Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Menopause is more than just hot flushes, night sweats and mood changes! Even though 50% of the population goes through menopause the majority of people and healthcare providers are under-informed about menopause and safe and effective treatments. Too many people are suffering unnecessarily. Perimenopause, the precursor to menopause begins in the 40’s for most people and most women will be in menopause by their early 50’s. Beyond the systemic symptoms of menopause people will start to experience more subtle genitourinary symptoms that will continue to worsen over time if untreated. Painful sex, urinary urgency, frequency, leaking and burning, recurrent vaginal and urinary tract infections and vaginal dryness are symptoms of the Genitourinary Syndrome of Menopause (GSM). The symptoms of GSM are also symptoms of pelvic floor dysfunction, which almost 50% of women suffer by the time they are in their 50s.
Systemic menopause symptoms are often treated with systemic hormonal therapy. This may not be sufficient for people developing GSM symptoms. The North American Menopause Society recommends vaginal estrogen for women in menopause to help counter GSM symptoms.
Differential Diagnosis:
GSM or Pelvic Floor Dysfunction
Symptoms of pelvic floor dysfunction and GSM include:
- Urinary urgency, frequency, burning, nocturia
- Feelings of bladder or pelvic pressure
- Painful sex
- Diminished or absent orgasm
- Difficulty evacuating stool
- Vulvovaginal pain and burning
- Pain with sitting

An informed healthcare provider – whether a pelvic floor physical and occupational therapists or medical doctor – can do a vulvovaginal visual examination, a q-tip test to establish pain areas, and a digital manual examination to identify pelvic floor dysfunction, hormonal deficiencies, and pelvic organ prolapse. All women will experience GSM if enough time passes without appropriate medical management. The majority of people do not realize that menopausal women can benefit from a pelvic floor physical and occupational therapy examination to address the musculoskeletal factors that are also making them uncomfortable. The combination of pelvic floor physical and occupational therapy and medical management is key to help restore pleasurable sex and eliminate urinary and bowel concerns!
FACTS
From: https://www.letstalkmenopause.org/further-reading
- 6000 women enter menopause everyday
- 50 million women are currently menopausal in the US
- 84% of women struggle with genital, sexual and urinary discomfort that will not resolve on its own, and less than 25% seek help
- 80% of OBGYN residents admit to being ill-prepared to discuss menopause
- GSM is clinically detected in 90% of postmenopausal women, only ⅓ report symptoms when surveyed.
- Barriers to treatment: women often have to initiate the conversation, believe that the symptoms are just part of aging, women fail to link their symptoms with menopause.
- Only 13% of providers asked their patients about menopause symptoms.
- Even after diagnosis, the majority of women with GSM go untreated despite studies demonstrating a negative impact on quality of life. Hesitation to prescribe treatment by providers as well as patient-perceived concerns over safety profiles limit the use of topical vaginal therapies.


Hormone insufficiency can result in interlabial and vaginal itching. Other dermatologic issues such as Lichen Sclerosus and cutaneous yeast infections are just two of the many factors to also be considered.
Unfortunately people are vulnerable to recurrent vaginal and urinary tract infections in menopause due to:
- pH and tissue changes
- incomplete bladder emptying
- pelvic organ prolapse compromising urinary function
Recurrent infections are a leading cause of pelvic floor dysfunction! They must be stopped or the noxious visceral-somatic input can cause further pain and dysfunction after the infection is cleared. Furthermore, if the infections are left untreated without hormone therapy infections continue to occur and the consequences can be severe. Women can develop unprovoked pain, sex may be impossible, and undetected UTIs can lead to kidney problems and more sinister issues.
We encourage people to work with a menopause expert to monitor, prevent, and treat these issues as they are serious and treatable! We need to normalize the conversation about what happens during GSM, it is nothing to be embarrassed about and with the right care vulva owners can live their best lives! Pelvic floor physical and occupational therapy and medical management go hand in hand.
Treatment:
How We Can Help You

If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.

