, an evaluation with a pelvic floor physical or occupational therapist is warranted.
A trained therapist will assess your pelvic floor and girdle muscles, neuromuscular control, and will evaluate biomechanics and strength, length, and endurance, as well as peripheral nerves and the central nervous system.
Treatment often involves manual therapy, neuromuscular re-education, home exercises, patient education, and help with plan of care coordination when other providers are also involved.
2. Bowel Symptoms
Bowel dysfunction can cause significant discomfort and distress. Many people experience symptoms like constipation, difficulty evacuating stool, anal pain, and/or fecal incontinence due to pelvic floor issues.
- Straining to evacuate stool, involves difficulty or pain when passing stool
- Constipation, involves infrequent or difficult bowel movements
- Fecal or gas leakage, which is involuntary leakage of stool or gas
- Hemorrhoids and fissures, which are painful, swollen veins in the rectum or tears in the anal lining
- Anal/Rectal pain, involves burning, itching, or pain before, during, or after bowel movements or spontaneous unprovoked pain, symptoms can also be triggered with exercise, sitting, or clothing
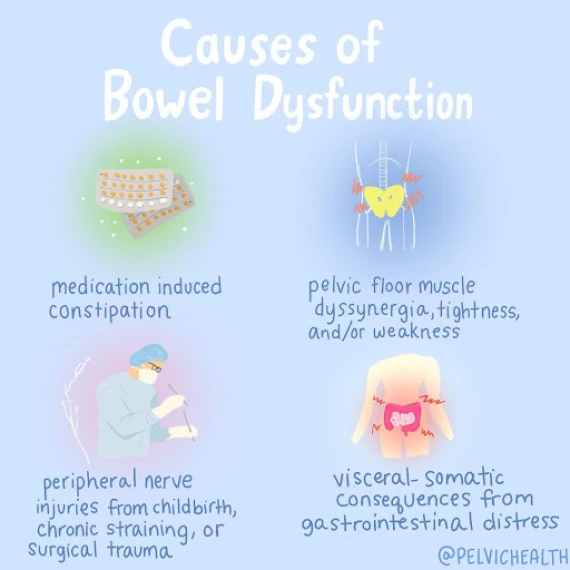
Causes of Bowel Symptoms
Bowel issues from pelvic floor dysfunction can result from:
- Medication-induced constipation, including opiates, mood stabilizers, oral contraceptives
- Pelvic Floor Muscle Dyssynergia, occurs when muscles are either too tight, too weak, or uncoordinated
- Peripheral nerve injuries, caused by childbirth, chronic straining, or surgical trauma
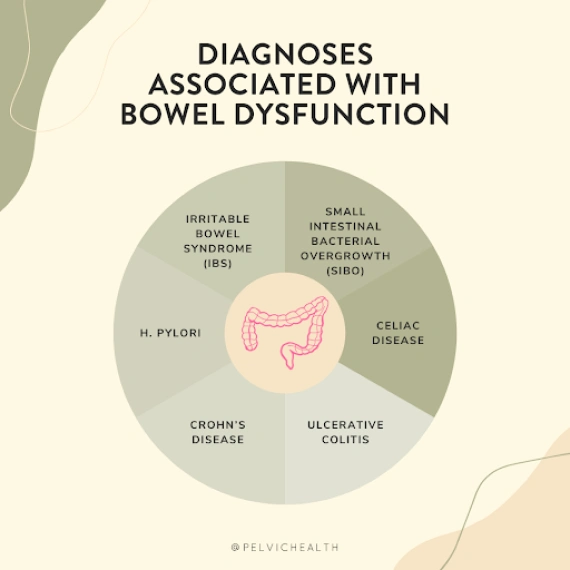
- Visceral-somatic consequences, which includes gastrointestinal issues such as IBS, Crohn’s disease, ulcerative colitis, SIBO (Small Intestinal Bacterial Overgrowth)
- Conditions like anal fissures and hemorrhoids, which are often caused by faulty bowel mechanics and are a sign of pelvic floor dysfunction (they are also painful and can cause further pelvic floor dysfunction and pain in response to the irritation from these tissues themselves)
Treatment for Bowel Issues
Pelvic floor physical and occupational therapy are key treatment options for bowel dysfunction. A pelvic floor physical or occupational therapist will assess the coordination and strength of the pelvic floor muscles and create a treatment plan focused on improving muscle control. Treatments might include exercises to improve coordination, manual therapy, and biofeedback to help regain control over bowel movements.
