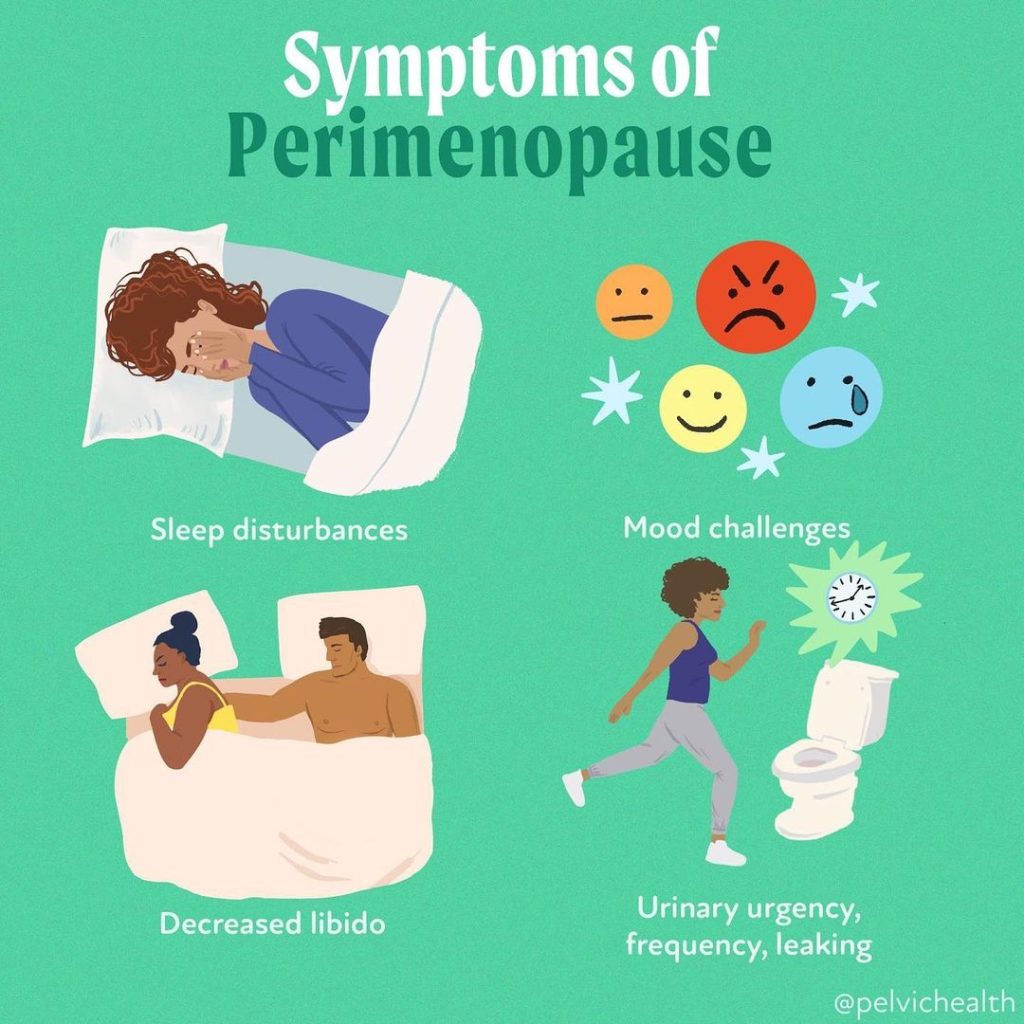
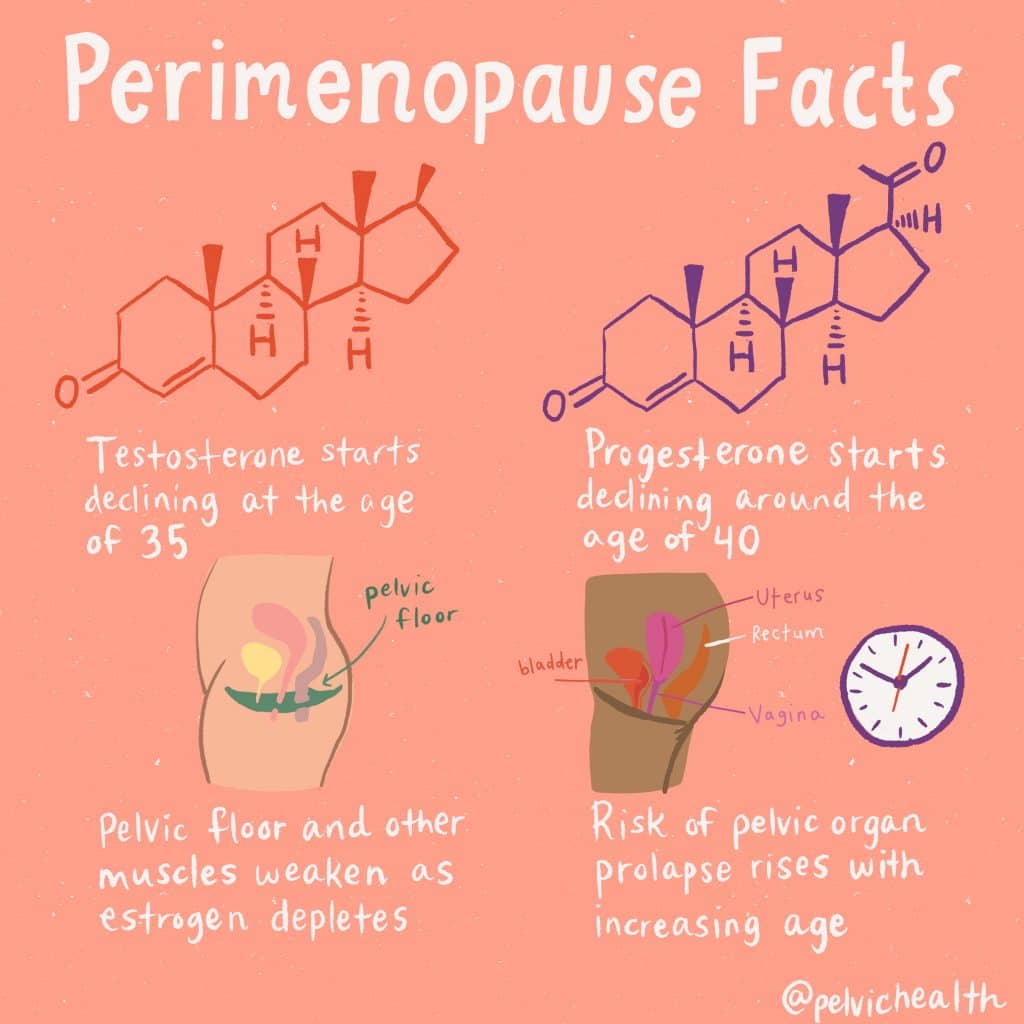
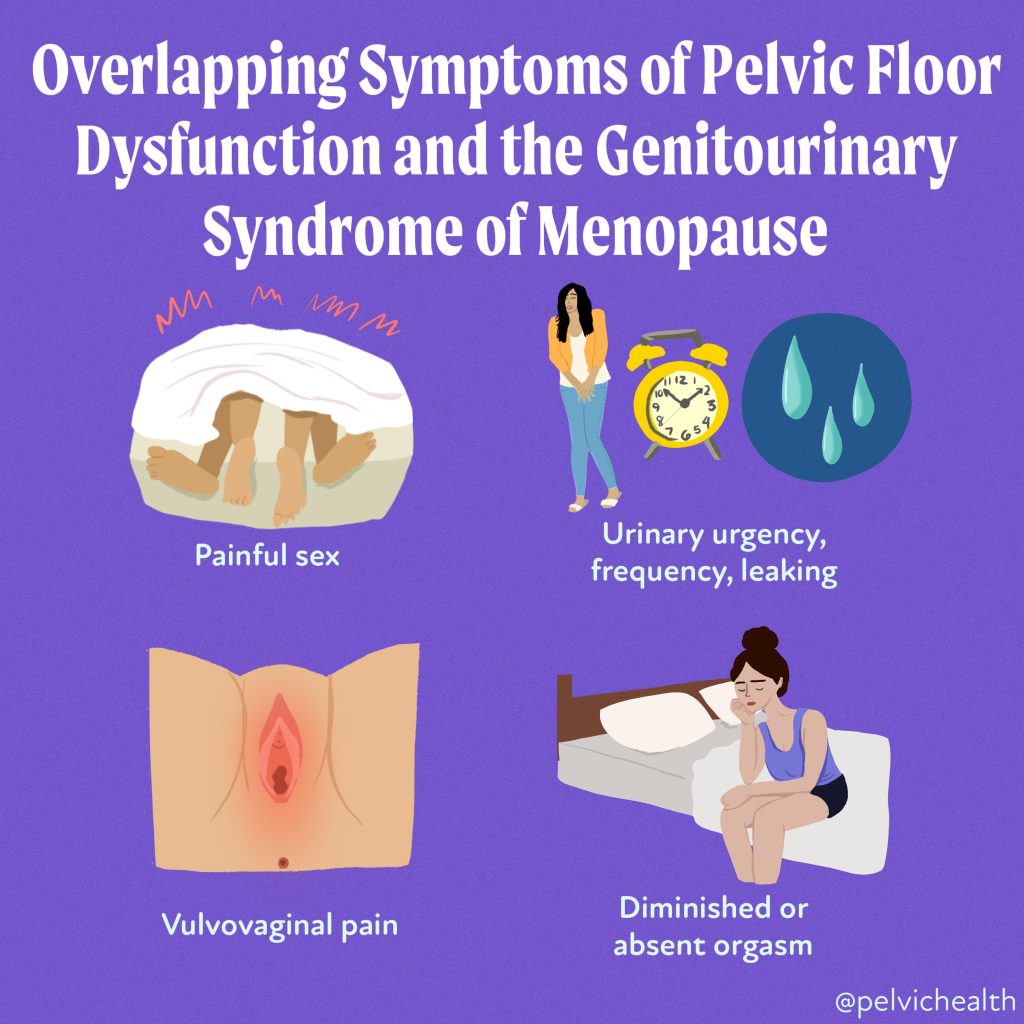
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

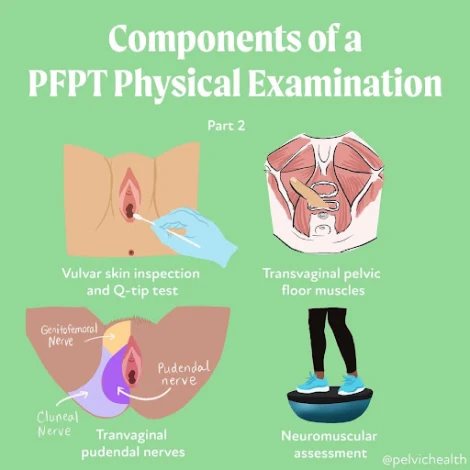
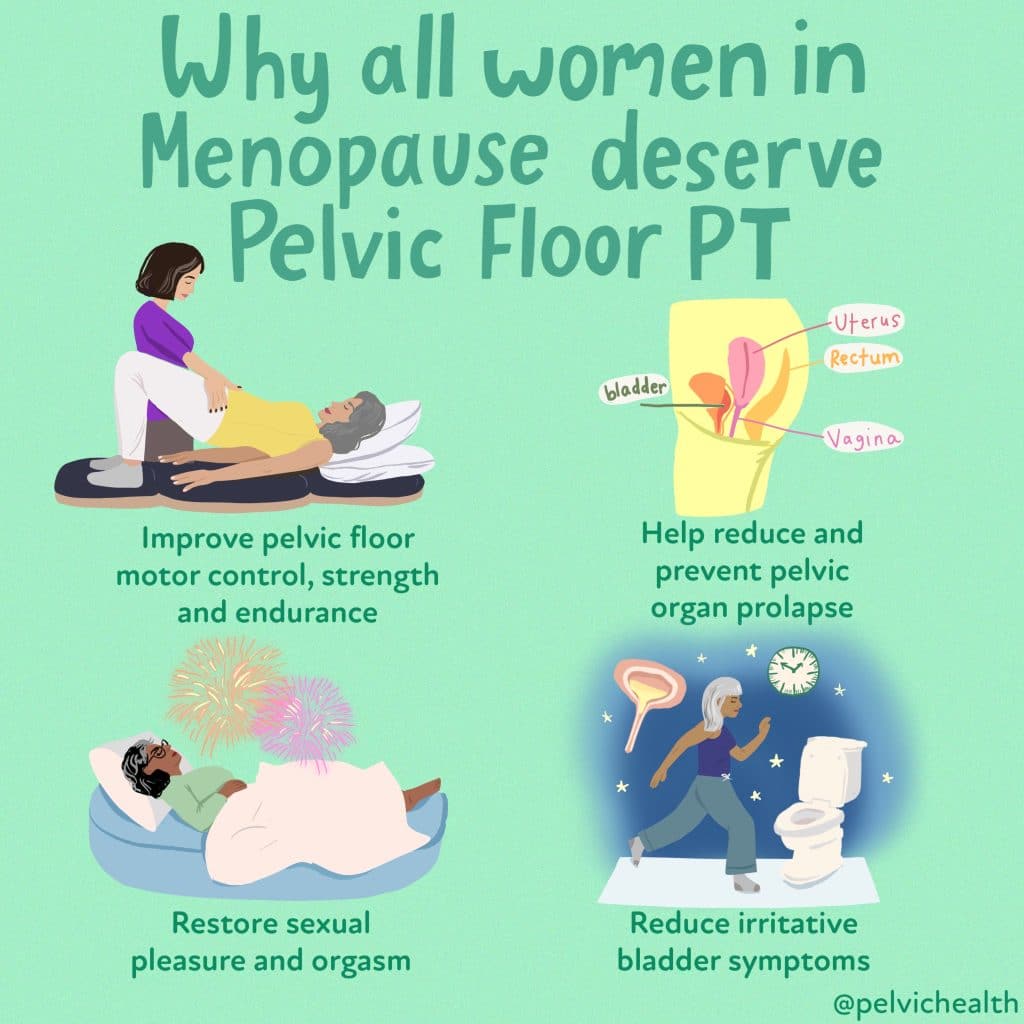
An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
Table of Contents
-
.
-
.
-
.
-
.
-
.
-
.
-
.
Pudendal and Pelvic Neuralgias Symptoms, Causes, and Treatments
-
.
-
.
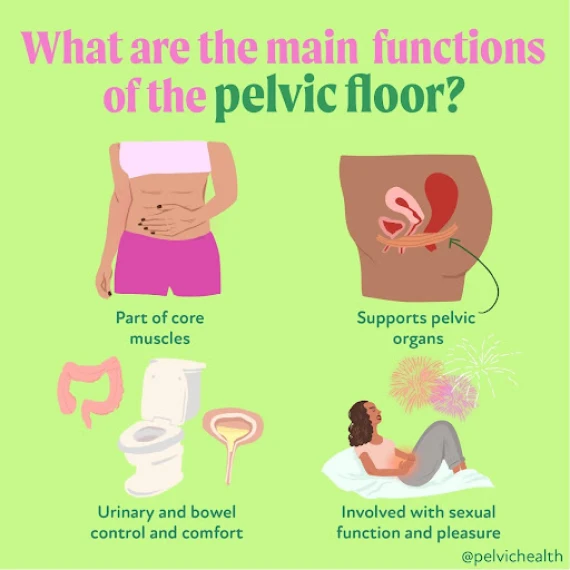
Pelvic floor muscles play an integral role in urinary, bowel, and sexual functioning. Additionally, they function as part of our core and support our pelvic organs. They are part of our pelvic girdle (the bones that support your hips and connect your legs to your spine). Most people do not know they even have pelvic floor muscles until issues arise and they begin to search for help and care. Because the nature of the symptoms can fall under the umbrella of urologic, gynecologic, and colorectal disciplines, people with symptoms often seek out the help of these providers. Recent studies have shown that medical schools do not currently include pelvic floor dysfunction training in their curricula, which is leading to diagnostic confusion and delays for suffering patients.