Treatment:
How We Can Help You
If you are having issues with your sexual function, it is in your best interest to get evaluated by a therapist for pelvic floor therapy, so they can establish what part, if any, of your pelvic floor may be contributing to the symptoms you are experiencing. During the course of the examination, the physical and occupational therapists will talk to you about your medical history and symptoms, including what you have been previously diagnosed with, the treatments or therapies you have had, and how effective or ineffective these therapies have been for you. It is significant to mention that we fully comprehend what you’ve been dealing with and that the majority of individuals are angry by the time they make it to see us. The physical and occupational therapists will conduct an evaluation of the patient’s nerves, muscles, joints, tissues, and movement patterns while doing the physical examination. After the examination is finished, your therapist will go over the results of the assessment with you. The physical and occupational therapists will conduct an evaluation to determine the cause of your symptoms and will establish both short-term and long-term therapy goals based on the results of the evaluation. Physical therapy treatments are typically administered between once and twice each week for a period of around 12 weeks. Your physical and occupational therapists will assist you in coordinating your recovery with all the other experts on your treatment team. They will provide you with an exercise regimen to complete at home and the sessions you attend in person. We are here to assist you in getting better and living the best life possible.
For more information about IC/PBS please check out our IC/PBS Resource List.
As many of us reading this blog can attest, pelvic pain can be an issue that leaves us feeling not only physically uncomfortable, but emotionally/mentally drained and isolated. Often, by the time many people get seen by a physical and occupational therapists, they have been mismanaged by other providers, leading to increased frustration among other things. Men, in particular, seem to be the population most overlooked or poorly managed by the current healthcare system when dealing with pelvic pain. The most current research on the prevalence of pelvic pain among males reports that 15% of men have dealt with or are currently dealing with pelvic pain at some point in their lives.1 And that is just based on a sample size of men that were actually willing to report whether or not this is something that has been an issue;I tend to think that this number might even be higher. Here is a great blog post on male pelvic pain that Stephanie wrote earlier this year.
Throughout this blog, we have tried to touch on so many of the issues that come up when dealing with pelvic pain, but have never specifically talked about what could be happening on a musculoskeletal level when erections become painful. This is such a common issue that I see men dealing with, so I wanted to spend some time delving into what can be happening to our sexual function when there are myofascial impairments in the pelvic floor musculature.
First, let’s do an anatomy review. My colleague Rachel Gelman, DPT wrote a great post last year detailing the male pelvic anatomy. She explains that “All of the internal muscles that make up the pelvic floor are the same for men and women. The muscles sit in the pelvis like a muscular bowl, providing support to the organs of the pelvis and assisting in bowel, bladder, and sexual function…In men, the pelvic floor supports the prostate as well as the bladder and the colon.”
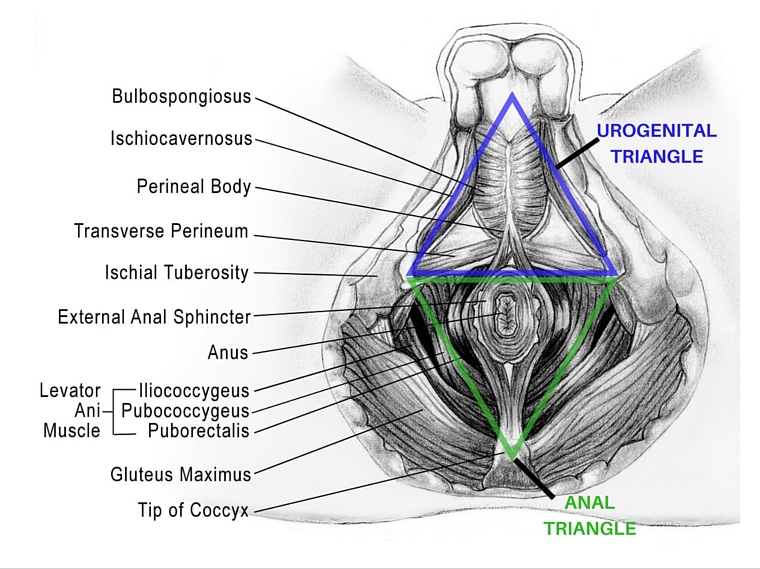
Taking a closer look at the image below, you will see that the artist has included two different triangles over the pelvic muscle groups. The top outline surrounds the urogenital triangle and the bottom outline identifies the anal triangle. The urogenital triangle muscles (aka urogenital diaphragm) are the most superficial muscles of the pelvic floor, comprised of the bulbospongiosus, ischiocavernosus, transverse perineum and external anal sphincter. These are the muscles that I will be writing about in this blog because they are the most involved muscles during arousal and orgasm.