3. Sexual Dysfunction Symptoms
Sexual dysfunction is associated with pelvic floor dysfunction in all genders and ages.
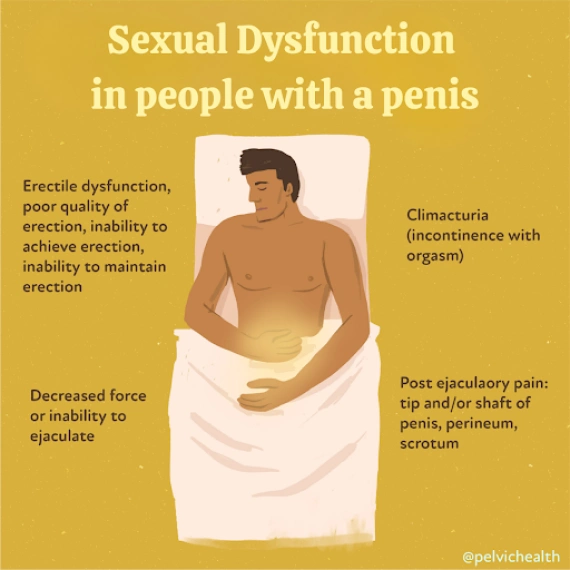
Symptoms of Sexual Dysfunction in People with Penises
- Erectile Dysfunction, involves poor quality, and inability to achieve or maintain an erection, which can occur in men of any age and is also a common complication after prostatectomy
- Premature Ejaculation, involves the inability to delay ejaculation
- Decreased Force or Inability to ejaculate, involves weak ejaculation or no ejaculation at all
- Post-ejaculatory pain, involves pain in the tip or shaft of the penis, perineum, or scrotum after ejaculation
- Penile, scrotal, and perineal pain, burning or itching
- Climacturia, involves leaking urine with orgasm
- Sexual dysfunction is common in diagnoses such as Chronic Pelvic Pain Syndrome and Pudendal Neuralgia
Causes of Sexual Dysfunction in People with Penises
Pelvic floor dysfunction is a source of sexual dysfunction. It can arise during the following scenarios:
- Pelvic Pain Syndromes, associated with pelvic floor dysfunction (Pudendal Neuralgia, Chronic Pelvic Pain Syndrome)
- Post-Surgical Effects, prostatectomy, pelvic floor reconstruction, genital surgeries (gender-affirming surgery)
- Medications, specifically medications that affect sexual function or arousal
- Cardiovascular Disease, leading to erectile dysfunction
- Jelqing, a manual stretching exercise is sometimes used to enhance penile size
- Genital Mutilation or Cutting, contributing to pelvic pain and dysfunction
Learn more about Male Pelvic Pain
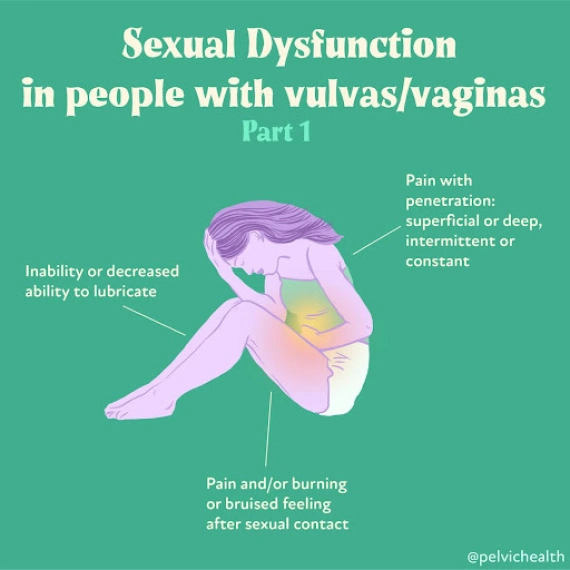
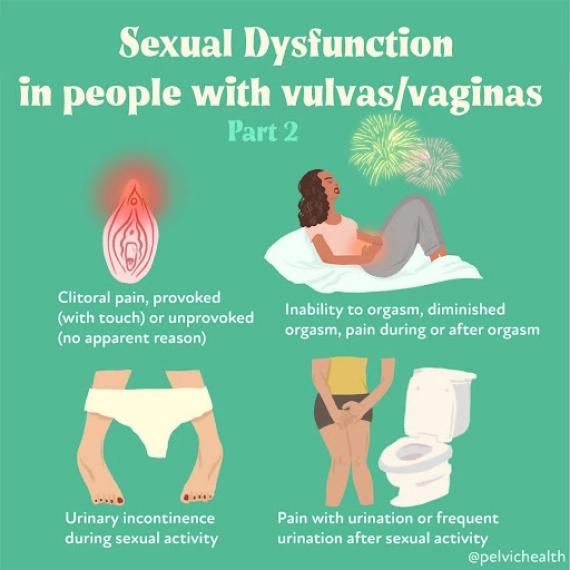
Symptoms of Sexual Dysfunction in People with Vulvas
- Pain with vaginal penetration, involves discomfort during superficial vaginal insertion or deep penetration or both
- Decreased lubrication, involves the inability or reduced ability to lubricate
- Clitoral pain, involves hypersensitivity or pain with touch, persistent genital arousal disorder, provoked or unprovoked
- Pain and/or burning before, during, or after sexual activity, which involves lingering pain or burning sensation following sexual contact
- Inability to orgasm, involves reduced or absent ability to achieve orgasm
- Climacturia, involves leaking urine with orgasm
Causes of Sexual Dysfunction in People with Vulvas
- Pelvic floor dysfunction is a primary cause of sexual dysfunction and commonly arises during the following scenarios