Pelvic floor dysfunction is a neuromuscular condition that must involve the care of a skilled pelvic floor physical or occupational therapist to establish a proper diagnosis and effective treatment plan. The therapists at the Pelvic Health and Rehabilitation Center have undergone extensive training in the management of pelvic floor dysfunction and are prepared and ready to help.
What is the Pelvic Floor?
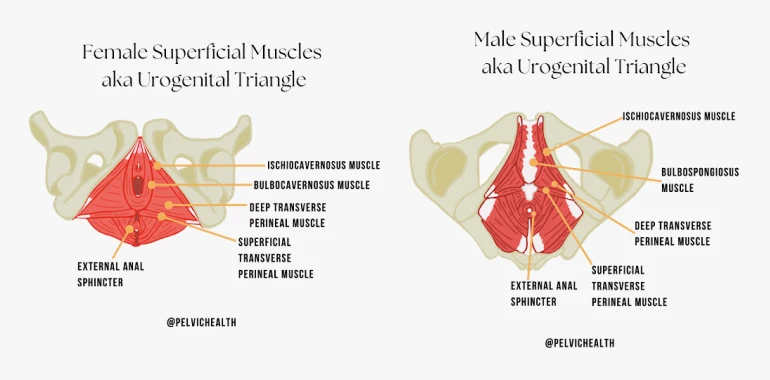
The pelvic floor muscles are bowl-like muscles inside the pelvic girdle. They attach at the pelvic girdle. They are loosely grouped as superficial or deep.
The superficial muscles, also known as the urogenital diaphragm, include the bulbospongiosus, ischiocavernosus, superficial and deep transverse perineal muscles, and the urethral and anal sphincter muscles.
The deep layer consists of the levator ani muscle group, which includes the pubococcygeus, puborectalis, iliococcygeus, and coccygeus.
Additionally, the obturator internus and piriformis muscles are external rotators of the hip and also have portions of their muscle bellies that communicate with the pelvic floor muscles. While these two muscles are external hip rotators, they also play a role in pelvic floor muscle function and dysfunction.