The penis is an organ that serves both urinary and sexual functions. It is made up of highly vascularized soft tissue that can become erect when there is an increased blood volume in the area . The bulbospongiosus (see on image above) attaches from the transverse perineal muscle to the lower ⅓ of the penis. During arousal blood rushes into the penis and is held in place by a sustained contraction of both the bulbospongiosus and the ischiocavernosus. Orgasm and ejaculation occur when these 2 muscles begin to maximally contract and relax repeatedly.
That is the how the muscle system physiology should work during a typical erection and orgasm/ejaculation. However, what happens if something goes awry? In many cases of pelvic pain and dysfunction, the pelvic floor muscles have been in a long term, shortened position. When they are contracted, tight, they often have trigger points, and they are often tender or painful to the touch. So it can make sense that if the muscles are already in a contracted state, it can be painful when there becomes an increased demand on these structures. We can apply this concept to a similar situation elsewhere on the body;think about if you have ever had a tight calf muscle, it doesn’t take much to put that thing into a full blown charlie horse (anyone ever wake up in the middle of the night with these?). But it is the same idea;calf muscle is tight, we tend to sleep with our feet/ankles in a plantar flexed or pointed position, the muscle gets pushed past its breaking point and we end up with a major cramp.
Here is how PT can help:
Painful erections can be caused by hypertonic pelvic floor muscles and potential trigger points. Think about it, if we need those superficial pelvic floor muscles to contract and maintain a sustained contraction for any length of time, that’s a big deal for those muscles. It’s like a major workout, and if they are already in a tightened state, then getting them to further tighten is going to be a problem. People with tight pelvic floor muscles may often notice difficulty achieving and maintaining an erection or diminished quality of erection. This change often precedes the onset of pelvic pain.
If you are experiencing this issue, consult with your physician and a pelvic floor physical and occupational therapists to address potential issues. Painful erections that are occurring due to factors mentioned in this blog are highly treatable with PT intervention. If you need some help finding a pelvic floor specialist in your area, check out some previous posts on this matter here and here.
Because the pelvic floor muscles are so often involved with this issue, it is important to schedule with a pelvic floor physical and occupational therapists sooner rather than later. Here are two previous blog posts on what to expect from a good pelvic floor physical and occupational therapy session.
______________________________________________________________________________________________________________________________________
Are you unable to come see us in person? We offer virtual appointments!
Due to COVID-19, we understand people may prefer to utilize our services from their homes. We also understand that many people do not have access to pelvic floor physical and occupational therapy and we are here to help! The Pelvic Health and Rehabilitation Center is a multi-city company of highly trained and specialized pelvic floor physical and occupational therapistss committed to helping people optimize their pelvic health and eliminate pelvic pain and dysfunction. We are here for you and ready to help, whether it is in-person or online.
Virtual sessions are available with PHRC pelvic floor physical and occupational therapistss via our video platform, Zoom, or via phone. The cost for this service is $75.00 per 30 minutes. For more information and to schedule, please visit our digital healthcare page.
In addition to virtual consultation with our physical and occupational therapistss, we also offer integrative health services with Jandra Mueller, DPT, MS. Jandra is a pelvic floor physical and occupational therapists who also has her Master’s degree in Integrative Health and Nutrition. She offers services such as hormone testing via the DUTCH test, comprehensive stool testing for gastrointestinal health concerns, and integrative health coaching and meal planning. For more information about her services and to schedule, please visit our Integrative Health website page.
References:
Systematic Review of Acupuncture for Chronic Prostatitis/Chronic Pelvic Pain Syndrome. Qin Z, Wu J, Zhou J, Liu Z. Medicine (Baltimore). 2016 Mar;95(11):e3095.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Joshua Gonzalez, MD
After reading my last post, Jagged Little Pill, many of you who have had similar suspected OCP-related problems may be thinking there’s no hope. Trust me, you are not doomed if you’ve ever taken an oral birth control and you have symptoms of vulvodynia. My goal this week is to reassure you that you’re not alone and that there are many resources and solutions available to you.