- Sexual dysfunction and pain is common in diagnoses such as Endometriosis, Vulvodynia, Vaginismus, Vestibulodynia, GSM, GSL, Interstitial Cystitis and Pudendal Neuralgia
- Post-surgical effects, including episiotomy, vestibulectomy, mesh excision, pelvic floor reconstruction, obstetric repair
- Hormonal deficiencies, including GSM, GSL, hormonal mediated vestibulodynia in response to medications such as OCPs, GnRh agonists, acne medications
Learn more about Female Pelvic Pain
Treatment for Sexual Dysfunction
Treatment for sexual dysfunction includes pelvic therapy and possibly medical management if hormonal deficiencies and/or infections are problematic. A trained therapist will assess your pelvic floor and girdle muscles, and neuromuscular control and will evaluate biomechanics and strength, length, and endurance as well as peripheral nerves and the central nervous system. Treatment often involves manual therapy, neuromuscular re-education and home exercises, patient education, and help with plan of care coordination when other providers are also involved.
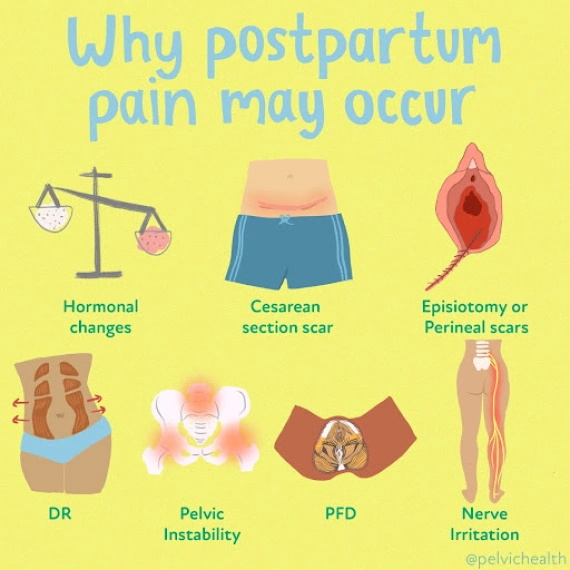
Postpartum Sexual Dysfunction Symptoms
- Genitourinary Syndrome Of Lactation (GSL), where hormonal deficiencies can cause superficial vulvar pain
- Vulvovaginal and perineal pain, which is pain in the perineum from episiotomy, levator ani avulsion, or obstetric instrument trauma
- Diminished or absent orgasm, which is the reduced ability to experience orgasm
- Incontinence during orgasm, involves leaking urine during sexual activity or orgasm
- Painful sex, which involves discomfort or pain during intercourse
Causes of Postpartum Sexual Dysfunction
- Pelvic floor dysfunction and GSL are the two main causes of postpartum sexual dysfunction
- Pelvic trauma from childbirth, including perineal tears or episiotomies
- Postpartum healing delays
Treatment for Postpartum Sexual Dysfunction
Treatment for sexual dysfunction includes pelvic therapy and possibly medical management if hormonal deficiencies and/or infections are problematic. A trained therapist will assess your pelvic floor and girdle muscles, and neuromuscular control and will evaluate biomechanics and strength, length, and endurance as well as peripheral nerves and the central nervous system. Treatment often involves manual therapy, neuromuscular re-education and home exercises, patient education, and help with plan of care coordination when other providers are also involved.