The pelvic floor muscles have unique innervation (nerve supply) in that they reflexively work with our core, bladder, and bowel function. However, we also have the ability to override the autonomic control. These muscles are always active because of these reflexive loops. When the muscles become impaired, they might be too tight, too weak, or have dysfunctional neuromuscular control. When this happens, people can experience bladder, bowel, sexual dysfunction, pelvic organ prolapse, and pelvic floor, girdle, hip, and lower back pain.
Symptoms of Pelvic Floor Dysfunction
Pelvic floor dysfunction can manifest in a range of symptoms, which generally fall into five categories: urinary, bowel, sexual dysfunction, musculoskeletal, and/or neuropathic pelvic pain.
Historically, pelvic floor dysfunction was oversimplified into what was called ‘low-tone’ and ‘high-tone’ pelvic floor disorders.
The ‘low-tone’ pelvic floor disorders included symptoms such as urinary and fecal incontinence (loss of bladder or bowel control), pelvic organ prolapse (when pelvic organs drop from their normal position), and post-prostatectomy and other surgical repairs, and are associated with lifetime milestones involving physiologic change such as the post-partum period (the time after childbirth) and perimenopause and menopause. These symptoms and time frames leave the pelvic floor muscles vulnerable to impaired neuromuscular control (disruption in the communication between nerves and muscles), which can result in weakness and poor endurance.
The ‘high-tone’ pelvic floor disorders were associated with symptoms of urogenital pain (pain in the urinary or genital region), irritative bladder symptoms (frequent or urgent need to urinate), and sexual pain and were more commonly identified in adolescents through aging adults of all sexes. While aging adults often suffer from sexual pain disorders, early pelvic pain research separated out premenopausal and menopausal women to show that muscular dysfunction and sexual pain can exist in premenopausal years as well.
However, emerging research on pelvic floor disorders has broadened our understanding of the syndrome, and we now understand people with any pelvic floor diagnosis or cluster of symptoms can have muscle dysfunction that includes elevated or reduced EMG findings (or tone), impaired neuromuscular control (disruption in nerve-to-muscle signaling), impaired lumbo-pelvic-hip biomechanics (issues with how the lower back, pelvis, and hips move together), muscle pain, weakness and endurance challenges.
Problems in how the body functions can happen at any age and in all sexes. Appropriate interdisciplinary care that includes pelvic floor physical and occupational therapy allows us to collaborate to establish the proper differential diagnosis and care plan.
1. Urinary Symptoms
Bladder changes are a common symptom of pelvic floor dysfunction. These symptoms can vary in severity from barely noticeable to severely limiting. Examples of urinary symptoms that are associated with pelvic floor dysfunction are listed below. Patients may experience some of these symptoms or a combination of multiple symptoms on this list.
- Stress Incontinence, which is the involuntary leaking of urine when coughing, laughing, sneezing, or during exercise, this is also common after pelvic surgeries, including prostatectomy
- Urge Incontinence, which is the involuntary urinary leaking when the urge strikes, such as putting the key in the front door to head to the bathroom
- Mixed Incontinence, which is a combination of both stress and urge incontinence
- Bladder pain, involves discomfort or pain in the bladder region, upon bladder filling or without bladder filling
- Urethral pain, which can occur unprovoked (spontaneous) or in a provoked situation such as in response to touch, urination, or clothing or sitting. Urethral pain can also occur before, during, and after urination
- Urgency/frequency, which is the feeling of needing to urinate urgently, even when the bladder isn’t full, can lead to frequency which refers to an increased number of trips to the bathroom
- Urinary hesitancy, involves difficulty starting the urine stream or having a slow flow
- Climacturia, which is leaking urine with orgasm
Causes of Urinary Issues/Bladder Dysfunction
Tight, weak, and discoordinated pelvic floor and girdle muscles can cause urinary dysfunction. There are a number of reasons pelvic floor muscles can become dysfunctional, key reasons are listed below.
- Recurrent Urinary Tract Infections (UTIs), urinary tract infections are considered recurrent if someone has more than 2 in a 6-month period or more than 3 in one year, the bladder irritation from the infection triggers the viscero-somatic reflex and pelvic floor dysfunction can occur and can continue to mimic the symptoms of a UTI in the absence of infection
- Hormonal deficiencies, specifically the Genitourinary Syndrome of Menopause (GSM), the Genitourinary Syndrome of Lactation (GSL), and Hormonally Mediated Vestibulodynia in premenopausal women can cause irritation of the vestibule, which houses the urethra, and these deficiencies also cause pelvic floor dysfunction
- Hormonally mediated vestibulodynia can be caused by medications that suppress free testosterone, including oral contraceptives, GnRH agonists, and acne medications
- Biomechanical or structural dysfunction, including hip dysfunction, sacroiliac joint dysfunction, piriformis syndrome, scoliosis, leg length discrepancy
- Pelvic Floor Dysfunction, involving tight, weak, or discoordinated pelvic muscles
- Pelvic Organ Prolapse, which occurs when the pelvic organs descend into the vaginal canal and cause urinary symptoms
- Endometriosis, constipation, and gastrointestinal distress or bloating, which cause increased pressure on the pelvic floor and bladder and can cause urinary symptoms
Treatment for Urinary Issues/Bladder Dysfunction
The American Urological Association published guidelines in 2011, 2014, and 2022 stating that manual pelvic floor physical and occupational therapy is the first-line treatment for people with irritative bladder symptoms associated with the diagnosis of Interstitial Cystitis/painful Bladder Syndrome. The International Continence Society also recommends physical and occupational therapy as first-line treatment for people with urinary leaking. Once lower urinary tract pathology is ruled out or being treated, an evaluation with a pelvic floor physical or occupational therapist is warranted.
A trained therapist will assess your pelvic floor and girdle muscles, neuromuscular control, and will evaluate biomechanics and strength, length, and endurance, as well as peripheral nerves and the central nervous system.
Treatment often involves manual therapy, neuromuscular re-education, home exercises, patient education, and help with plan of care coordination when other providers are also involved.
2. Bowel Symptoms
Bowel dysfunction can cause significant discomfort and distress. Many people experience symptoms like constipation, difficulty evacuating stool, anal pain, and/or fecal incontinence due to pelvic floor issues.
- Straining to evacuate stool, involves difficulty or pain when passing stool
- Constipation, involves infrequent or difficult bowel movements
- Fecal or gas leakage, which is involuntary leakage of stool or gas
- Hemorrhoids and fissures, which are painful, swollen veins in the rectum or tears in the anal lining
- Anal/Rectal pain, involves burning, itching, or pain before, during, or after bowel movements or spontaneous unprovoked pain, symptoms can also be triggered with exercise, sitting, or clothing
Causes of Bowel Symptoms
Bowel issues from pelvic floor dysfunction can result from:
- Medication-induced constipation, including opiates, mood stabilizers, oral contraceptives
- Pelvic Floor Muscle Dyssynergia, occurs when muscles are either too tight, too weak, or uncoordinated
- Peripheral nerve injuries, caused by childbirth, chronic straining, or surgical trauma
- Visceral-somatic consequences, which includes gastrointestinal issues such as IBS, Crohn’s disease, ulcerative colitis, SIBO (Small Intestinal Bacterial Overgrowth)
- Conditions like anal fissures and hemorrhoids, which are often caused by faulty bowel mechanics and are a sign of pelvic floor dysfunction (they are also painful and can cause further pelvic floor dysfunction and pain in response to the irritation from these tissues themselves)
Treatment for Bowel Issues
Pelvic floor physical and occupational therapy are key treatment options for bowel dysfunction. A pelvic floor physical or occupational therapist will assess the coordination and strength of the pelvic floor muscles and create a treatment plan focused on improving muscle control. Treatments might include exercises to improve coordination, manual therapy, and biofeedback to help regain control over bowel movements.
3. Sexual Dysfunction Symptoms
Sexual dysfunction is associated with pelvic floor dysfunction in all genders and ages.