Find the right provider.
Once you recognize that you may be suffering from vulvodynia/vestibulodynia, interstitial cystitis, recurrent infections, or any other symptoms or conditions you think may be related to your hormonal birth control, say something. Bring it up with your provider. Voicing your concerns is the first step. As I alluded to last week though, you speaking up may sometimes fall on deaf ears. But that doesn’t mean you should stay quiet.
Much of the attention regarding the adverse effects of OCPs focuses on nausea, headache, breakthrough menses, breast tenderness, or blood clots. Many prescribers of OCPs don’t bother to ask if you’re having pain with intercourse. As long as you’re not getting pregnant, they don’t really care. Some feel uncomfortable asking; others simply don’t want to hear about it. Still others may not recognize the aforementioned symptoms as being at all related to oral contraceptive pills. But that doesn’t mean it isn’t happening to you. If you don’t feel heard by your physician or health care provider, find someone that will listen.
Finding that special someone may mean having to think outside of the box. There are a myriad of providers out there that see patients just like you all the time: internists, gynecologists, urologists, pelvic floor physical and occupational therapistss, psychologists and psychiatrists, and endocrinologists. Seek these providers out. Heck, seek out more than one. Sometimes it takes more than one provider to provide solutions; to resolve these issues, it often takes a village.
Get educated.
There’s plenty of resources online. Read blogs, search for forums with patients reporting similar symptoms, get informed. You can’t believe everything you read, but there are plenty of national and international societies out there that offer reliable information.
One easy place to start is this very blog. Others have previously written on the topic of oral contraceptives and their potential harm. Drs. Goldstein, Krapf, and Belkin wrote a great piece outlining the differences between different OCPs and discussing some of the potential factors that may predispose certain women to harm after using these medications. Check it out here.
The International Society for the Study of Women’s Sexual Health (ISSWSH) website is another great place to start (www.isswsh.org). ISSWSH is a multidisciplinary, academic, and scientific organization focused solely on the study of female sexual health. They formed to address needs not being met by other medical societies. On their website, you can search for providers well versed in the management of issues affecting female sexual health. There are consensus statements on specific conditions like vulvodynia, news about the latest scientific happenings in female sexual health, and links to important research articles. But remember that this is a medical society, so some of the information may be a little complicated for the average reader.
Sex Health Matters (www.sexhealthmatters.org) is a fantastic website maintained by the Sexual Medicine Society of North America (SMSNA). Established in 1994, SMSNA is a non-profit organization of physicians, researchers, and other allied health professionals. They focus on both male and female sexual health, but there is plenty of good information on conditions affecting the latter. Learn about hypoactive sexual desire disorder (HSDD) or how acupuncture may help women with vulvodynia. Sign up for their regularly distributed e-newsletter to learn more about issues affecting women’s sexual health. The information here tends to be a little more reader friendly and easier to understand.
If you’re having vulvar or vestibular pain, check out the National Vulvodynia Association’s website (www.nva.org). The NVA is another non-profit organization formed in 1994 that focuses specifically on vulvodynia. Many of their services are restricted to members only but fortunately one of the most valuable parts of the site is absolutely free. Check out the Patient Stories section to hear the experiences of women with vulvodynia, maybe women just like you. You can even share your own story. You can learn about the latest research going on in the study of vulvodynia and even volunteer to be part of future studies. The site also offers useful Self-Help Tips that anyone suffering from vulvodynia will appreciate.
The International Pelvic Pain Society (IPPS) website is also another helpful resource. They offer a wealth of handouts regarding conditions like interstitial cystitis, pelvic floor dysfunction, endometriosis, pudendal neuropathy, irritable bowel syndrome (IBS), and vulvodynia. All of them are informative and meant for you to easily understand. You can search for medical professionals in your area that treat these conditions regularly. You can even link to their Marketplace and purchase books that go into more detail about pelvic pain.
Many women with pelvic pain have undiagnosed pelvic floor disorders and may also need to see a pelvic floor physical and occupational therapists. Pelvic Guru (https://pelvicguru.com/2016/02/13/find-a-pelvic-health-professional/) created a thorough resource to help people find a the right PT in their area.