Genitourinary Syndrome of Menopause Symptoms
- Hormonal deficiencies and pelvic floor dysfunction are sources of irritative bladder and vulvovaginal pain in menopause
- Decreased lubrication, which is the inability or difficulty lubricating
- Pain with penetration, which is pain and/or tearing during vaginal penetration
- Clitoral pain
- Diminished or absent orgasm, involves reduced or absent ability to achieve orgasm
- Urinary urgency, frequency, hesitancy, pain
- Recurrent vaginal and urinary tract infections
Causes of Menopausal Sexual Dysfunction
- Pelvic floor dysfunction
- Decreased hormone levels
- Pelvic Surgeries
Treatment for Menopausal Sexual Dysfunction
Treatment for menopausal sexual dysfunction includes pelvic therapy and possibly medical management if hormonal deficiencies and/or infections are problematic. A trained therapist will assess your pelvic floor and girdle muscles, and neuromuscular control and will evaluate biomechanics and strength, length, and endurance as well as peripheral nerves and the central nervous system. Treatment often involves manual therapy, neuromuscular re-education and home exercises, patient education, and help with plan of care coordination when other providers are also involved.
4. Musculoskeletal Pelvic Pain Symptoms
Musculoskeletal pelvic pain is another common issue associated with pelvic floor dysfunction. This type of pain can be caused by muscle imbalances, joint dysfunction, or nerve entrapment in the pelvic region. It is important to note that pelvic floor dysfunction causes urinary, bowel and sexual dysfunction listed above and below. In addition to the interruption to these normal daily function people may also feel provoked pain in the trunk and pelvis as result of pelvic floor dysfunction.
Symptoms can include:
- Vulvovaginal or Penile/Scrotal Pain, involves pain or discomfort in the genital region (provoked or unprovoked)
- Anal pain
- Pelvic Girdle Pain, involves pain around the pelvic bones or joints
- Sitting Pain, involves discomfort in the genitopelvic area and bony pelvis when attempting to sit or after prolonged sitting
- Exercise or clothing intolerance, involves difficulty exercising or wearing tight clothing due to pelvic pain or exacerbation of urinary, bowel, or sexual symptoms
Causes of Musculoskeletal Pelvic Pain
- Pelvic floor muscle tightness, weakness, discoordination issues
- Viscro-somatic reflex issues, such as in response to visceral diseases or infections
- Orthopedic injuries or traumas, involving hip dysfunction, sacro-iliac joint dysfunction, piriformis syndrome, leg length discrepancy
- Peripheral neuralgias, such as pudendal neuralgia, ilioinguinal or genitofemoral neuralgia, sciatica, etc
- Diseases such as Chronic Pelvic Pain Syndrome, Endometriosis, Vulvodynia, Vaginismus, Vestibulodynia, Interstitial Cystitis/painful Bladder Syndrome, Pudendal Neuralgia
Treatment for Musculoskeletal Pelvic Pain
Pelvic floor physical and occupational therapy specialists can provide significant relief for those experiencing musculoskeletal pelvic pain. Treatment typically focuses on individualized impairments to address muscle, connective tissue, biomechanical and peripheral nerve, and central nervous system dysfunction.