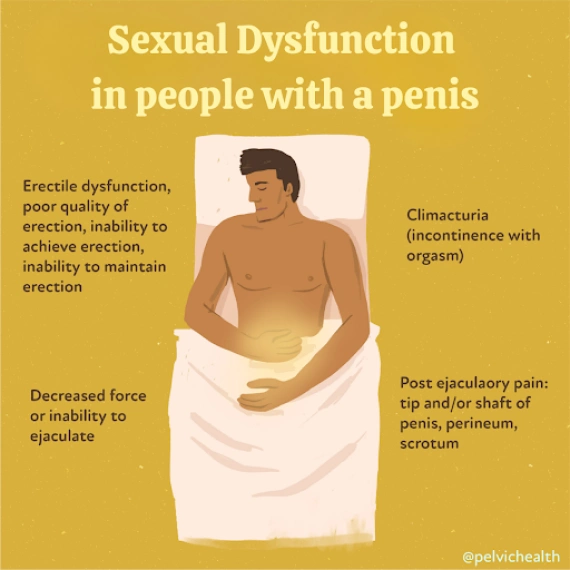
Symptoms of Sexual Dysfunction in People with Penises
- Erectile Dysfunction, involves poor quality, and inability to achieve or maintain an erection, which can occur in men of any age and is also a common complication after prostatectomy
- Premature Ejaculation, involves the inability to delay ejaculation
- Decreased Force or Inability to ejaculate, involves weak ejaculation or no ejaculation at all
- Post-ejaculatory pain, involves pain in the tip or shaft of the penis, perineum, or scrotum after ejaculation
- Penile, scrotal, and perineal pain, burning or itching
- Climacturia, involves leaking urine with orgasm
- Sexual dysfunction is common in diagnoses such as Chronic Pelvic Pain Syndrome and Pudendal Neuralgia
Causes of Sexual Dysfunction in People with Penises
Pelvic floor dysfunction is a source of sexual dysfunction. It can arise during the following scenarios:
- Pelvic Pain Syndromes, associated with pelvic floor dysfunction (Pudendal Neuralgia, Chronic Pelvic Pain Syndrome)
- Post-Surgical Effects, prostatectomy, pelvic floor reconstruction, genital surgeries (gender-affirming surgery)
- Medications, specifically medications that affect sexual function or arousal
- Cardiovascular Disease, leading to erectile dysfunction
- Jelqing, a manual stretching exercise is sometimes used to enhance penile size
- Genital Mutilation or Cutting, contributing to pelvic pain and dysfunction
Learn more about Male Pelvic Pain
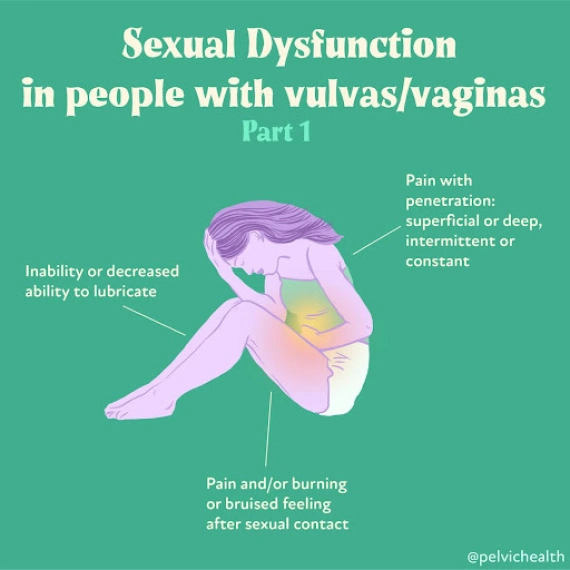
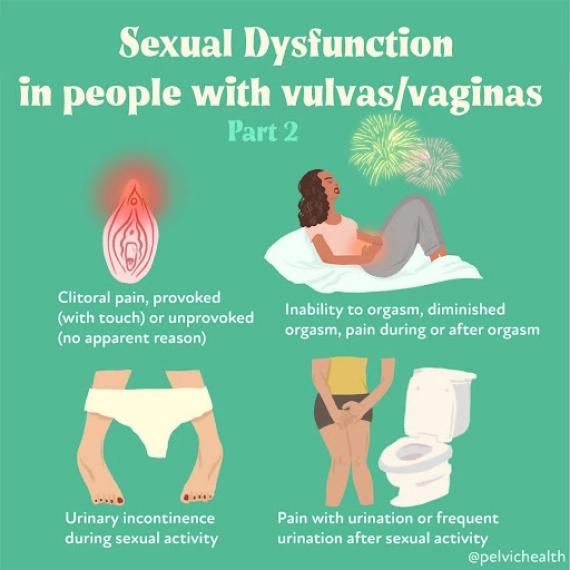
Symptoms of Sexual Dysfunction in People with Vulvas
- Pain with vaginal penetration, involves discomfort during superficial vaginal insertion or deep penetration or both
- Decreased lubrication, involves the inability or reduced ability to lubricate
- Clitoral pain, involves hypersensitivity or pain with touch, persistent genital arousal disorder, provoked or unprovoked
- Pain and/or burning before, during, or after sexual activity, which involves lingering pain or burning sensation following sexual contact
- Inability to orgasm, involves reduced or absent ability to achieve orgasm
- Climacturia, involves leaking urine with orgasm
Causes of Sexual Dysfunction in People with Vulvas
- Pelvic floor dysfunction is a primary cause of sexual dysfunction and commonly arises during the following scenarios
- Sexual dysfunction and pain is common in diagnoses such as Endometriosis, Vulvodynia, Vaginismus, Vestibulodynia, GSM, GSL, Interstitial Cystitis and Pudendal Neuralgia
- Post-surgical effects, including episiotomy, vestibulectomy, mesh excision, pelvic floor reconstruction, obstetric repair
- Hormonal deficiencies, including GSM, GSL, hormonal mediated vestibulodynia in response to medications such as OCPs, GnRh agonists, acne medications
Learn more about Female Pelvic Pain
Treatment for Sexual Dysfunction
Treatment for sexual dysfunction includes pelvic therapy and possibly medical management if hormonal deficiencies and/or infections are problematic. A trained therapist will assess your pelvic floor and girdle muscles, and neuromuscular control and will evaluate biomechanics and strength, length, and endurance as well as peripheral nerves and the central nervous system. Treatment often involves manual therapy, neuromuscular re-education and home exercises, patient education, and help with plan of care coordination when other providers are also involved.
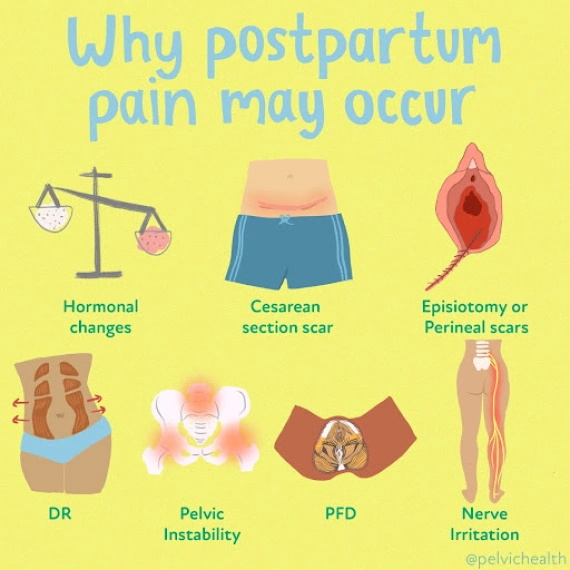
Postpartum Sexual Dysfunction Symptoms
- Genitourinary Syndrome Of Lactation (GSL), where hormonal deficiencies can cause superficial vulvar pain
- Vulvovaginal and perineal pain, which is pain in the perineum from episiotomy, levator ani avulsion, or obstetric instrument trauma
- Diminished or absent orgasm, which is the reduced ability to experience orgasm
- Incontinence during orgasm, involves leaking urine during sexual activity or orgasm
- Painful sex, which involves discomfort or pain during intercourse
Causes of Postpartum Sexual Dysfunction
- Pelvic floor dysfunction and GSL are the two main causes of postpartum sexual dysfunction
- Pelvic trauma from childbirth, including perineal tears or episiotomies
- Postpartum healing delays
Treatment for Postpartum Sexual Dysfunction
Treatment for sexual dysfunction includes pelvic therapy and possibly medical management if hormonal deficiencies and/or infections are problematic. A trained therapist will assess your pelvic floor and girdle muscles, and neuromuscular control and will evaluate biomechanics and strength, length, and endurance as well as peripheral nerves and the central nervous system. Treatment often involves manual therapy, neuromuscular re-education and home exercises, patient education, and help with plan of care coordination when other providers are also involved.
Genitourinary Syndrome of Menopause Symptoms
- Hormonal deficiencies and pelvic floor dysfunction are sources of irritative bladder and vulvovaginal pain in menopause
- Decreased lubrication, which is the inability or difficulty lubricating
- Pain with penetration, which is pain and/or tearing during vaginal penetration
- Clitoral pain
- Diminished or absent orgasm, involves reduced or absent ability to achieve orgasm
- Urinary urgency, frequency, hesitancy, pain
- Recurrent vaginal and urinary tract infections
Causes of Menopausal Sexual Dysfunction
- Pelvic floor dysfunction
- Decreased hormone levels
- Pelvic Surgeries
Treatment for Menopausal Sexual Dysfunction
Treatment for menopausal sexual dysfunction includes pelvic therapy and possibly medical management if hormonal deficiencies and/or infections are problematic. A trained therapist will assess your pelvic floor and girdle muscles, and neuromuscular control and will evaluate biomechanics and strength, length, and endurance as well as peripheral nerves and the central nervous system. Treatment often involves manual therapy, neuromuscular re-education and home exercises, patient education, and help with plan of care coordination when other providers are also involved.
4. Musculoskeletal Pelvic Pain Symptoms
Musculoskeletal pelvic pain is another common issue associated with pelvic floor dysfunction. This type of pain can be caused by muscle imbalances, joint dysfunction, or nerve entrapment in the pelvic region. It is important to note that pelvic floor dysfunction causes urinary, bowel and sexual dysfunction listed above and below. In addition to the interruption to these normal daily function people may also feel provoked pain in the trunk and pelvis as result of pelvic floor dysfunction.