I provide all of this information primarily to demonstrate that you’re not alone. There are patients suffering out there just like you. There’s whole societies and associations established to conduct research on these very topics. All you have to do is look.
Get tested.
Before you start the road to recovery, you have to figure out what the problem is first. You need a proper diagnosis because not every woman experiences the same adverse effects of OCPs. Skillful providers will likely need to do a careful evaluation and may need to perform some diagnostic tests. This can include blood tests to measure specific hormones like testosterone, estradiol, and progesterone. A pelvic floor physical and occupational therapy evaluation should also be completed. Your providers will need to take a careful history and learn about when your story started and how it developed.
Once the evaluation and testing is done you should have a diagnosis. Is it pelvic floor dysfunction? Is it a hormonal problem? Is it interstitial cystitis? Maybe it’s all three. The point is you need to have a diagnosis before you can get the right treatment.
Get treatment.
First things first, get off your OCP. I don’t mean to imply you should abandon contraception altogether, but find an alternative. There’s plenty out there. For instance, the American College of Obstetricians and Gynecologists (ACOG) published a Practice Bulletin in 2011 stating: Intrauterine devices (IUDs) and contraceptive implants, also called long-acting reversible contraceptives (LARCs), are the most effective reversible contraceptives (1). So talk to your doctor about LARCs. They are widely under-utilized largely because women aren’t told about them or have heard horror stories that are based on older contraceptive options or are grossly inaccurate. Bottom line: you need to find something else.
Once the OCP is gone, you need to figure out what additional treatment might be needed. As I mentioned just stopping your oral birth control pill will often not resolve the problem completely. Not every woman will need the same treatment, so it’s important that your provider(s) come up with a comprehensive strategy tailor made for you. As I said before, it takes a village. To get better you will likely need a physical and occupational therapists, you might need topical and/or systemic hormonal treatments, you might need a pain specialist, or you might need all of the above. The best and most informed clinicians who work in this field already know this so don’t be surprised if they recommend you see another specialist.
The most important part of starting treatment is to remain patient. You may have been dealing with some of these issues for months, years, even decades. It can be incredibly frustrating, I know. But once you are plugged into the right providers, trust them. These problems likely didn’t occur overnight and won’t get better that quickly either. I reassure my female patients all the time to hang in there. I promise that we will work together and bring in anyone necessary to help fix their problem. You can and will get better with the right village behind you. It just takes time.
Here’s just one example:
Remember CL from the last post? After spending years of not finding answers and coping with continuous vulvar and vestibular pain, she was referred to Pelvic Health and Rehabilitation Center. Thankfully PHRC helped CL address her pelvic floor muscle dysfunction over several months. PHRC asked the right questions, learned of CL’s previous OCP use, and suspected that her issues went beyond the pelvic floor. They astutely referred her to my office for a hormonal work up. CL had improved with physical and occupational therapy, but she still didn’t feel right. After performing my own careful exam and running some standard hormonal blood tests, I diagnosed her with hormonally mediated vestibulodynia. CL was started on systemic testosterone therapy and a local hormonal cream to improve the health of her irritated tissues. She continued with physical and occupational therapy and continues to improve today.
Conclusion.
I did not write this to imply that every woman who ever took an OCP is going to have problems or that every case of vulvodynia stems from OCP use. My point is to suggest that it’s a possibility. We have some data indicating certain pills are worse than others but the risk is always there. With other forms of contraception out there, why are we still so quick to push The Pill? Especially if ACOG has published a bulletin stating that IUDs and other LARCs are more effective anyway. Why aren’t more clinicians discussing the potential risks of vulvar and vestibular pain with women? Certainly if women knew this was a possibility they might think twice about trying an OCP and might ask their physician to suggest an alternative. I hope this blog has been informative and thought provoking and forced you to question the purported “safety” of a medication that is prescribed to millions of women, young and old, every year.