5. Symptoms of Pudendal and Pelvic Neuralgias
Pelvic floor physical and occupational therapy specialists can provide significant relief for those experiencing musculoskeletal pelvic pain. Treatment typically focuses on individualized impairments to address muscle, connective tissue, biomechanical and peripheral nerve, and central nervous system dysfunction.
The term ‘neuralgia’ means neuropathic pain in the distribution of a nerve. Symptoms of pudendal neuralgia include:
- Burning, shooting, stabbing pain in the genitals, perineum, or anus
- Urinary urgency, frequency, burning before, during, or after urination
- Pain before, during, or after bowel movements
- Pain before, during, or after sexual activity and orgasm
- Symptoms are worse when sitting versus standing or lying down
- Symptoms can be provoked by trunk flexion, hip flexion, external rotation of the hip, and certain exercises/activities such as squats, lunges, walking uphill, and sitting
Multiple nerves innervate the pelvic region, including the list below. The symptoms of pudendal neuralgia (including burning, shooting, or stabbing in pain) can occur in some or all of the structures the involved nerve supplies sensation to.
- Ilioinguinal Nerve
- Genitofemoral Nerve
- Illiohypogastric Nerve
- Posterior Femoral Cutaneous Nerve
- Sciatic Nerve
- Obturator Nerve
- Pudendal Nerve
Pudendal neuralgia is a condition that causes pelvic pain and can lead to issues with urination, bowel movements, and sexual function. The pudendal nerve originates from sacral nerve roots two, three, and four and takes a complex route through the pelvis. This route includes the pelvic floor muscles, sacrotuberous and sacrospinous ligaments, and Alcock’s Canal. Along its path, the nerve splits into branches, making sharp angles and turns, which increases its risk of injury.
The pudendal nerve’s sensory coverage includes the vulva (clitoris, labia major/minora, vestibule), the penis and scrotum, the last third of the urethra and rectum, the anal and urinary sphincters, the perineum, and pelvic floor muscles. It is a unique mixed nerve, meaning it contains sensory, motor, and autonomic fibers. These components allow it to provide feeling, muscle movement, and voluntary and involuntary control of urinary, bowel, sexual function and muscle activation.
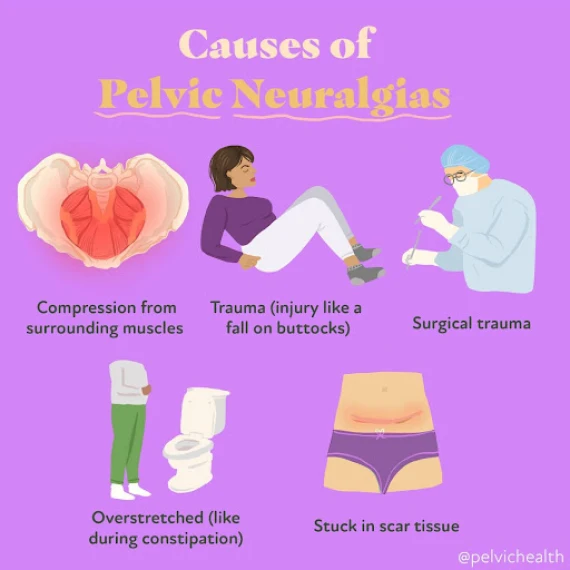
Causes of Pudendal and Pelvic Neuralgias
Symptoms of neuralgia occur when the nerve is compromised in a manner that interrupts its ability to slide, glide, and move normally. Common causes of pelvic neuralgias include:
- Surgical scars from hernia repairs, cesarean section, laparoscopic abdominal and pelvic surgeries
- External trauma such as car accidents or falls
- Musculoskeletal and joint dysfunction