Symptoms can include:
- Vulvovaginal or Penile/Scrotal Pain, involves pain or discomfort in the genital region (provoked or unprovoked)
- Anal pain
- Pelvic Girdle Pain, involves pain around the pelvic bones or joints
- Sitting Pain, involves discomfort in the genitopelvic area and bony pelvis when attempting to sit or after prolonged sitting
- Exercise or clothing intolerance, involves difficulty exercising or wearing tight clothing due to pelvic pain or exacerbation of urinary, bowel, or sexual symptoms
Causes of Musculoskeletal Pelvic Pain
- Pelvic floor muscle tightness, weakness, discoordination issues
- Viscro-somatic reflex issues, such as in response to visceral diseases or infections
- Orthopedic injuries or traumas, involving hip dysfunction, sacro-iliac joint dysfunction, piriformis syndrome, leg length discrepancy
- Peripheral neuralgias, such as pudendal neuralgia, ilioinguinal or genitofemoral neuralgia, sciatica, etc
- Diseases such as Chronic Pelvic Pain Syndrome, Endometriosis, Vulvodynia, Vaginismus, Vestibulodynia, Interstitial Cystitis/painful Bladder Syndrome, Pudendal Neuralgia
Treatment for Musculoskeletal Pelvic Pain
Pelvic floor physical and occupational therapy specialists can provide significant relief for those experiencing musculoskeletal pelvic pain. Treatment typically focuses on individualized impairments to address muscle, connective tissue, biomechanical and peripheral nerve, and central nervous system dysfunction.
5. Symptoms of Pudendal and Pelvic Neuralgias
Pelvic floor physical and occupational therapy specialists can provide significant relief for those experiencing musculoskeletal pelvic pain. Treatment typically focuses on individualized impairments to address muscle, connective tissue, biomechanical and peripheral nerve, and central nervous system dysfunction.
The term ‘neuralgia’ means neuropathic pain in the distribution of a nerve. Symptoms of pudendal neuralgia include:
- Burning, shooting, stabbing pain in the genitals, perineum, or anus
- Urinary urgency, frequency, burning before, during, or after urination
- Pain before, during, or after bowel movements
- Pain before, during, or after sexual activity and orgasm
- Symptoms are worse when sitting versus standing or lying down
- Symptoms can be provoked by trunk flexion, hip flexion, external rotation of the hip, and certain exercises/activities such as squats, lunges, walking uphill, and sitting
Multiple nerves innervate the pelvic region, including the list below. The symptoms of pudendal neuralgia (including burning, shooting, or stabbing in pain) can occur in some or all of the structures the involved nerve supplies sensation to.
- Ilioinguinal Nerve
- Genitofemoral Nerve
- Illiohypogastric Nerve
- Posterior Femoral Cutaneous Nerve
- Sciatic Nerve
- Obturator Nerve
- Pudendal Nerve
Pudendal neuralgia is a condition that causes pelvic pain and can lead to issues with urination, bowel movements, and sexual function. The pudendal nerve originates from sacral nerve roots two, three, and four and takes a complex route through the pelvis. This route includes the pelvic floor muscles, sacrotuberous and sacrospinous ligaments, and Alcock’s Canal. Along its path, the nerve splits into branches, making sharp angles and turns, which increases its risk of injury.
The pudendal nerve’s sensory coverage includes the vulva (clitoris, labia major/minora, vestibule), the penis and scrotum, the last third of the urethra and rectum, the anal and urinary sphincters, the perineum, and pelvic floor muscles. It is a unique mixed nerve, meaning it contains sensory, motor, and autonomic fibers. These components allow it to provide feeling, muscle movement, and voluntary and involuntary control of urinary, bowel, sexual function and muscle activation.
Causes of Pudendal and Pelvic Neuralgias
Symptoms of neuralgia occur when the nerve is compromised in a manner that interrupts its ability to slide, glide, and move normally. Common causes of pelvic neuralgias include:
- Surgical scars from hernia repairs, cesarean section, laparoscopic abdominal and pelvic surgeries
- External trauma such as car accidents or falls
- Musculoskeletal and joint dysfunction
- Hernias
The pudendal nerve has a more complicated course than other pelvic nerves, making it more prone to injury. The aponeurosis (a flat, strong layer of connective tissue) of the obturator internus muscles forms a fascial canal (a tunnel made of connective tissue) called Alcock’s Canal, which houses a main branch of the pudendal nerve. Common causes of pudendal neuralgia include:
- Obturator Internus, Piriformis, and/or pelvic floor dysfunction
- Altered lumbo-pelvic-hip mechanics
- Compression issues (sitting, cycling, horseback riding)
- Tension issues (constipation, childbirth, heavy weight lifting involving squats/lunges)
- Surgical insult (pelvic organ prolapse repair, prostatectomy)
Treatment of Pudendal and Pelvic Neuralgias
Most cases of pelvic and pudendal neuralgias have a neuro-muscular pelvic floor and girdle component. Therefore, pelvic floor physical or occupational therapy should always be offered as a first-line treatment for these syndromes. Because these syndromes affect urinary, bowel, and sexual dysfunction as well as daily comfort and ability to perform professional and recreational activities, interdisciplinary care that includes the following treatments can be the most effective:
- Pelvic floor physical or occupational therapy
- Pharmacologic management with a pain management doctor
- Procedural interventions (nerve blocks, botox injections to surrounding dysfunctional muscles, regenerative injections such as PRP or stem cells, dry needling)
- Pain Science education and stress management strategies
- Temporary lifestyle modifications
- Surgical intervention in cases of suspected entrapment
Post-Gynecologic Cancer Treatment Symptoms
- Pelvic pain, involves persistent discomfort or sharp pain in the pelvic region
- Urinary symptoms, involves urinary urgency, frequency, incontinence, or difficulty emptying the bladder
- Bowel symptoms, involves constipation, fecal incontinence, or painful bowel movements
- Pain with penetration, involves discomfort or pain during vaginal penetration or other sexual activities
- Vaginal dryness or tightness, involves reduced lubrication or sensation of vaginal constriction
- Decreased orgasmic function, involves difficulty or inability to achieve orgasm
- Muscle weakness or spasms, involves weakness in the pelvic floor muscles or painful spasms
- Pelvic heaviness or pressure, involves a sensation of fullness or pressure in the pelvis
- Scar pain, involves hypersensitivity or discomfort around surgical or radiation treatment sites
Post-Gynecologic Cancer Treatment Causes of Pelvic Pain
- Surgical effects, such as scar tissue formation, altered anatomy, or nerve damage from procedures like hysterectomy, oophorectomy, or lymph node removal
- Radiation therapy, involving pelvic floor tissue damage, fibrosis, or inflammation due to radiation exposure
- Hormonal changes, decreased estrogen levels causing vaginal tissue compromise or genitourinary syndrome of menopause (GSM)
- Chemotherapy side effects, which impact tissue health and muscle function
- Pelvic muscle overactivity, involving muscle tension or spasms triggered by pain or trauma from treatment
- Nerve damage, the injury to pelvic nerves during surgery or radiation
- Psychological factors, including anxiety, depression, or PTSD related to cancer diagnosis and treatment
- Lymphedema, swelling and discomfort in the pelvic area due to lymphatic damage
- Adhesions, internal scar tissue causing restricted movement and pain
Post-Gynecologic Cancer Treatment Pain Treatment
- Pelvic floor Physical or Occupational Therapy is warranted after cancer treatment
- Therapies may include manual therapy, dilator therapy, neuromuscular re-education, homes exercise program development, patient education
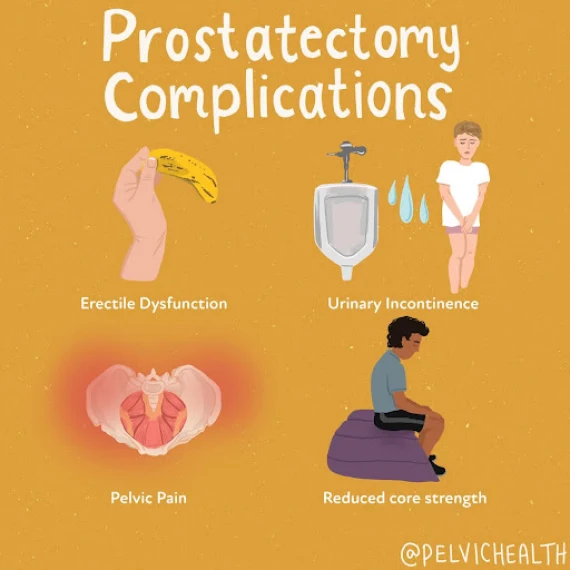
Post-Prostatectomy Symptoms
- Urinary incontinence
- Urinary urgency, frequency, nocturia
- Erectile Dysfunction
- Pelvic and Perineal Pain
- Diastasis Recti
Causes of Post-Prostatectomy
Surgical procedures such as:
- Simple prostatectomy
- Radical prostatectomy
- Robotic-assisted prostatectomy
- Laprascopic prostatectomy
- Single-port radical prostatectomy
Treatments for Post-Prostatectomy
Research shows that men who undergo pelvic floor prehab (physical or occupational therapy prior to surgery) have a reduced risk of urinary incontinence and erectile dysfunction. Studies also show that men who have post-prostatectomy rehab within one year of surgery have significantly less urinary leakage and sexual dysfunction. Treatment includes:
- Manual therapy
- Neuromuscular re-education
- Home Exercise Program Development
- Patient Education
What To Expect During Your Appointment
When you arrive for your first appointment at PHRC, our primary goal is to understand your pelvic health concerns. During this initial consultation, your therapist will ask about your medical history, including any previous pelvic surgeries, childbirth experiences, or conditions that might contribute to symptoms such as urinary issues, bowel dysfunction, sexual pain, musculoskeletal pelvic pain, or pudendal and pelvic neuralgias. This thorough discussion will help us determine the best approach for your care. We are also looking to understand what providers, if any, are currently involved in your care and listening for issues that might need additional medical management.