Additional Reading:
In 2015 an International Consensus Conference on Vulvar Pain was held to examine levels of evidence surrounding causes of vulvar pain and associated factors. During this meeting, it was decided that hormonal insufficiencies can cause vulvar pain. The details and resource list have been published in three locations, the references are listed below.
http://www.nva.org/wp-content/uploads/2015/01/2015_ISSVD_ISSWSH_and_IPPS_Consensus_Terminology.2.pdf
http://www.sophiebergeron.ca/images/publications/Pukall_2016_Vulvodynia.pdf
American College of Obstetrics and Gynecology: http://www.sophiebergeron.ca/images/publications/Bornstein_2015_ISSVD.pdf
Resources:
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 121: Long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol. 2011 Jul;118(1):184-96
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.
By Admin
I recently attended a course with pain researcher and clinical neuroscientist, Lorimer Moseley. He, along with his colleague David Butler, have changed the face of pain science and helped many clinicians and patients understand how pain works. If you want to see Lorimer in action, and explain pain better than I ever could, check out his TED talk (https://youtu.be/gwd-wLdIHjs). I’ve synopsized what I found most applicable below. All of this pain education should be attributed to Lorimer Moseley and David Butler and the amazing work they are doing for pain science. I hope this information to be an invitation to understanding your pain better. Let’s start the conversation…
So pain, how would you describe it? It’s horrible, awful, unrelenting, unforgettable- in not the good type of way- it’s pain. What’s its purpose? Well, at it’s base, pain is for survival as a species, to help us learn from our mistakes. That’s why our pain experiences are so memorable. Fool me once snake, shame on me, fool me twice…well you won’t fool me twice. So, basically if our brain detects any possibility of danger or injury to our body, it will produce pain. The purpose of pain is to warn us for a potential for injury- and what an efficient warning system it is. Lorimer recalled a story of his own to explain the effectiveness of this system- perhaps you have a similar story.
One bright morning Lorimer, a native Australian in his native land, was “tramping”, i.e. walking, through the bush, like he had done many mornings before. He was enjoying the scenery, the desert, the rocks, and well, the things of the bush. And, like many times before, he felt a light scratch on his ankle, probably from a twig or something, he thought. It caught his step, but nothing really of note, and he continued on his trek. He visited a nearby swimming hole, took a cool dip, and then turned to return home. And…that’s it…that’s all he remembers. He woke up in the hospital with his leg bandaged, incredulity on his doctors’ faces, and searing leg pain. In actuality, that small “scratch” was no scratch at all, but a snake bike, from the 3rd most deadliest snake in the world! Fortunately when he passed out, he was found by some fellow trampers, carried to the hospital, and quickly given the anti-venom. He soon healed up and learned his lesson, tramping alone in the bush = not the safest idea. So, several years later, he was out again, tramping with some friends. In the midst of talking with a friend, he felt something scratch his ankle. Immediately, searing pain shot up his leg and he crumpled to the ground screaming in agony. Quickly, his companion came to his aid and started organizing how to get him immediate medical attention. Another friend examined his ankle to localize the bite, but to his and Lorimer’s dismay, no bite could be found. A small scratch, similar to something you might get from a twig or something, was all that could be found on his outer left ankle. In the end, that’s all that had happened. A branch had scratched his leg. His brain, the most efficient and effective warning system ever, was prepped to protect, and it did with intense pain. Lorimer, upon recounting the story, was convinced that he even saw a bite mark.
So, what does this mean? Is Lorimer crazy? Some may say yes, but not because of this. This story, and many others, exemplify how pain works. If there is any stimulus the brain determines as dangerous, the brain will protect by all means, with pain, a scream, a fall, even a visual protective response- for self-preservation. The PURPOSE of PAIN is to PROTECT.
A study1 done in 2007 by Moseley and Arntz showed that people given the same very cold (-20 ℃, that’s like -4 ℉) stimulus on the back of their hand along with a blue or red light experienced different levels of pain. Their findings displayed the same protective response. What was the consistent finding? When a participant was shown the blue light with the stimulus he experienced significantly less pain than when that same participate was shown the red light. Interestingly, some participants even reported the cold stimulus as “hot” when shown the red light.