- Hernias
The pudendal nerve has a more complicated course than other pelvic nerves, making it more prone to injury. The aponeurosis (a flat, strong layer of connective tissue) of the obturator internus muscles forms a fascial canal (a tunnel made of connective tissue) called Alcock’s Canal, which houses a main branch of the pudendal nerve. Common causes of pudendal neuralgia include:
- Obturator Internus, Piriformis, and/or pelvic floor dysfunction
- Altered lumbo-pelvic-hip mechanics
- Compression issues (sitting, cycling, horseback riding)
- Tension issues (constipation, childbirth, heavy weight lifting involving squats/lunges)
- Surgical insult (pelvic organ prolapse repair, prostatectomy)
Treatment of Pudendal and Pelvic Neuralgias
Most cases of pelvic and pudendal neuralgias have a neuro-muscular pelvic floor and girdle component. Therefore, pelvic floor physical or occupational therapy should always be offered as a first-line treatment for these syndromes. Because these syndromes affect urinary, bowel, and sexual dysfunction as well as daily comfort and ability to perform professional and recreational activities, interdisciplinary care that includes the following treatments can be the most effective:
- Pelvic floor physical or occupational therapy
- Pharmacologic management with a pain management doctor
- Procedural interventions (nerve blocks, botox injections to surrounding dysfunctional muscles, regenerative injections such as PRP or stem cells, dry needling)
- Pain Science education and stress management strategies
- Temporary lifestyle modifications
- Surgical intervention in cases of suspected entrapment
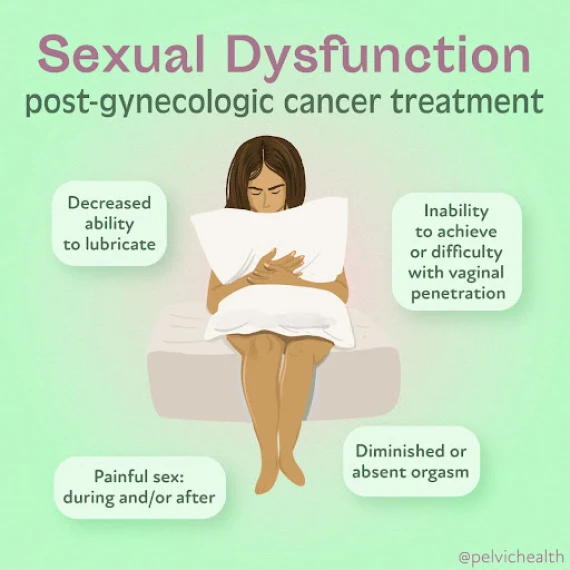
Post-Gynecologic Cancer Treatment Symptoms
- Pelvic pain, involves persistent discomfort or sharp pain in the pelvic region
- Urinary symptoms, involves urinary urgency, frequency, incontinence, or difficulty emptying the bladder
- Bowel symptoms, involves constipation, fecal incontinence, or painful bowel movements
- Pain with penetration, involves discomfort or pain during vaginal penetration or other sexual activities
- Vaginal dryness or tightness, involves reduced lubrication or sensation of vaginal constriction
- Decreased orgasmic function, involves difficulty or inability to achieve orgasm
- Muscle weakness or spasms, involves weakness in the pelvic floor muscles or painful spasms
- Pelvic heaviness or pressure, involves a sensation of fullness or pressure in the pelvis
- Scar pain, involves hypersensitivity or discomfort around surgical or radiation treatment sites
Post-Gynecologic Cancer Treatment Causes of Pelvic Pain
- Surgical effects, such as scar tissue formation, altered anatomy, or nerve damage from procedures like hysterectomy, oophorectomy, or lymph node removal