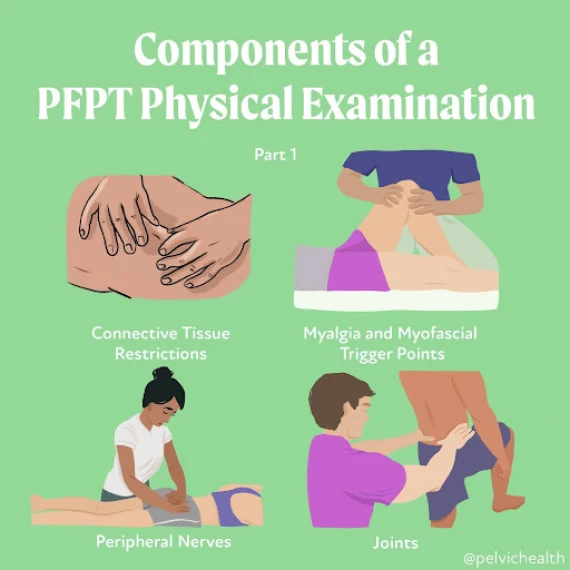
A physical examination will follow, where your pelvic floor physical or occupational therapist will evaluate the muscles, tissues, and nerves in the trunk, pelvic girdle, and pelvic floor muscles. This examination may include checking for muscle and connective tissue pain, tightness, weakness, or imbalances that could be affecting your pelvic floor function. We also assess how well your muscles coordinate during breathing and movement, which is helpful for managing functions like urination, bowel movements, and sexual activity.
Once the physical examination is complete, your pelvic floor physical or occupational therapist will provide you with an assessment. This assessment links your history to your current symptoms and findings from the physical examination. It is important for us to develop a working theory as to how your pain and dysfunction began and which physical impairments are contributing. Often multiple factors are involved, both in terms of the musculoskeletal system and possibly other symptoms as well.
Part of the assessment involves setting both short-term and long-term goals. Short-term goals focus on specific issues, like reducing pelvic floor muscle pain to ease discomfort during sex or improving pelvic floor muscle control to address urinary symptoms. Long-term goals are more focused on overall function, such as helping the patient have enjoyable, pain-free intercourse or reducing the need to urinate more than eight times a day without pain or hesitation.
You and your therapist will work together to create a treatment plan, deciding how often and for how long you’ll have sessions. This plan will guide you toward relieving your symptoms and reaching both your short-term and long-term goals.
The in-person clinical treatment plan is usually weekly and includes manual therapy, neuromuscular re-education, patient education, therapeutic exercise, and home exercise program development. Short-term goals can usually be achieved in 12 weeks. Treatment plans are dynamic and will evolve over time as impairments reduce and improvement is made. As therapists, we are afforded more time with our patients than our medical colleagues are, therefore, we will also communicate with other providers to ensure medical management is also organized and coordinated with the plan of care at PHRC.
Find Relief From PHRC
At PHRC, our goal is to provide compassionate and comprehensive care to help you manage and overcome pain from pelvic floor dysfunction. By understanding the underlying causes and providing targeted treatments, our goal is to improve your quality of life and restore your health.
We also recognize the challenges some people might face in accessing in-person care, which is why we offer virtual sessions through telehealth after your initial consultation. These sessions allow for continuity of care and accessibility for those unable to travel to one of our clinics.
By Emily Tran
SCHEDULE APPOINTMENT
Hello 2025, farewell 2024! It’s been another year full of changes for Pelvic Health and Rehabilitation Center. With the start of the new year, we would like to acknowledge all of the changes that have occurred both virtually and in person.
Last year…..
Social Media Expansion and Engagement
With our ever increasing audience, we wanted to share some wins through social media! Our Youtube channel surpassed the 17k subscribers mark, our Instagram page flew over 53k followers, and recently our Tik Tok hit almost 12k followers, Twitter soared over 7k followers, LinkedIn hit 1.7k followers and our Facebook jumped in followers from 14k to 17k followers! We thank you for your support and for helping us spread the word about pelvic floor physical and occupational therapy and pelvic health!
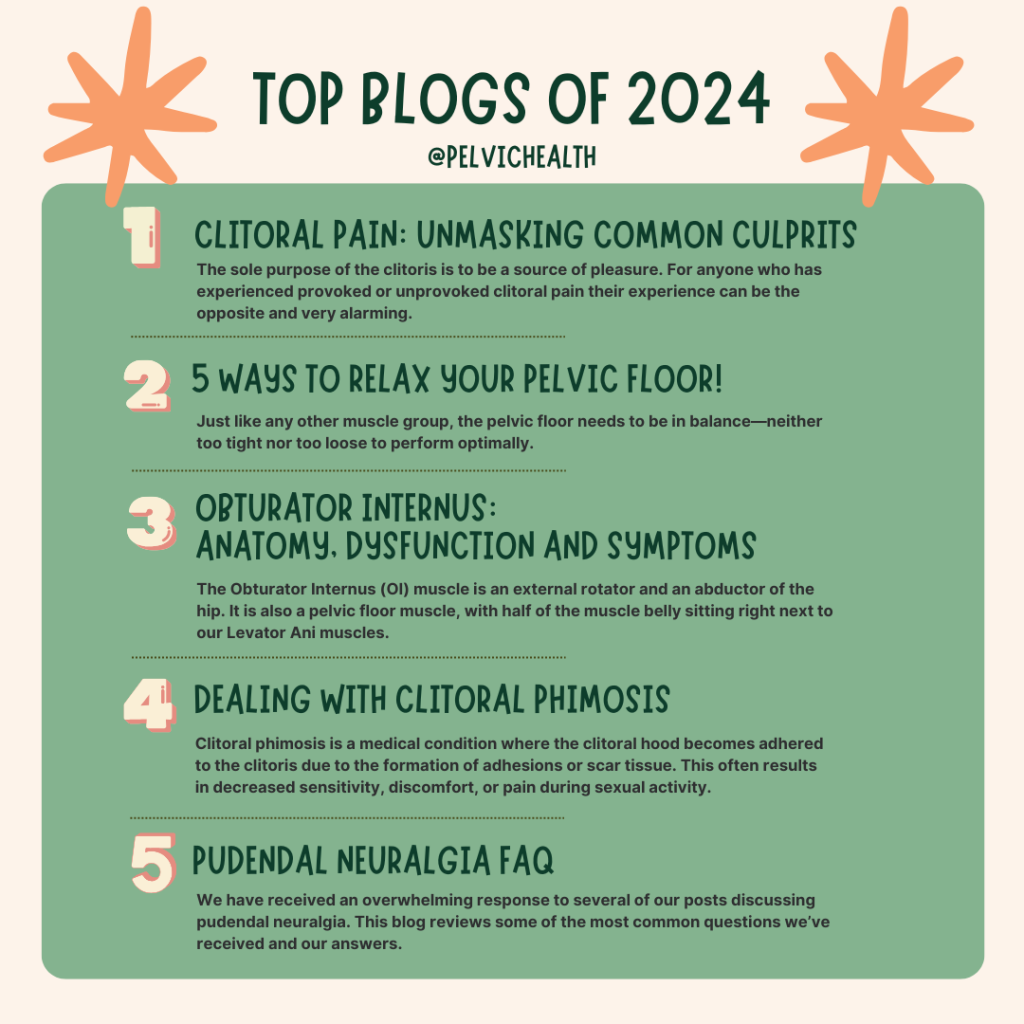
Our Top Blogs
Clitoral Pain: Unmasking Common Culprits- The sole purpose of the clitoris is to be a source of pleasure. For anyone who has experienced provoked or unprovoked clitoral pain their experience can be the opposite and very alarming.
5 Ways to Relax Your Pelvic Floor- Just like any other muscle group, the pelvic floor needs to be in balance—neither too tight nor too loose to perform optimally.
Obturator Internus: Anatomy, Dysfunction and Symptoms- The Obturator Internus (OI) muscle is an external rotator and an abductor of the hip. It is also a pelvic floor muscle, with half of the muscle belly sitting right next to our Levator Ani muscles.
Dealing with Clitoral Phimosis- Clitoral phimosis is a medical condition where the clitoral hood becomes adhered to the clitoris due to the formation of adhesions or scar tissue. This often results in decreased sensitivity, discomfort, or pain during sexual activity.
Pudendal Neuralgia FAQ- We have received an overwhelming response to several of our posts discussing pudendal neuralgia. This blog reviews some of the most common questions we’ve received and our answers.
We were featured as guests on quite a few platforms!