Something even more trippy: do you know what color Viagra is in Italy? Is it blue, like here in the US? No. It’s beige. Do you know why? It all has to do with context. Blue, for most of the world, indicates calm and relaxation, rest and let the parasympathetic nervous system make the magic happen. One researcher found that there were different responses in people based on the color of placebo pill they were given.2,3 Red made the participants heart rate and blood pressure rise. Blue, it dropped. Now, for Viagra, a vasodilator, the last thing you want is a significant rise in heart rate and blood pressure, it kinda defeats the purpose. So, we got our blue pills here in the US. But, in Italy, they got their beige pill. This is because when given to men living in Italy, the blue placebo actually produced an equal rise in blood pressure and heart rate as the red pill. Do you know why? It’s all for the love of soccer: Forza Azzurri! What color is the uniform? Azure, blue. Yep, there is NOTHING more manly in Italy then their soccer team. They even have a national song about it, crushing their enemies and rising victorious. An interesting social experiment, but even more revealing, that our context, experiences, background and beliefs shape us down to our very circulatory and nervous systems. Now Lorimer’s not looking so crazy, is he?
Ok, back to the point of all this-
If our brain is hardwired to protect us, and even just the potential for injury can cause pain, can’t we just turn it off? Well, not exactly. Anyone who has experienced pain knows that you can’t just ignore it to make it go away, not the big pain anyway. Pain is as real as your other protective responses: heart racing, sweating, eye dilating, etc. You can’t just stop sweating, can you? However, what we can do is modify some of the inputs coming in. We can take actions to make our body and brain be more safe. This brings us to the application part of today’s topic. Pain is the output, after our brain decides there are enough danger signals out there to warrant protection.
So, if you are stressed at work, worried about paying off the credit card bills, haven’t slept very well, missed a meal and are moving boxes and feel a “pull” in your back, your brain may just shoot up red flags saying,
Now pain is not this simple, but imagine instead.
You’ve got everything in control at work, savings in the bank, had a good night’s sleep. You just ate a nutritious and delectable meal meal with a close friend and are helping him move boxes. You feel the same “pull” in your back. Your brain may respond differently due to all the the safety signals both circulating in your body and experiencing in your present context. You may feel a twinge, but it will be fleeting, and your brain may say,
This is how we try to look at pain. All aspects of pain. What things make you feel safe: good friends, warm sun on the beach, education on how pain works? What makes you feel unsafe: that MRI picture the doctor told you was the worst he’s ever seen, unsure if you’ll be able to provide for your family, fear you’ll never get better? How can you turn down your danger signals and turn up the safety ones?
So overall, this is plain neuroscience.
PAIN ≠ TISSUE DAMAGE.
PAIN = PROTECTING against POTENTIAL FOR TISSUE DAMAGE.
Understanding this is half the battle.
References:
1) Pain. 2007 Dec 15;133(1-3):64-71. Epub 2007 Apr 20.The context of a noxious stimulus affects the pain it evokes. Moseley GL1, Arntz A.
2) Moerman, DE. (2006), The Meaning Response: Thinking about Placebos. Pain Practice, 6:233-236.
3) Silberman, S. Wired Online. Placebos are getting more effective, drugmakers are desperate to know why. Aug. 29, 2009. Accessed June 27, 2016. http://www.wired.com/2009/08/ff-placebo-effect/?currentPage=all.
FAQ
What are pelvic floor muscles?
The pelvic floor muscles are a group of muscles that run from the coccyx to the pubic bone. They are part of the core, helping to support our entire body as well as providing support for the bowel, bladder and uterus. These muscles help us maintain bowel and bladder control and are involved in sexual pleasure and orgasm. The technical name of the pelvic floor muscles is the Levator Ani muscle group. The pudendal nerve, the levator ani nerve, and branches from the S2 – S4 nerve roots innervate the pelvic floor muscles. They are under voluntary and autonomic control, which is a unique feature only they possess compared to other muscle groups.
What is pelvic floor physical and occupational therapy?
Pelvic floor physical and occupational therapy is a specialized area of physical and occupational therapy. Currently, physical and occupational therapistss need advanced post-graduate education to be able to help people with pelvic floor dysfunction because pelvic floor disorders are not yet being taught in standard physical and occupational therapy curricula. The Pelvic Health and Rehabilitation Center provides extensive training for our staff because we recognize the limitations of physical and occupational therapy education in this unique area.
What happens at pelvic floor therapy?