- Radiation therapy, involving pelvic floor tissue damage, fibrosis, or inflammation due to radiation exposure
- Hormonal changes, decreased estrogen levels causing vaginal tissue compromise or genitourinary syndrome of menopause (GSM)
- Chemotherapy side effects, which impact tissue health and muscle function
- Pelvic muscle overactivity, involving muscle tension or spasms triggered by pain or trauma from treatment
- Nerve damage, the injury to pelvic nerves during surgery or radiation
- Psychological factors, including anxiety, depression, or PTSD related to cancer diagnosis and treatment
- Lymphedema, swelling and discomfort in the pelvic area due to lymphatic damage
- Adhesions, internal scar tissue causing restricted movement and pain
Post-Gynecologic Cancer Treatment Pain Treatment
- Pelvic floor Physical or Occupational Therapy is warranted after cancer treatment
- Therapies may include manual therapy, dilator therapy, neuromuscular re-education, homes exercise program development, patient education
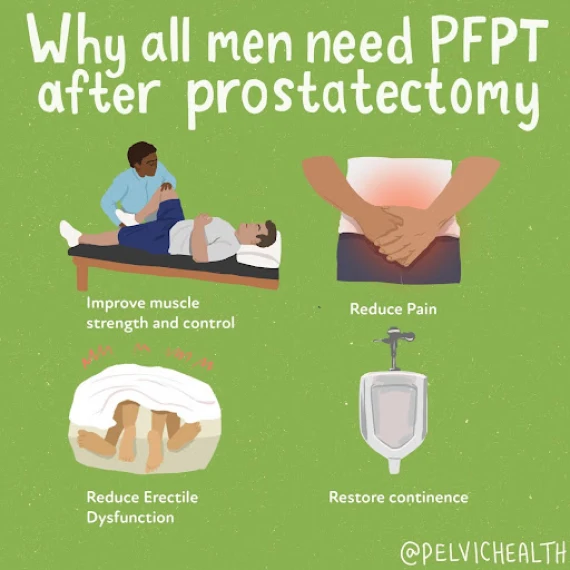
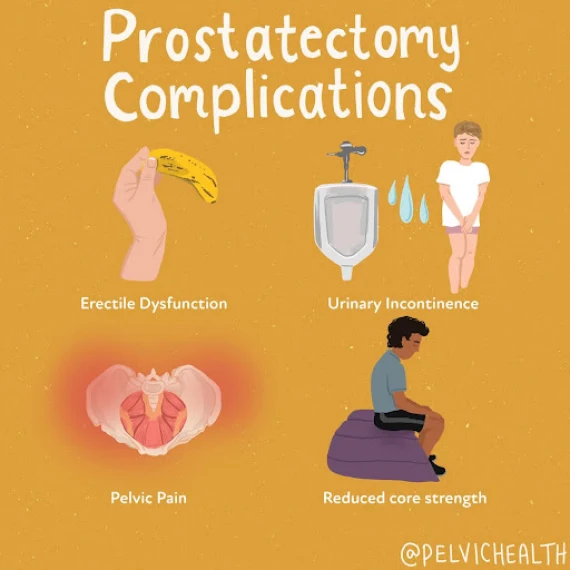
Post-Prostatectomy Symptoms
- Urinary incontinence
- Urinary urgency, frequency, nocturia
- Erectile Dysfunction
- Pelvic and Perineal Pain
- Diastasis Recti
Causes of Post-Prostatectomy
Surgical procedures such as:
- Simple prostatectomy
- Radical prostatectomy
- Robotic-assisted prostatectomy
- Laprascopic prostatectomy
- Single-port radical prostatectomy
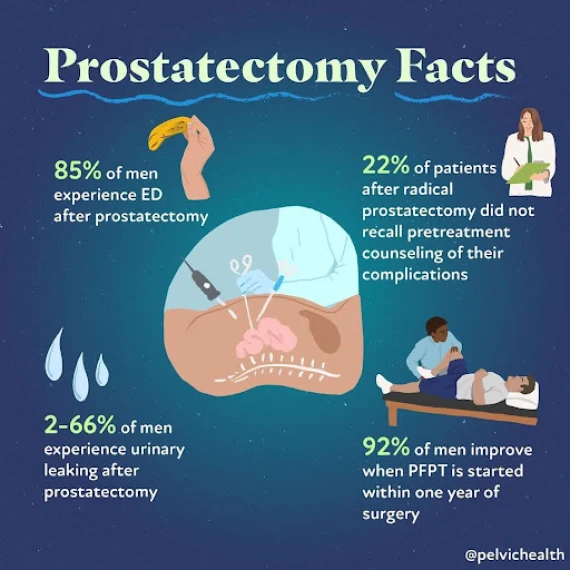
Treatments for Post-Prostatectomy
Research shows that men who undergo pelvic floor prehab (physical or occupational therapy prior to surgery) have a reduced risk of urinary incontinence and erectile dysfunction. Studies also show that men who have post-prostatectomy rehab within one year of surgery have significantly less urinary leakage and sexual dysfunction. Treatment includes:
- Manual therapy
- Neuromuscular re-education
- Home Exercise Program Development
- Patient Education
What To Expect During Your Appointment
When you arrive for your first appointment at PHRC, our primary goal is to understand your pelvic health concerns. During this initial consultation, your therapist will ask about your medical history, including any previous pelvic surgeries, childbirth experiences, or conditions that might contribute to symptoms such as urinary issues, bowel dysfunction, sexual pain, musculoskeletal pelvic pain, or pudendal and pelvic neuralgias. This thorough discussion will help us determine the best approach for your care. We are also looking to understand what providers, if any, are currently involved in your care and listening for issues that might need additional medical management.