- It is always an honor to work alongside Tight Lipped Organization! Our cofounder, Stephanie Prendergast, was a part of a panel being featured in the upcoming Vagina Girl Documentary. It was an empowering evening all about Vaginal/Vulvar Pain. Thank you Tight Lipped Org and Vagina Girl documentary for hosting us all! Stay tuned for the upcoming documentary as it shines a light on vaginal + vulvar pain to help raise awareness and facilitate (much needed) change across the medical field!
View this post on Instagram
- Cofounder, Stephanie Prendergast was interviewed on HEM SupportWear’s podcast. In her interview, the host shares her unexpected experience of being diagnosed with prolapse early in her postpartum journey, despite feeling educated and empowered during pregnancy.
- Jandra Mueller, DPT, MS (Encinitas) was interviewed on the Al Jazeera English Podcasts to discuss Endometriosis- Join @miss_samjohnson and @pelvichealthsd as they discuss the crucial symptoms you should never ignore on #NowYouKnow.
- Cofounder, Stephanie Prendergast was part of the online, multi-disciplinary Vulvodynia Symposium hosted by Pelvicon.
- PHRC hosted an exclusive fundraiser/educational event during Pelvic Pain Awareness Month (May)! Our talk included Tight Lipped’s Patient Advocacy work by Keena Batti, Sneak peek from the film Vestibule, Presentation of PHRC’s new e-book from Stephanie and Jandra, A Q&A with our EXPERT medical panel Drs. Rubin, Krapf and Cigna plus more!
- Stephanie Prendergast and Jandra Mueller were a part of the Genito-Pelvic Pain 2024/5 course!
- Jandra Mueller and Britt Gosse-Jesus hosted Endometriosis 101: Moving Towards Better Care- This course is designed to empower you with knowledge and tools to navigate the complexities of endometriosis.
- Our cofounder, Stephanie Prendergast was interviewed by Sameena Rahman, to explore the insidious nature of pudendal neuralgia, its symptoms, and the challenges it presents in diagnosis and treatment.
- The second annual Menoposium LIVE in Chicago was a hit, with cofounder Stephanie Prendergast.
- Jandra Mueller was interviewed on the Chronic Illness Therapist Podcast. They discussed all things pelvic pain, endometriosis, and pelvic floor physical and occupational therapy.
We published TWO eBooks
Vulvodynia, Vestibulodynia, and Vaginismus
Chances are you or someone you know is dealing with vulvar pain and urogenital concerns. This book serves as a comprehensive guide to navigating these issues. Urogenital pain is prevalent in people with vulvas, and there ARE solutions! Despite extensive research and endorsement from top medical experts and leadership societies, not everyone is aware of the benefits of the strategic combo of medical management & pelvic floor PT.
We’ve developed this e-book to provide reliable information, practical tips, and solutions for those struggling with urogenital pain!By combining physical and occupational therapy and medical treatment, you can overcome these challenges and regain control over your pelvic health. Our goal is to lead you towards a reasonable path to feel yourself again.
We are here to help people find their individual solutions and to provide hope that full recoveries are possible and this book will tell you how!
Purchase it here: Vulvodynia, Vaginismus & Vestibulodynia
Careers at Pelvic Health and Rehabilitation Center
Have you seen our latest e-book? This free e-book gives an in-depth review about Careers At PHRC! We are always on the search for occupational and physical and occupational therapistss to join our team!
Why should you consider working with us?
- Paid Training Mentor Program
- Paid Professional Development
- Paid Ongoing Mentorship
- Plus More Benefits!
Interested in reading more about becoming part of the team? Submit your resume via our website today!
Our Pasadena Office Welcomed Dr. Winter
Our colleague Dr. Rachel Rubin expanded her practice to include Dr. Ashley G Winter!
The news continues as we welcomed Dr. Winter, urologist and sexual medicine specialist to our Pasadena office! She see patients in person in the LA area and Telemedicine for CA residents. She will also be seeing patients from out of state, but they must come into her Pasadena/LA office for in-person appointments. She will be seeing patients with conditions such as:
- Perimenopause/Menopause
- Orgasm Disorders
- Low Libido
- Hormone Therapy
- Testosterone
- Pelvic Pain
- Male Sexual Dysfunction
- Female Sexual Dysfunction
Interested? Check out how to start the new patient process with Dr. Winter!
We celebrated the release of the M Factor documentary!
What is the M Factor? The first documentary film that addresses the marginalized or ignored health crisis faced by millions of women as they go through menopause.
This documentary is currently airing on PBS! We encourage everyone to go and give it a watch.
We want to give a HUGE thank you to Tamsen Fadal, Denise Pines, and Dr. Kelly Casperson for their continued work! Please help us share the news of this amazing documentary: The M Factor: Shredding the Silence on Menopause.
We supported (and continue to support) the Unboxing Menopause Campaign
Why are we in support of this campaign? Despite overwhelming support from scientific studies, this outdated boxed warning continues to restrict access to this essential treatment. This isn’t just about removing a warning label it’s about saving lives and improving women’s health.
Women deserve accurate, evidence-based information that reflects the true safety of local vaginal estrogen!
What can you do? Join us in urging the FDA to remove this outdated and misleading warning by supporting the Unboxing Menopause campaign. Your voice can make a difference. Let’s fight for the care all women deserve. Want access to the facts, resources and templates to send a letter to the FDA? Whether you are a physician or patient, we got you! You can get all the information and more via their website.
Special thanks to Dr. Kelly Casperson, Dr. Rachel Rubin and This is the Swell for helping us announce this campaign!
We continue to support Tight Lipped Org
We’re proud to support Tight Lipped, a patient advocacy group bringing crucial sexual medicine training to OBGYN residents, and Riley Hooper’s documentary “Vestibule,” sharing her journey with Vestibulodynia. All patients with vulvovaginal and pelvic pain deserve access to effective and compassionate care. Yet, the vast majority of us can’t even get a diagnosis–and that’s why we’re fighting for change. Changing medical practice, standards, and training takes time and we’re in it for the long-haul.
We couldn’t take this on without incredible grassroots support from our community. We’re aiming to raise $23,000 to deepen our work.
PHRC continues its partnerships in helping The Jackson Clinics Foundation
The past two years a group of us, under the umbrella of The Jackson Clinic Foundation, have been developing a two year advanced degree program in Pelvic Health for physical and occupational therapistss in Kenya, Africa! We have been mining our beautiful pelvic health community for content contributors, teachers, and volunteers. It’s been a beautiful, intense, overwhelming experience…and it’s HAPPENING!
Over the next 2 years students will experience a robust online curriculum and 6 in person segments with expert teachers from the US. BUT the GOAL is to have this program independently run by Kenyans. For this first run of the program, we will be teaching a whole new batch of students. AND also training women who have been through pelvic health education to be the next generation of TEACHERS. These women will be the volunteer Teacher Assistants for the 6 in person sessions.
We would love to give them a financial gift for their support of the program, the students and pelvic health in Kenya. They will be taking unpaid time off of work which of course is a barrier. This gofundme will raise money to support our volunteer TAs and also go to purchase a few teaching supplies (books, models) that we would like to provide to the students to enhance their learning.
Please consider donating to the future of pelvic health in Kenya. Whether you can donate, share this post or engage with us, we are appreciative!
Please visit https://gofund.me/30cdd665 for more info!
Here’s to the rest of 2025 and all things pelvic health
Thank you for joining us for another year. We’re wishing you all a healthier, stronger new year!
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
By Cambria Oetken, DPT, PHRC Westlake Village and Stephanie Prendergast, MPT, PHRC Pasadena
HOT off the Press:
Menopause is finally getting the attention it deserves in recent years with an exponential amount of attention in 2024. This year, Let’s Talk Menopause has considered their advocacy work, heading to Capital Hill and hosting in-person events for women. Tamsen Fadel and Denise Pines produced the documentary The M Factor which aired on PBS this October (stream it for free NOW!) and is being screened around the country.
While menopause was previously characterized as hot flashes and vaginal dryness, we now know so much more. This week we share new research about another symptom caused by hormonal decline: muscle and joint pain. While this sounds frustrating, understanding the role hormones play in our musculoskeletal health can be viewed as a therapeutic opportunity to help people live their best lives.