During an evaluation for pelvic floor dysfunction the physical and occupational therapists will take a detailed history. Following the history the physical and occupational therapists will leave the room to allow the patient to change and drape themselves. The physical and occupational therapists will return to the room and using gloved hands will perform an external and internal manual assessment of the pelvic floor and girdle muscles. The physical and occupational therapists will once again leave the room and allow the patient to dress. Following the manual examination there may also be an examination of strength, motor control, and overall biomechanics and neuromuscular control. The physical and occupational therapists will then communicate the findings to the patient and together with their patient they establish an assessment, short term and long term goals and a treatment plan. Typically people with pelvic floor dysfunction are seen one time per week for one hour for varying amounts of time based on the severity and chronicity of the disease. A home exercise program will be established and the physical and occupational therapists will help coordinate other providers on the treatment team. Typically patients are seen for 3 months to a year.
What is pudendal neuralgia and how is it treated?
Pudendal Neuralgia is a clinical diagnosis that means pain in the sensory distribution of the pudendal nerve. The pudendal nerve is a mixed nerve that exits the S2 – S4 sacral nerve roots, we have a right and left pudendal nerve and each side has three main trunks: the dorsal branch, the perineal branch, and the inferior rectal branch. The branches supply sensation to the clitoris/penis, labia/scrotum, perineum, anus, the distal ⅓ of the urethra and rectum, and the vulva and vestibule. The nerve branches also control the pelvic floor muscles. The pudendal nerve follows a tortuous path through the pelvic floor and girdle, leaving it vulnerable to compression and tension injuries at various points along its path.
Pudendal Neuralgia occurs when the nerve is unable to slide, glide and move normally and as a result, people experience pain in some or all of the above-mentioned areas. Pelvic floor physical and occupational therapy plays a crucial role in identifying the mechanical impairments that are affecting the nerve. The physical and occupational therapy treatment plan is designed to restore normal neural function. Patients with pudendal neuralgia require pelvic floor physical and occupational therapy and may also benefit from medical management that includes pharmaceuticals and procedures such as pudendal nerve blocks or botox injections.
What is interstitial cystitis and how is it treated?
Interstitial Cystitis is a clinical diagnosis characterized by irritative bladder symptoms such as urinary urgency, frequency, and hesitancy in the absence of infection. Research has shown the majority of patients who meet the clinical definition have pelvic floor dysfunction and myalgia. Therefore, the American Urologic Association recommends pelvic floor physical and occupational therapy as first-line treatment for Interstitial Cystitis. Patients will benefit from pelvic floor physical and occupational therapy and may also benefit from pharmacologic management or medical procedures such as bladder instillations.
Who is the Pelvic Health and Rehabilitation Team?
The Pelvic Health and Rehabilitation Center was founded by Elizabeth Akincilar and Stephanie Prendergast in 2006, they have been treating people with pelvic floor disorders since 2001. They were trained and mentored by a medical doctor and quickly became experts in treating pelvic floor disorders. They began creating courses and sharing their knowledge around the world. They expanded to 11 locations in the United States and developed a residency style training program for their employees with ongoing weekly mentoring. The physical and occupational therapistss who work at PHRC have undergone more training than the majority of pelvic floor physical and occupational therapistss and as a result offer efficient and high quality care.
How many years of experience do we have?
Stephanie and Liz have 24 years of experience and help each and every team member become an expert in the field through their training and mentoring program.
Why PHRC versus anyone else?
PHRC is unique because of the specific focus on pelvic floor disorders and the leadership at our company. We are constantly lecturing, teaching, and staying ahead of the curve with our connections to medical experts and emerging experts. As a result, we are able to efficiently and effectively help our patients restore their pelvic health.
Do we treat men for pelvic floor therapy?
The Pelvic Health and Rehabilitation Center is unique in that the Cofounders have always treated people of all genders and therefore have trained the team members and staff the same way. Many pelvic floor physical and occupational therapistss focus solely on people with vulvas, this is not the case here.
Do I need pelvic floor therapy forever?
The majority of people with pelvic floor dysfunction will undergo pelvic floor physical and occupational therapy for a set amount of time based on their goals. Every 6 -8 weeks goals will be re-established based on the physical improvements and remaining physical impairments. Most patients will achieve their goals in 3 – 6 months. If there are complicating medical or untreated comorbidities some patients will be in therapy longer.