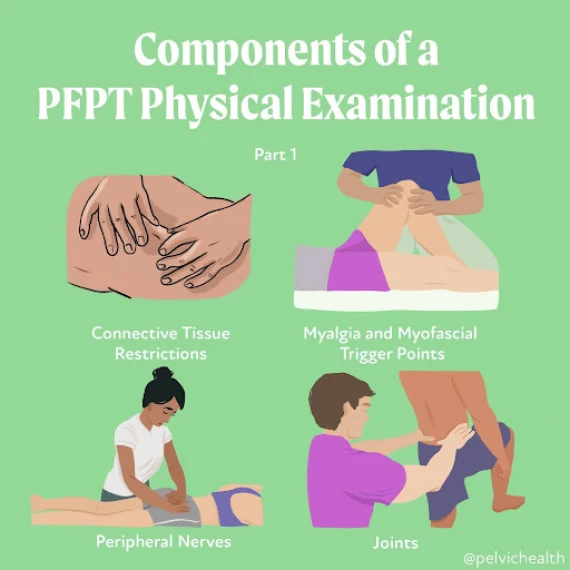
A physical examination will follow, where your pelvic floor physical or occupational therapist will evaluate the muscles, tissues, and nerves in the trunk, pelvic girdle, and pelvic floor muscles. This examination may include checking for muscle and connective tissue pain, tightness, weakness, or imbalances that could be affecting your pelvic floor function. We also assess how well your muscles coordinate during breathing and movement, which is helpful for managing functions like urination, bowel movements, and sexual activity.
Once the physical examination is complete, your pelvic floor physical or occupational therapist will provide you with an assessment. This assessment links your history to your current symptoms and findings from the physical examination. It is important for us to develop a working theory as to how your pain and dysfunction began and which physical impairments are contributing. Often multiple factors are involved, both in terms of the musculoskeletal system and possibly other symptoms as well.
Part of the assessment involves setting both short-term and long-term goals. Short-term goals focus on specific issues, like reducing pelvic floor muscle pain to ease discomfort during sex or improving pelvic floor muscle control to address urinary symptoms. Long-term goals are more focused on overall function, such as helping the patient have enjoyable, pain-free intercourse or reducing the need to urinate more than eight times a day without pain or hesitation.
You and your therapist will work together to create a treatment plan, deciding how often and for how long you’ll have sessions. This plan will guide you toward relieving your symptoms and reaching both your short-term and long-term goals.
The in-person clinical treatment plan is usually weekly and includes manual therapy, neuromuscular re-education, patient education, therapeutic exercise, and home exercise program development. Short-term goals can usually be achieved in 12 weeks. Treatment plans are dynamic and will evolve over time as impairments reduce and improvement is made. As therapists, we are afforded more time with our patients than our medical colleagues are, therefore, we will also communicate with other providers to ensure medical management is also organized and coordinated with the plan of care at PHRC.
Find Relief From PHRC
At PHRC, our goal is to provide compassionate and comprehensive care to help you manage and overcome pain from pelvic floor dysfunction. By understanding the underlying causes and providing targeted treatments, our goal is to improve your quality of life and restore your health.
We also recognize the challenges some people might face in accessing in-person care, which is why we offer virtual sessions through telehealth after your initial consultation. These sessions allow for continuity of care and accessibility for those unable to travel to one of our clinics.