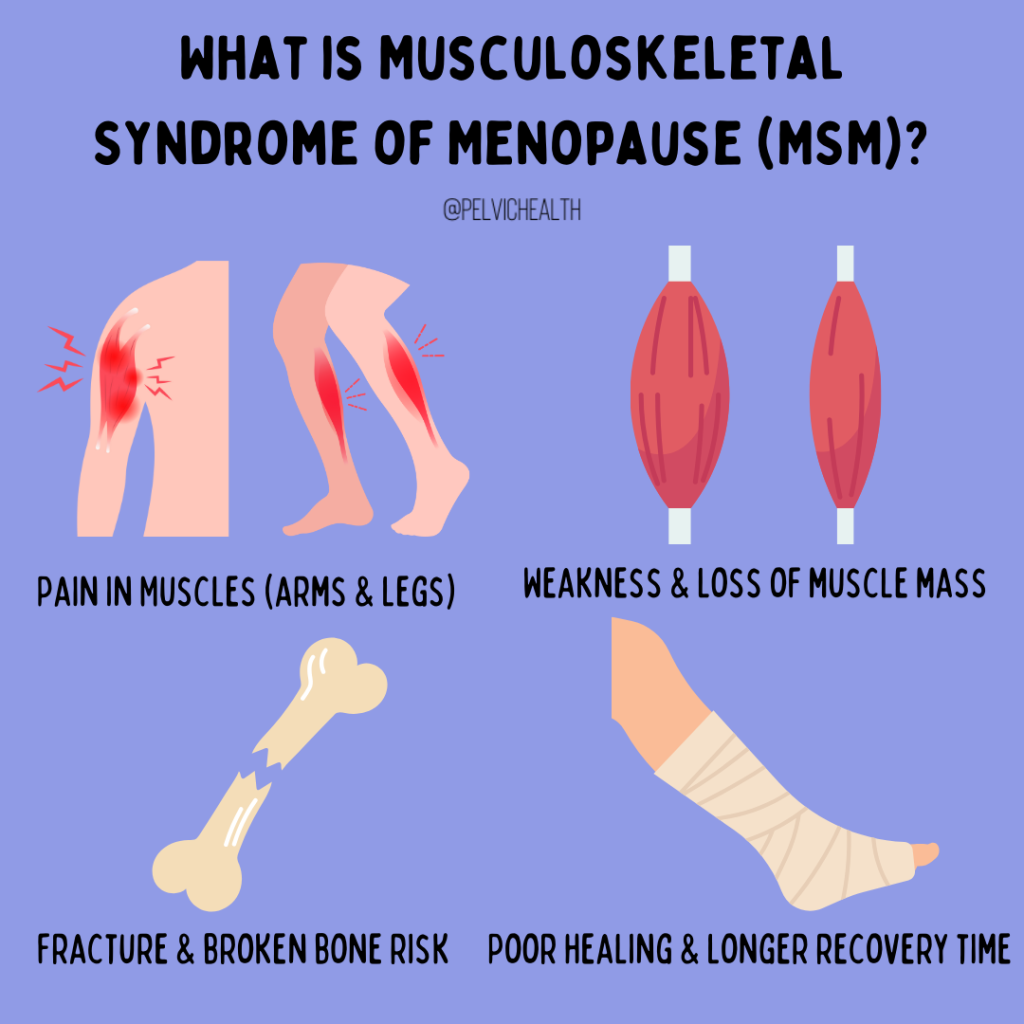
A recent article has introduced a new term called the Musculoskeletal Syndrome of Menopause (MSM) discussing the implications of menopause on our muscular system due to the precipitous drop in estrogen during this transition. Approximately 2 million women in the US will enter menopause annually, 70% of those women will experience the musculoskeletal syndrome of menopause, and 25% will experience severe symptoms. Menopause is considered a transition that occurs between the ages of 45 and 55 and has 35 known symptoms being associated with it. Menopause is typically determined as occurring 12 months after a woman’s last menstrual cycle, and can also be confirmed with additional lab testing. With the relevance of how many women experience menopause yearly it is crucial to be aware of the symptoms associated with it and how we can best treat these women to optimize their wellbeing.
Common symptoms of menopause include hot flashes, brain fog, sleep disturbances, anxiety, menstrual changes, night sweats, vaginal dryness and more. A previous syndrome that has been recognized is the genitourinary syndrome of menopause (GSM) which has been presented in previous articles discussing the genitourinary symptoms that can occur.
The article discussed her states that the the musculoskeletal syndrome of menopause (MSM) includes, but is not limited to, musculoskeletal pain, arthralgia (joint pain), loss of lean muscle mass, loss of bone density with increased risk of resultant fracture, increased tendon and ligament injury, adhesive capsulitis (“frozen shoulder”), and cartilage matrix fragility with the progression of osteoarthritis. These musculoskeletal issues can be attributed to the decline in estradiol which is a fundamental form of estrogen needed for bone, tendon, muscle, cartilage, ligament and adipose.
The decline in estrogen in perimenopause and menopause lead to 5 primary changes that will be summarized below.
1. Increased Inflammation
More than half of menopausal women report arthralgia or joint pain symptoms. Estrogen is a known inflammatory regulator that is part of our immune system and thus with this significant drop in estrogen, inflammation can become more difficult to combat. The article discusses menopausal hormone therapy (MHT) as an important treatment option to help regulate these symptoms of inflammation.
2. Sarcopenia
Sarcopenia is the age related loss of lean muscle mass with an increased amount of intramuscular adipose tissue (fat!). There are some nutritional interventions that have been recommended in the literature including protein, vitamin D and creatine that are shown to be effective in combination with resistance training. The decrease in estrogen is also an imperative factor associated with this condition that also decreases insulin sensitivity. With decreased estrogen capacity it can become difficult to regulate glucose especially in the skeletal muscle. The suggested method to assist in this long term is menopausal hormone treatment and resistance training.
3. Satellite Cell Proliferation
Satellite cells, also known as stem cells are crucial cells found in muscle fibers and are activated during an injury to repair muscle tissue. Estradiol is the hormone responsible for stimulating these cells to begin the repair mechanism. However, when we lose this stimulation that estrogen drives, muscle strength and recovery become impaired, making recovery from injury slower and less efficient.
4. Bone Density
You have likely heard of osteoporosis which affects 200 million menopausal women and is an underdiagnosed condition that is preventable and treatable! 30-50% of women will suffer a fracture in their lifetime which puts them at significant risk for long term chronic pain, disability and even death. Prevention of this is key and includes optimal nutrition, resistance training, and yep, you guessed it hormone treatment should it be appropriate. Hormone treatment has been shown to prevent and treat osteoporotic fractures.
5. Cartilage Damage and Osteoarthritis
There is conflicting evidence in the relationship between estrogen decrease and the frequency of hip, knee and finger osteoarthritis as well as the severity of hip osteoarthritis. However, estrogen has shown to have protective properties in the intervertebral discs of our spine which could suggest its role in helping to prevent osteoarthritis and further cartilage damage. Though more research is needed, there is pertinent evidence that estrogen replacement therapy can partake in reducing these changes in the connective tissue matrix.
The article considers the conservative approaches that are available should menopausal hormone replacement not be an option for certain patients. The study discusses the benefits of Vitamin D2 on bone turnover, magnesium to help optimize Vitamin D and K2 to potentially decrease the progression of and treat osteoporosis. Creatine and protein intake are also heavily studied nutritional options in improving bone mineral density and muscle power output.
Along with these nutritional supplements is resistance training, which is an accessible, non medical option that is a crucial component in managing musculoskeletal care, preventing age related injuries and decreasing mortality rates. Talking with your physical and occupational therapists in creating a safe, effective and progressive weight training plan can be utmost beneficial.
Pelvic Floor PT and MSM
Since resistance training has continued to be a recommended staple in the prevention of these major primary factors associated with MSM, your physical and occupational therapists can be a guide in navigating this long term. During a physical and occupational therapy examination your PT can evaluate your strength, ROM, pelvic floor strength, and functional goals you may have in order to develop a customized exercise plan to meet your needs. PTs are trained to identify imbalances or weaknesses that could predispose you to injury, such as poor posture or dysfunctional movement patterns. Resistance training requires progressive overload to build strength, which means gradually increasing the resistance or intensity of the exercises. However, it’s essential to do this at the right pace to avoid overtraining or re-injuring yourself, especially if you’re coming back from an injury.
Your physical and occupational therapists can help you determine when to increase the intensity of your exercises based on your progress. They will monitor your response to resistance training, adjusting the program to ensure you’re constantly improving without putting yourself at risk. Whether it’s increasing weights, reps, or sets, or incorporating more complex movements, your PT can help ensure that you’re progressing in a way that’s both safe and effective.
In conclusion
This article suggests the importance for patients and their medical care team to be aware of the changes that occur with menopause and recognize prevention approaches in order to optimize this population’s well being. The combination of informed and shared medical management and physical and occupational therapy can help people feel more comfortable in their bodies. We are now spending ⅓ of our lives in menopause and there is no need to suffer.
Resources
Wright, V. J., Schwartzman, J. D., Itinoche, R., & Wittstein, J. (2024). The musculoskeletal syndrome of menopause. Climacteric, 27(5), 466–472. https://doi.org/10.1080/13697137.2024.2380363
The M Factor which aired on PBS this October
Find a certified menopause healthcare practitioner in your area
Further reading about menopause
______________________________________________________________________________________________________________________________________
Check out our recently published e-book titled “Vulvodynia, Vestibulodynia, and Vaginismus,” designed to empower and inform individuals on their journey towards healing and understanding.
Did you know we opened our 11th location in Columbus, OH? Now scheduling new patients- call (510) 922-9836 to book!
Are you unable to come see us in person in the Bay Area, Southern California or New England? We offer virtual physical and occupational therapy appointments too!
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. For more information and to schedule, please visit our digital healthcare page.
Do you enjoy or blog and want more content from PHRC? Please head over to social media!
Facebook, YouTube Channel, Twitter, Instagram, Tik Tok
tags: menopause symptoms, menopause transition, muscle pain, hormone therapy, hormone replacement therapy, muscle aches, women’s health, menopausal transition